L6 Autonomic pharmacology:Adrenergic and Anti-adrenergic Drugs
Objectives
- To understand the pharmacological effects
- The mechanisms of drug action
- Therapeutic applications of alpha and beta adrenergic agonists
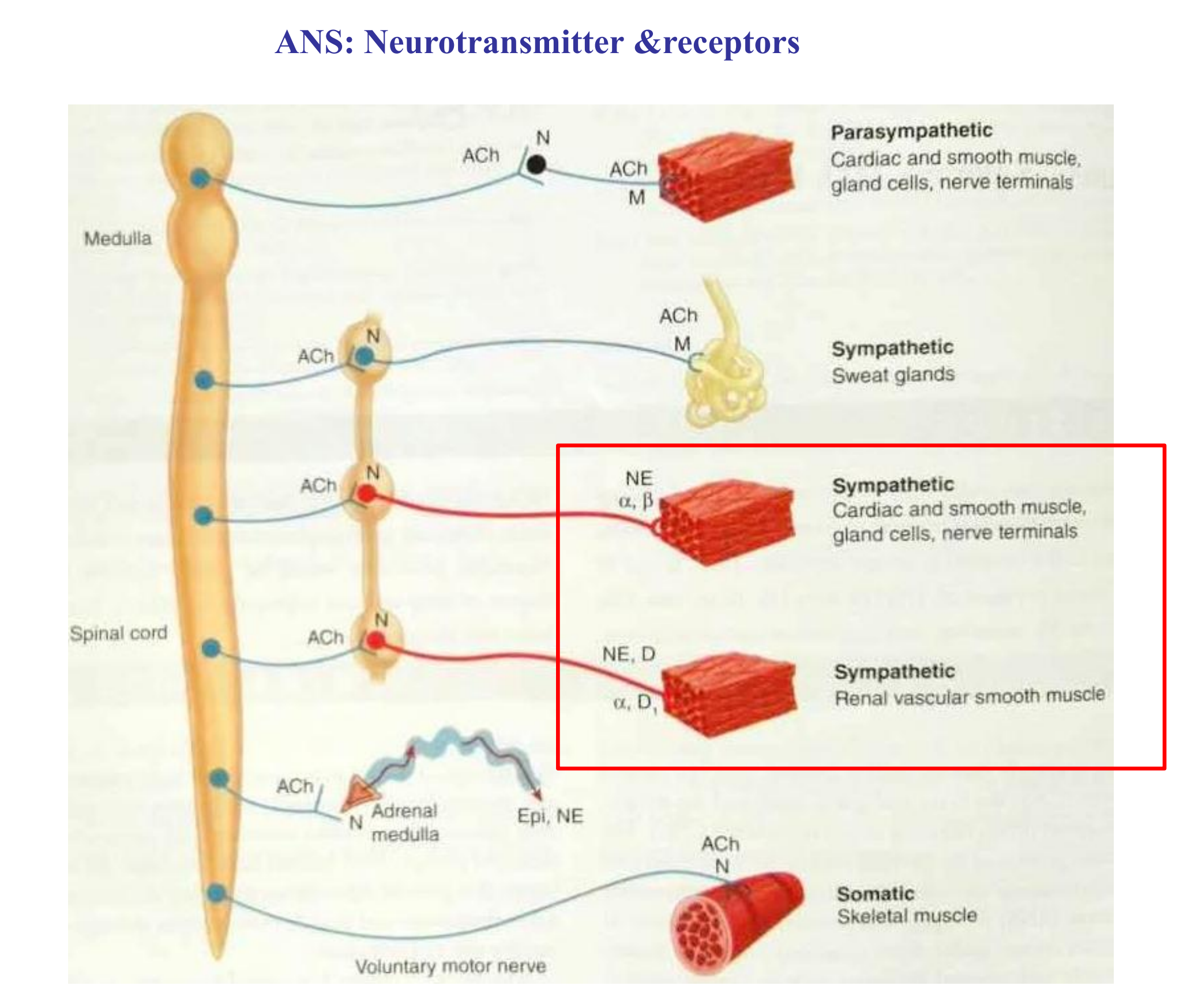
Sympathetic nervous system
Fight or flight response results in:
- Increased BP
- Increased blood flow to brain, heart and skeletal muscles
- Increased muscle glycogenolysis for energy
- Pupil dilation
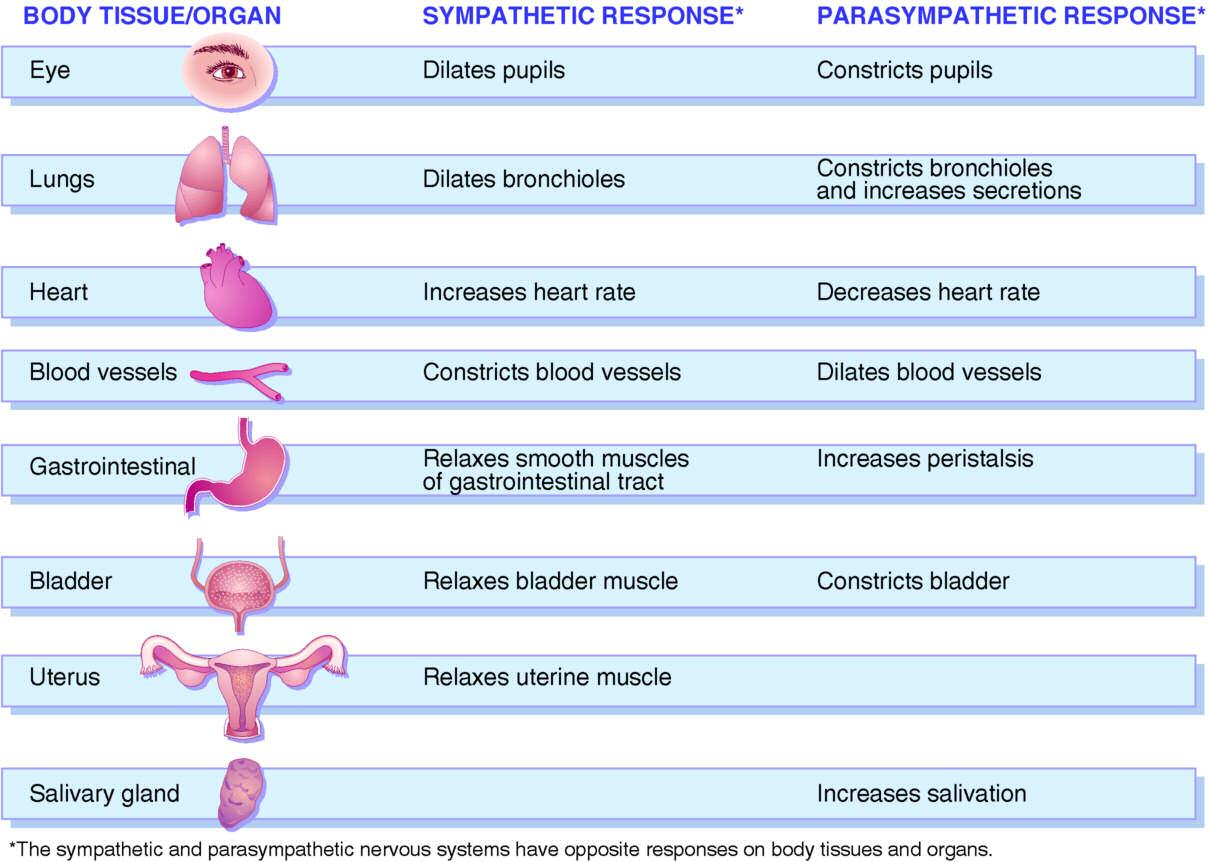
Sympathetic and Parasympathetic Effects on Body Tissues
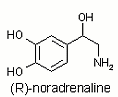
Noradrenaline (NA)
Noradrenaline(NA) or norepinephrine(NE)
- most postganglionic sympathetic fibers (Adrenergic fibers)
1. Noradrenaline VS Adrenaline
Noradrenaline is the main neurotransmitter of the sympathetic nerves in the cardiovascular system.
Adrenaline is the main hormone secreted by the adrenal medulla.
The sympathetic noradrenergic system plays major roles in tonic and reflexive changes in cardiovascular tone.
Adrenaline is a major determinant of responses to metabolic or global challenges to homeostasis.
Adrenaline responses to stressors are more closely linked to responses of the hypothalamic‐pituitary‐adrenocortical system than of the sympathetic nervous system.
The sympathetic noradrenergic system is active even when the individual is at rest and maintains tonic levels of cardiovascular performance.
2. Synthesis of Adrenaline and Noradrenaline
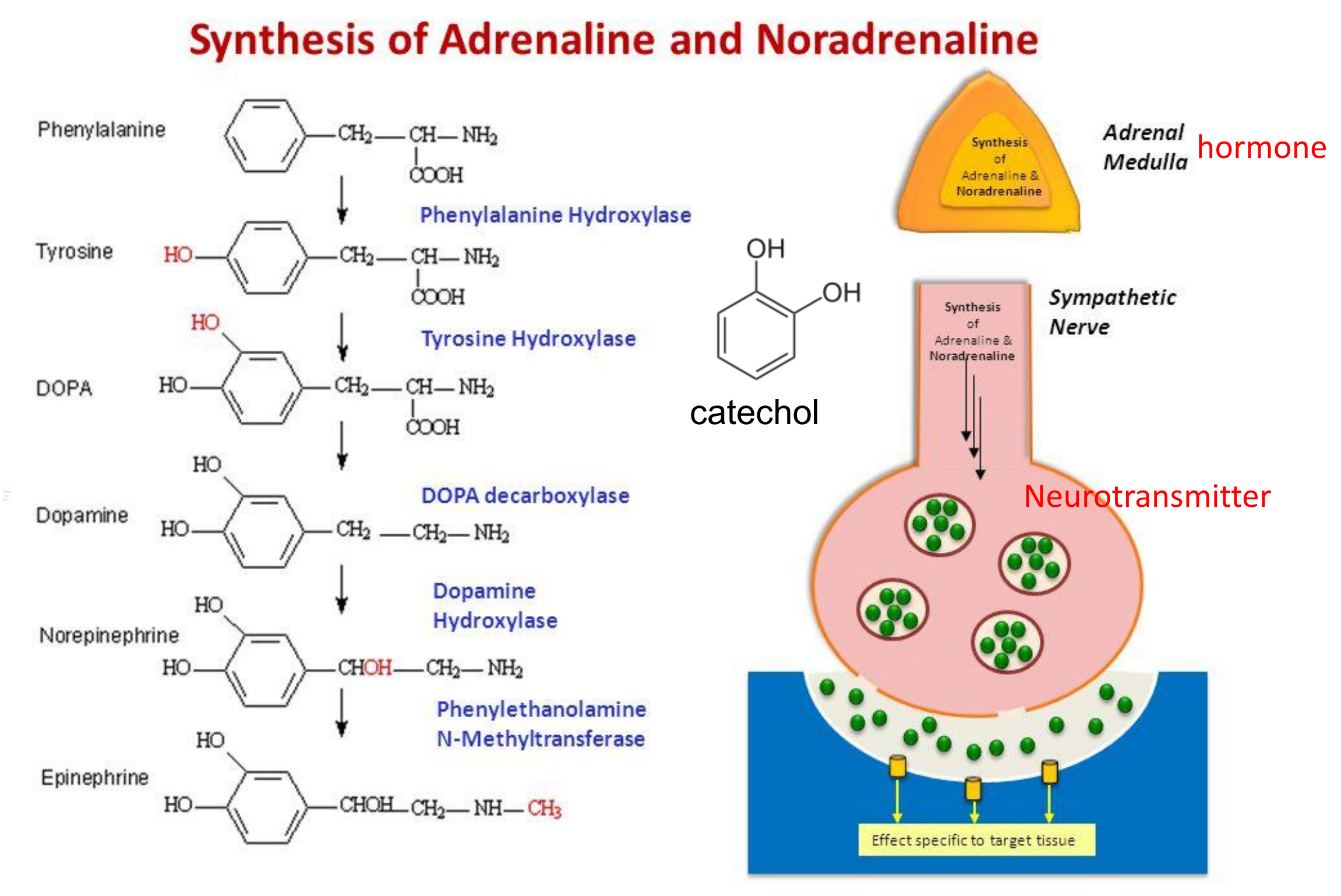
- A catecholamine: an organic compound that has a catechol (benzene with two hydroxyl side groups at carbons 1 and 2) and a side-chain amine
3. NA synapse: synthesis, storage, release and regulation
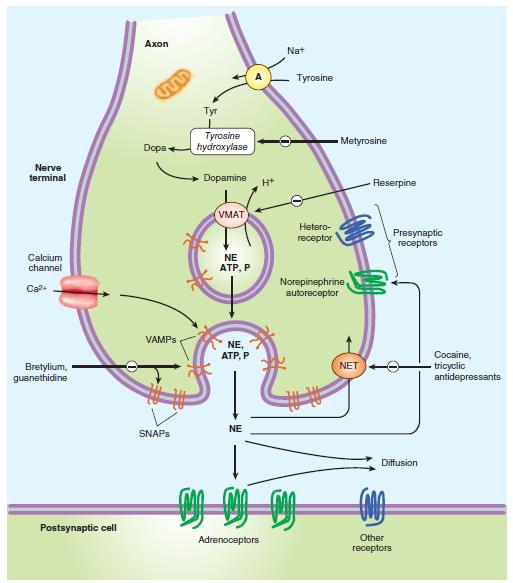
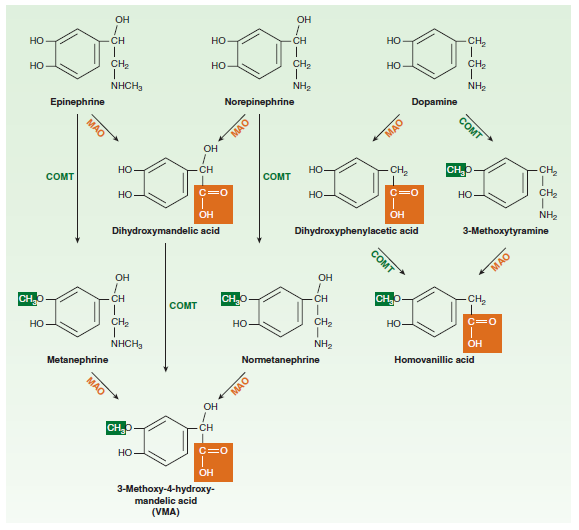
4. Norepinephrine degradation
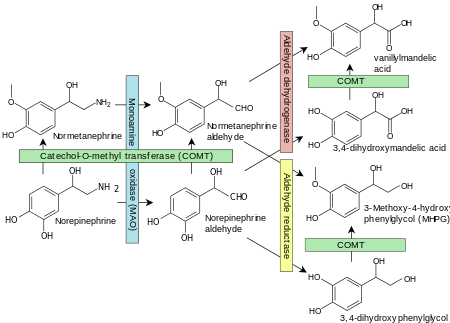
- COMT is found in the gut and liver, so catecholamines are not active orally
5. Metabolism of NA
Norepinephrine transporter targeted by amphetamine and cocaine
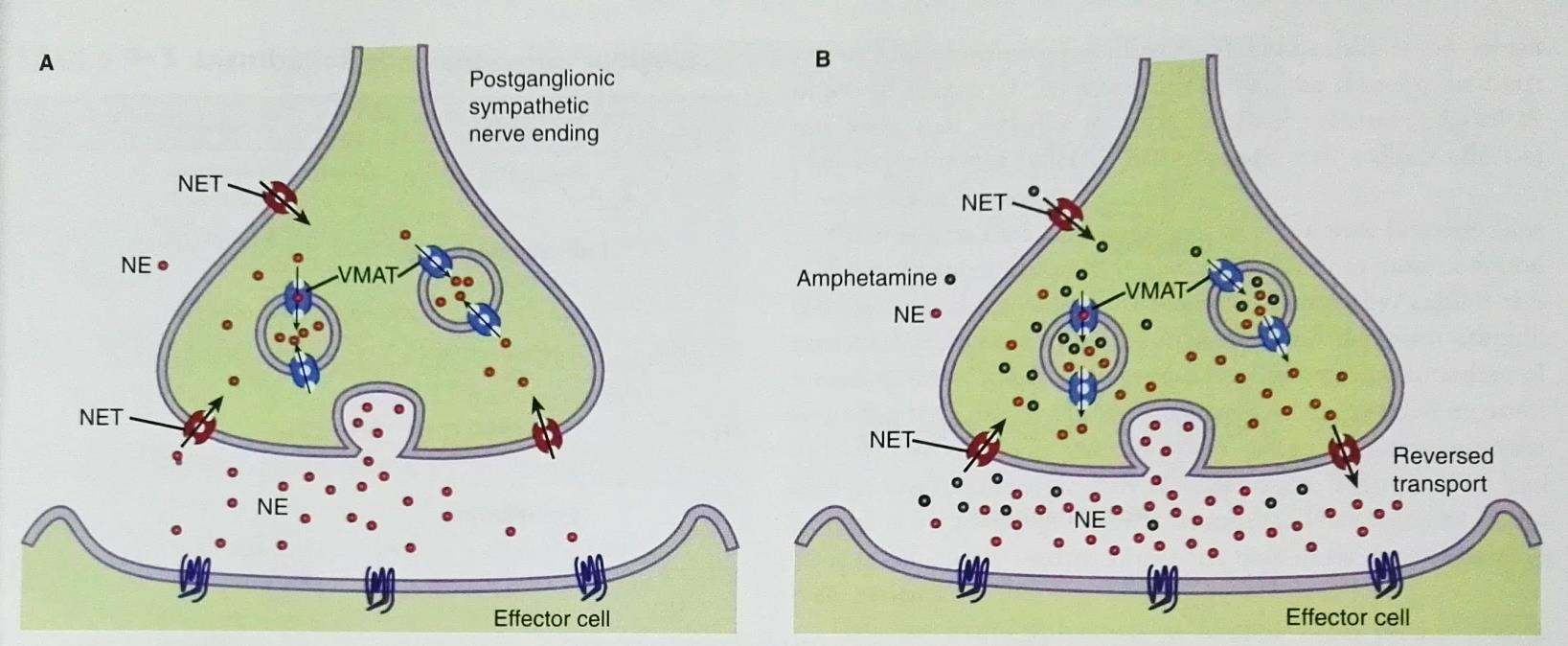
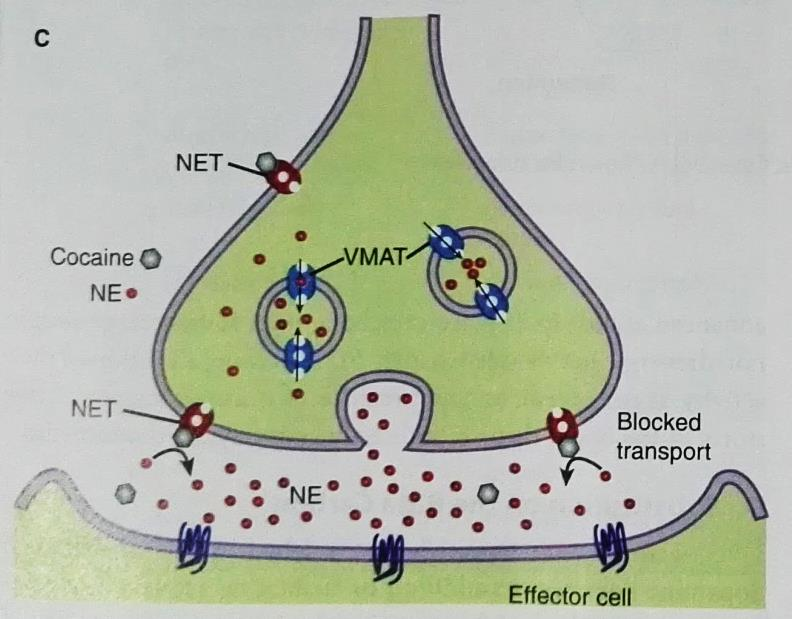
- amphetamine is a competitive antagonist,competitively binds the receptor
- cocaine is noncompetitive antagonist,inhibit the receptor
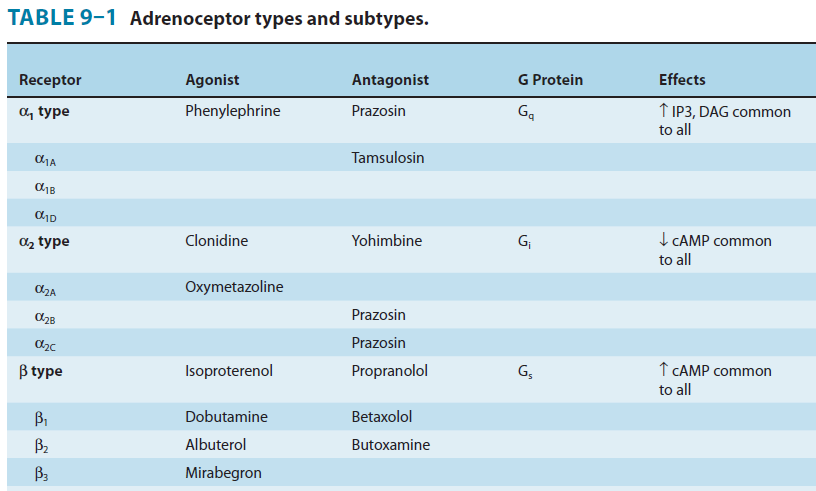
Adrenoceptors
Adrenoceptors in the membranes of effector cells determine the physiological and metabolic effects of catecholamines.
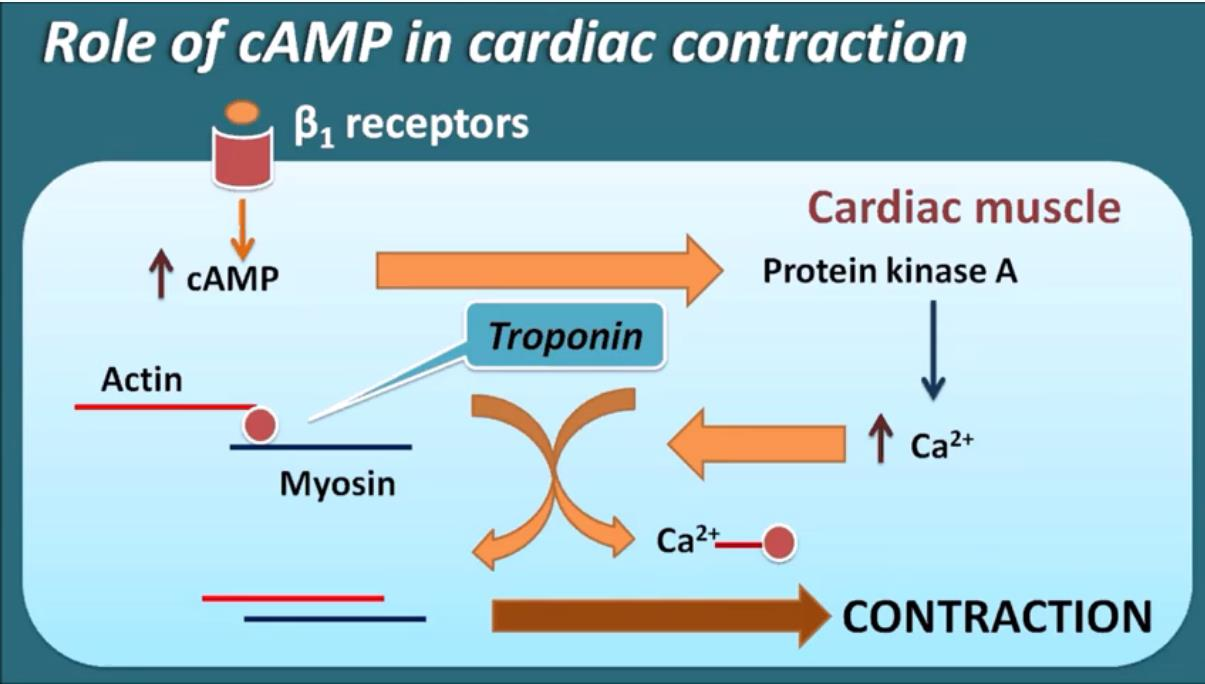
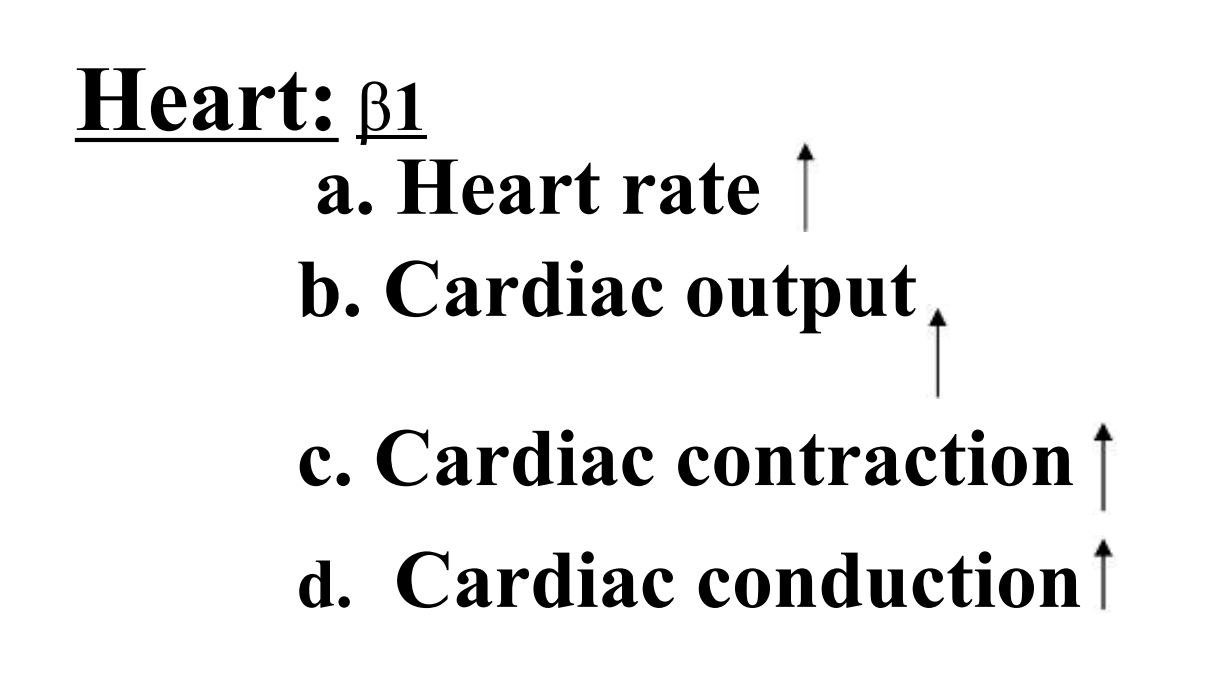
Beta‐adrenoceptors mediate stimulatory effects of catecholamines on the rate and force of the heartbeat;
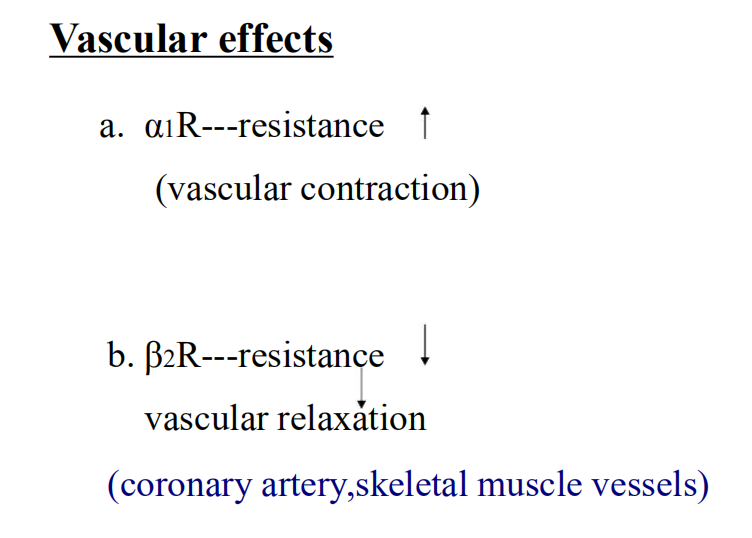
stimulation of vascular alpha‐adrenoceptors produces vasoconstriction and increases blood pressure, and stimulation of vascular beta‐adrenoceptors – especially beta‐2 adrenoceptors in skeletal muscle – produces vasodilation.
Catecholamines affect cardiovascular functions by actions at adrenoceptors on cardiovascular cells, in the nervous system,and in the kidneys
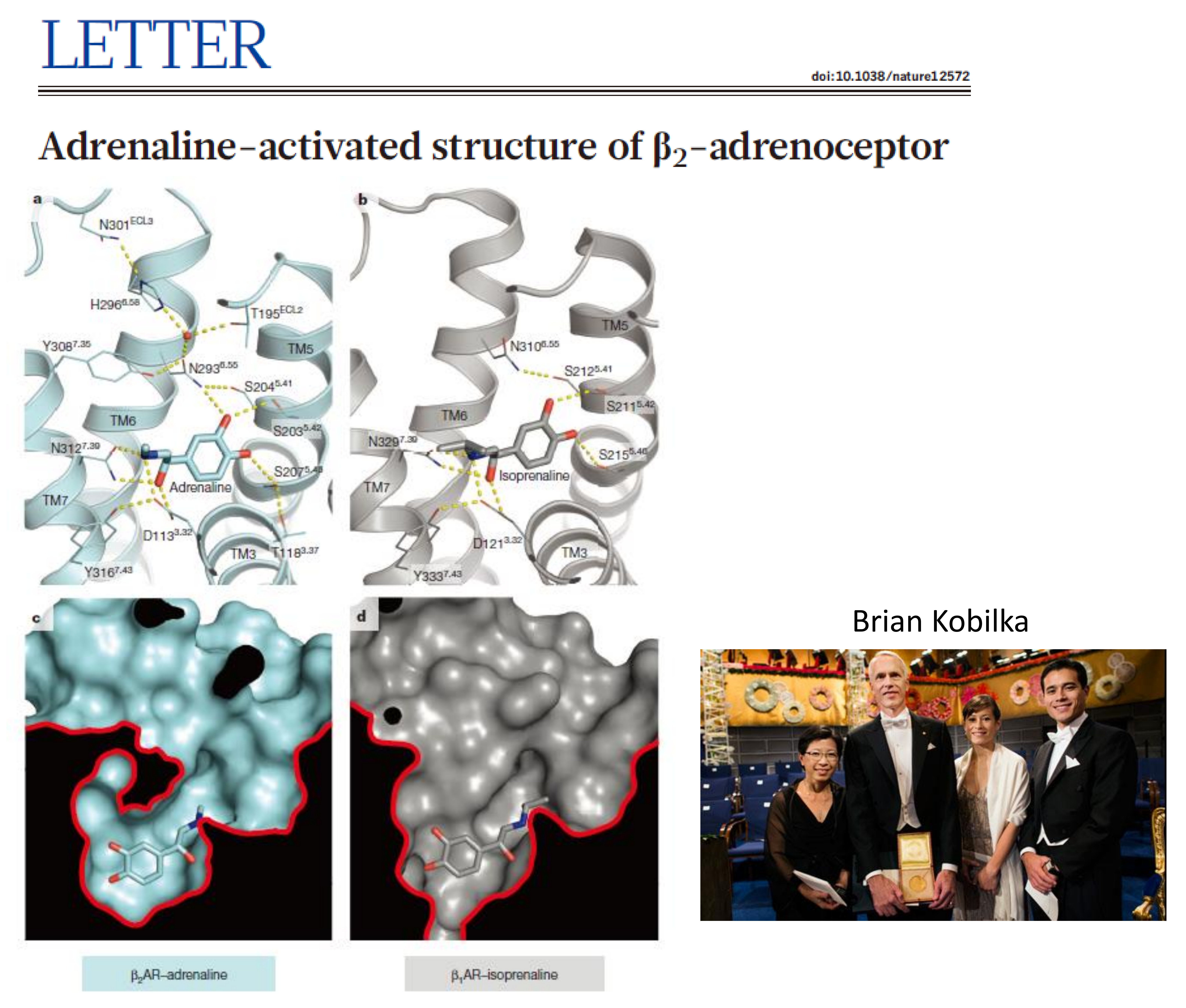
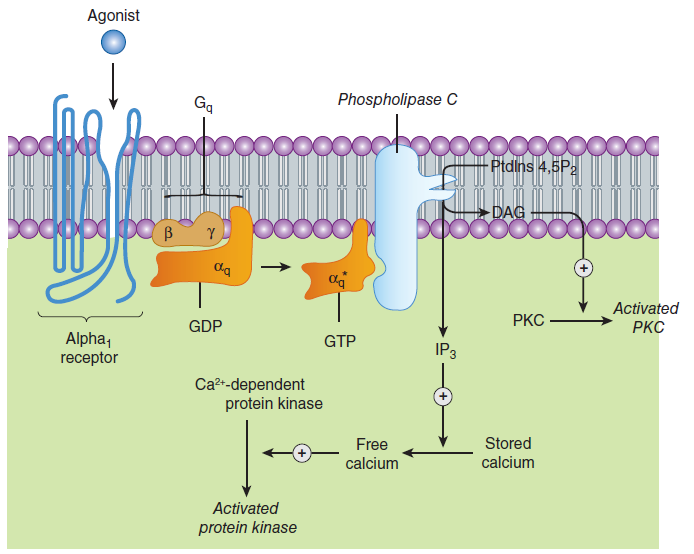
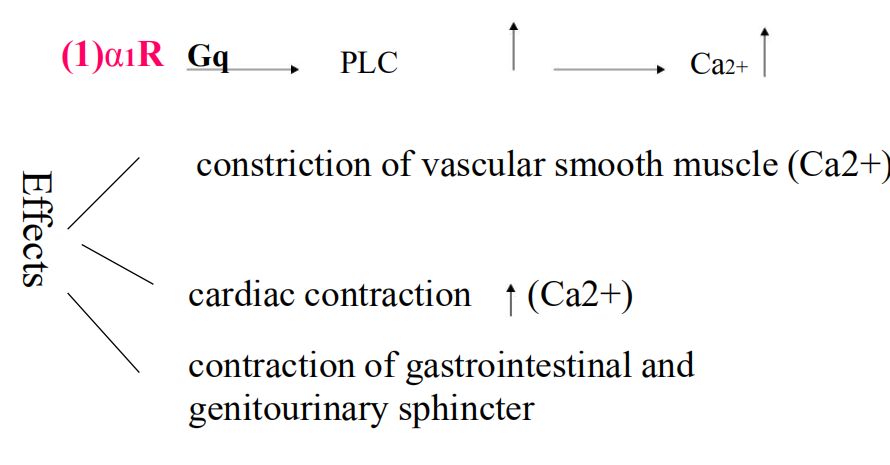
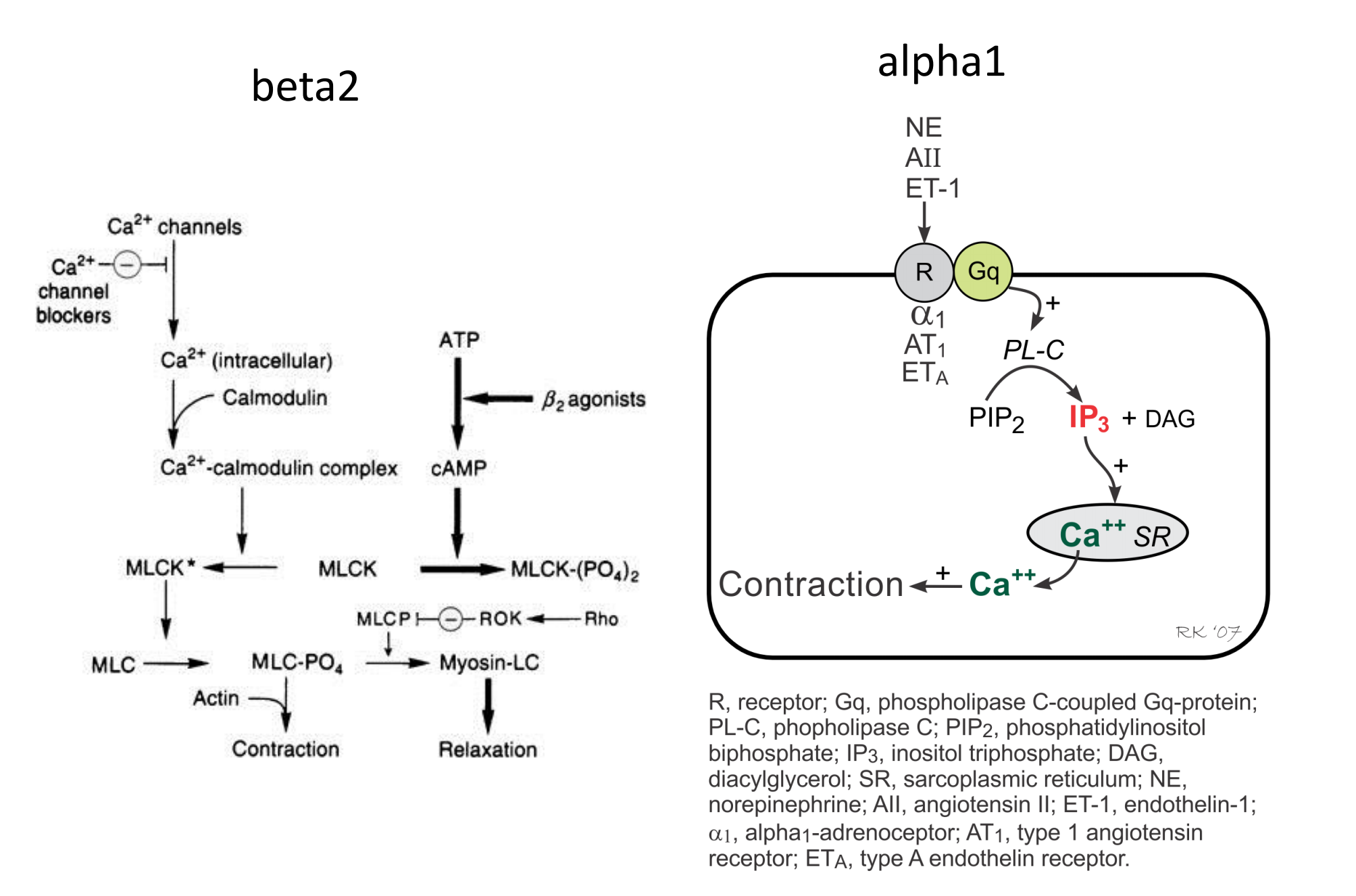
1. Signaling pathway of α1 receptor activation
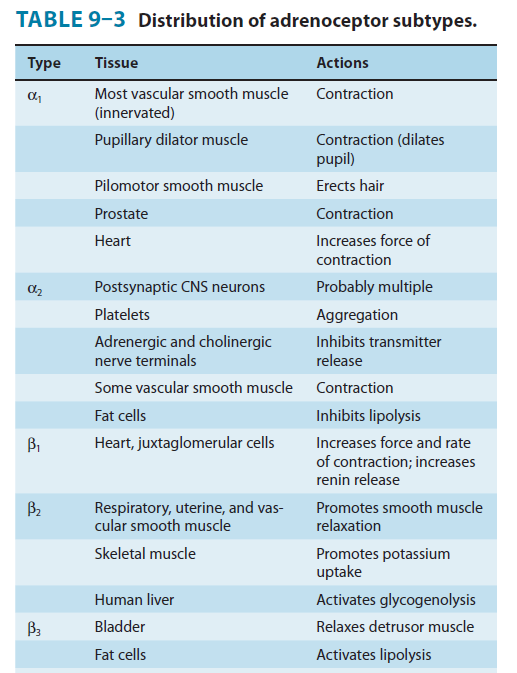
- α receptor: α1, α2
- β receptor: β1,β2,β3
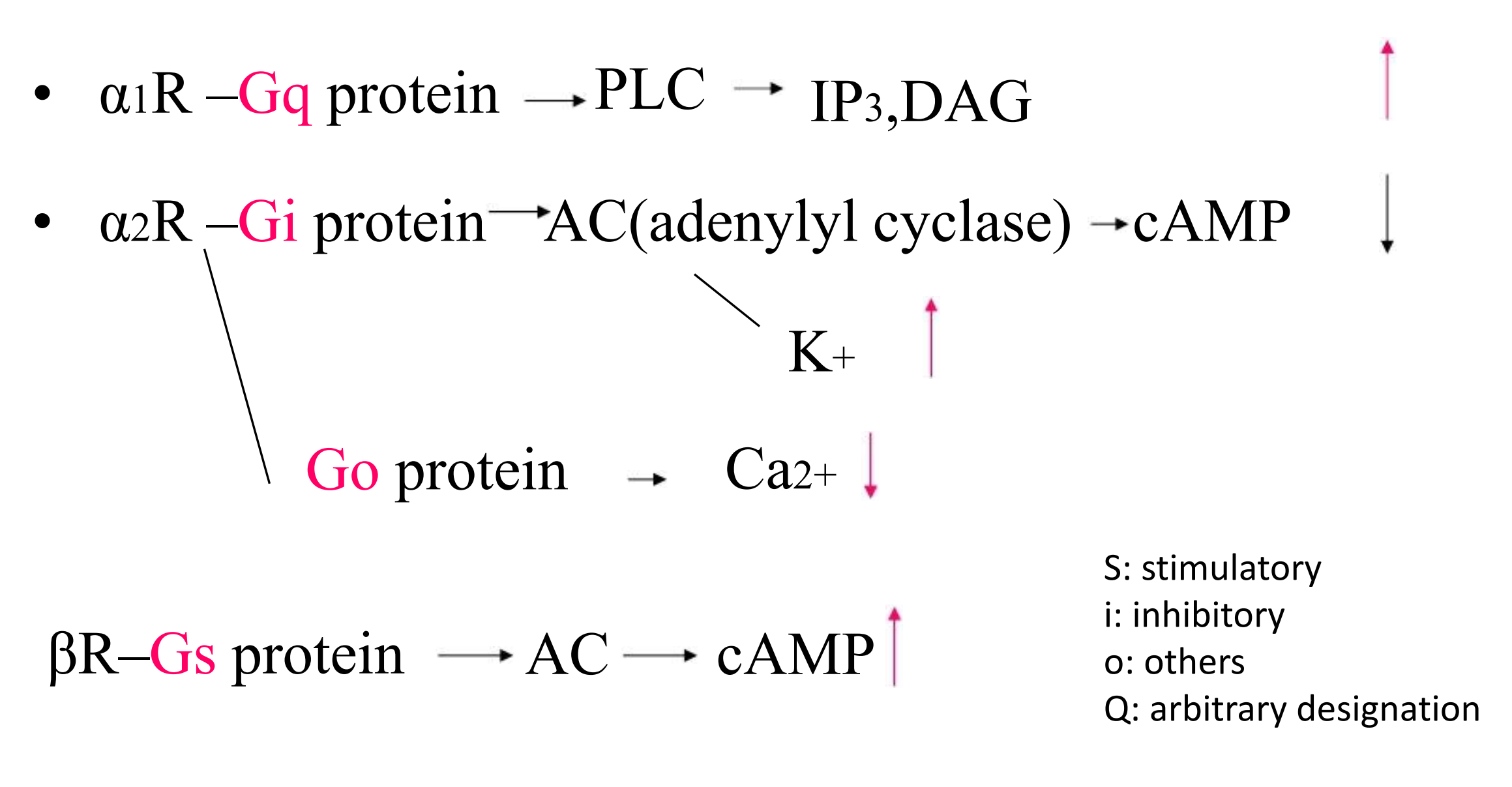
2. Signaling pathway of β and α2 receptor
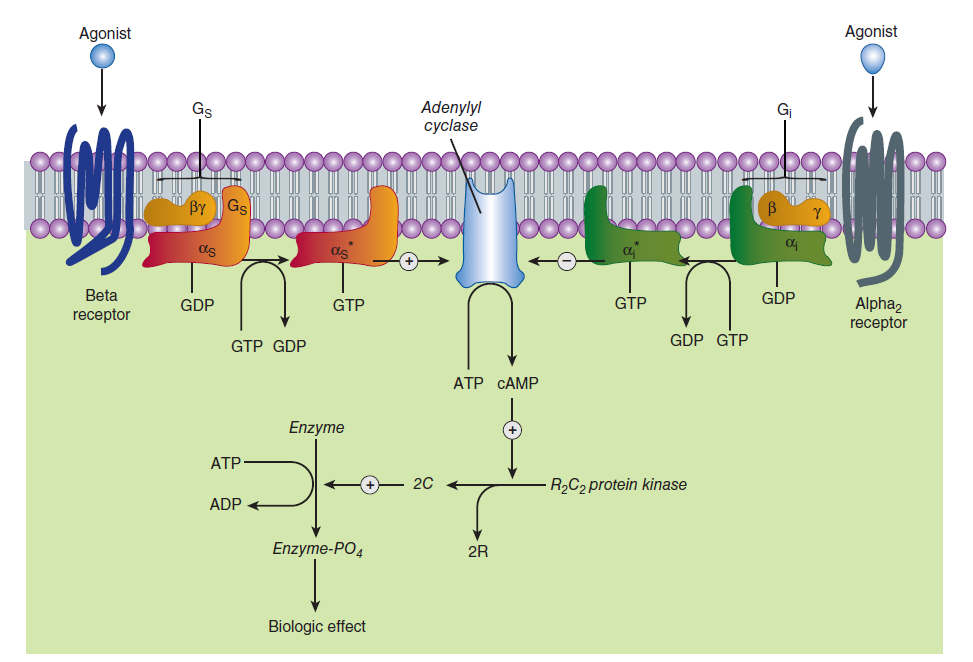
3. Adrenoceptors: signaling
Sympathetic Responses
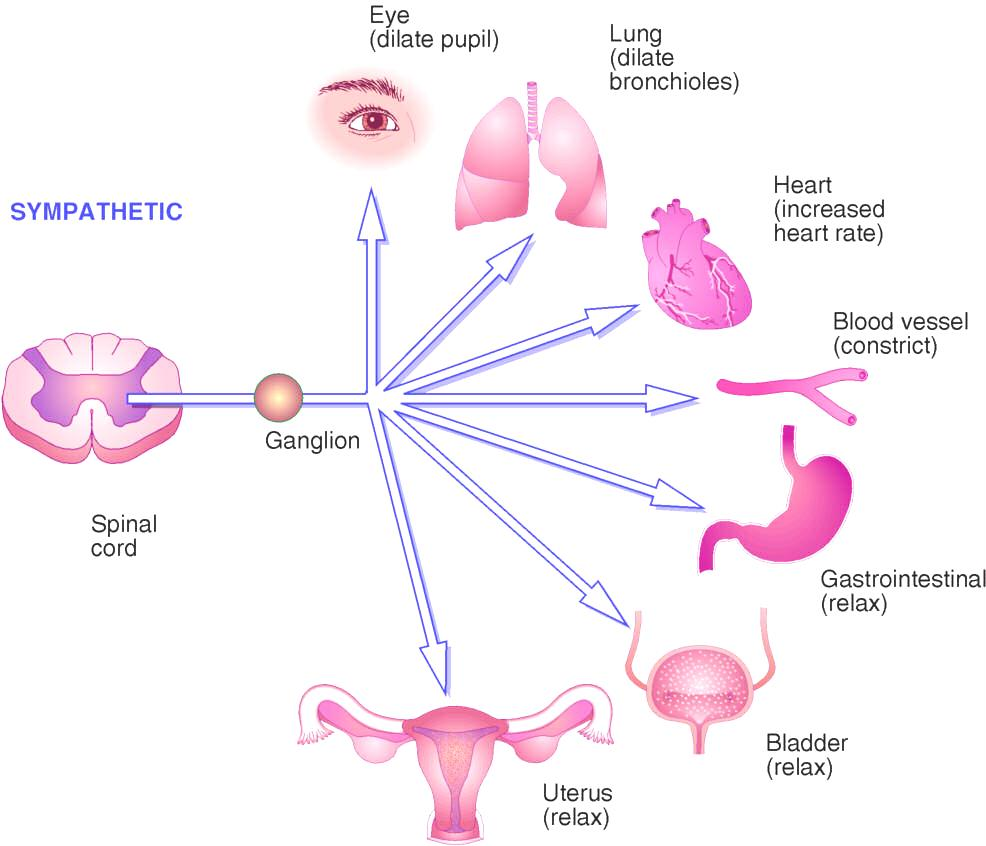
Stimulation
1. Effects of stimulation of α1 adrenergic receptors
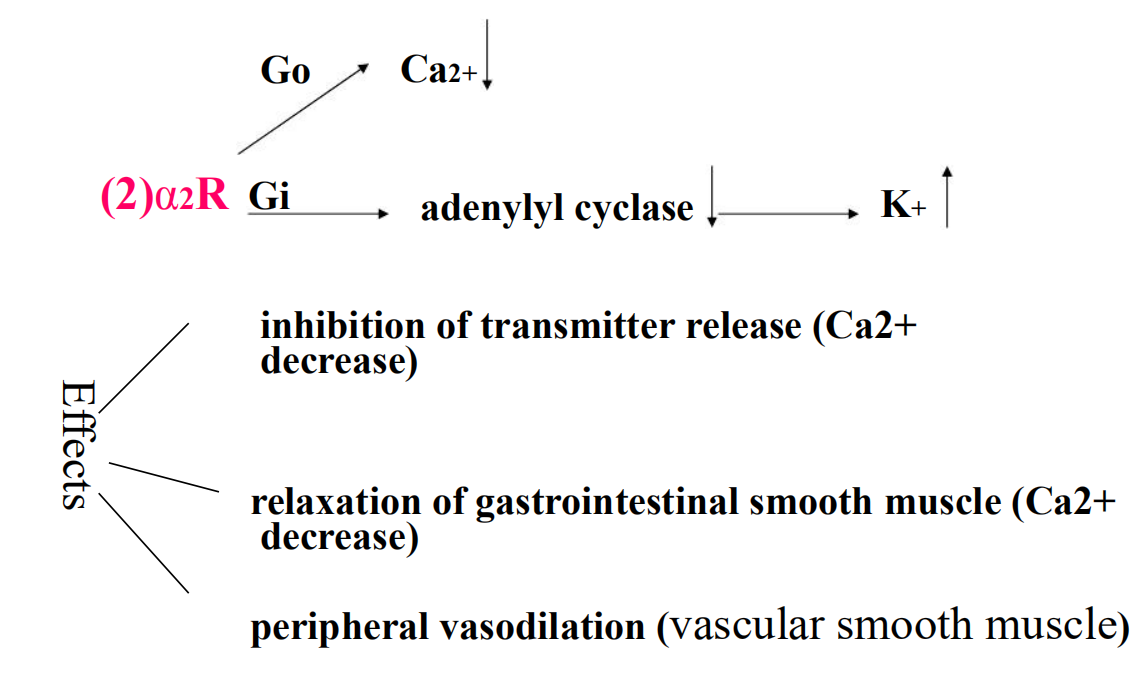
2. Effects of stimulation of α2 adrenergic receptors
3. Effects of stimulation of β–adrenergic receptors
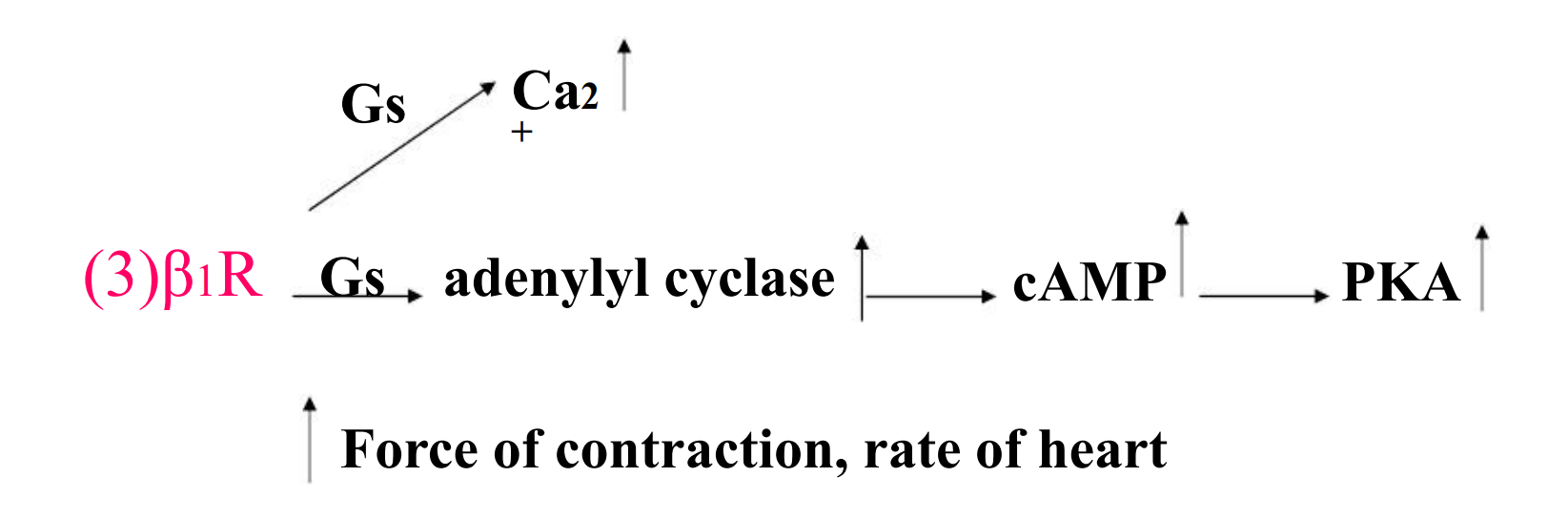
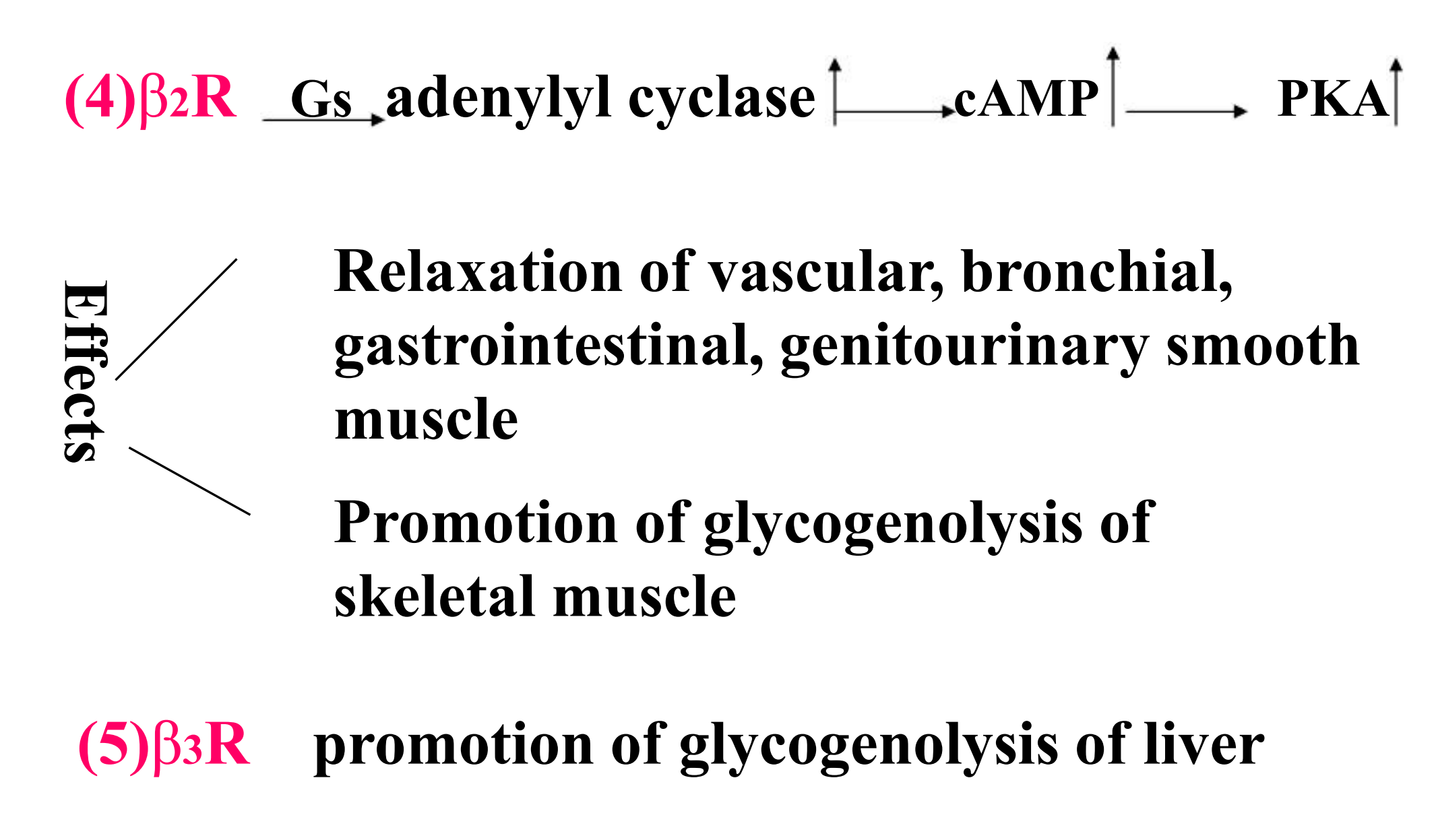
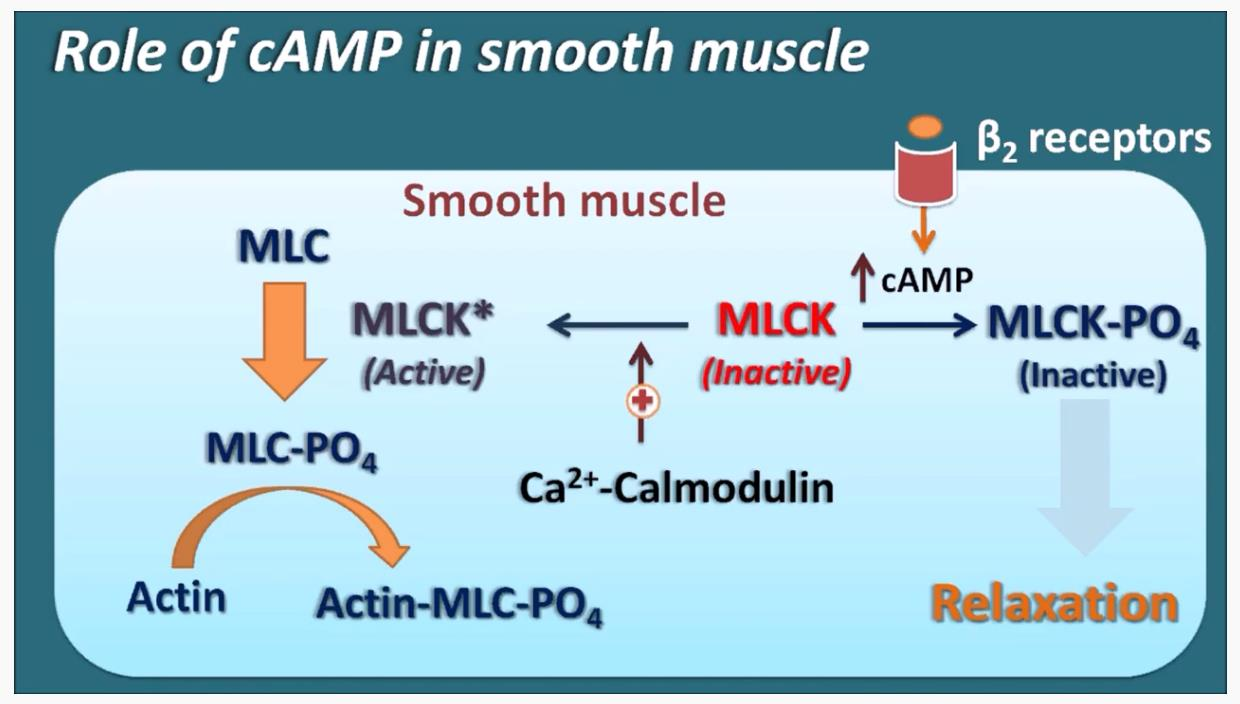
4. Different role of cAMP in Smooth and Cardiac Muscles
Review of functions of sympathetic nervous system receptors
Alpha 1—smooth muscle contraction
Alpha 2-negative feedback causes less norepinephrine to be released so BP is
reduced
Beta 1—increased heart rate
Beta 2—bronchodilation
Beta 3—actual site for lipolysis
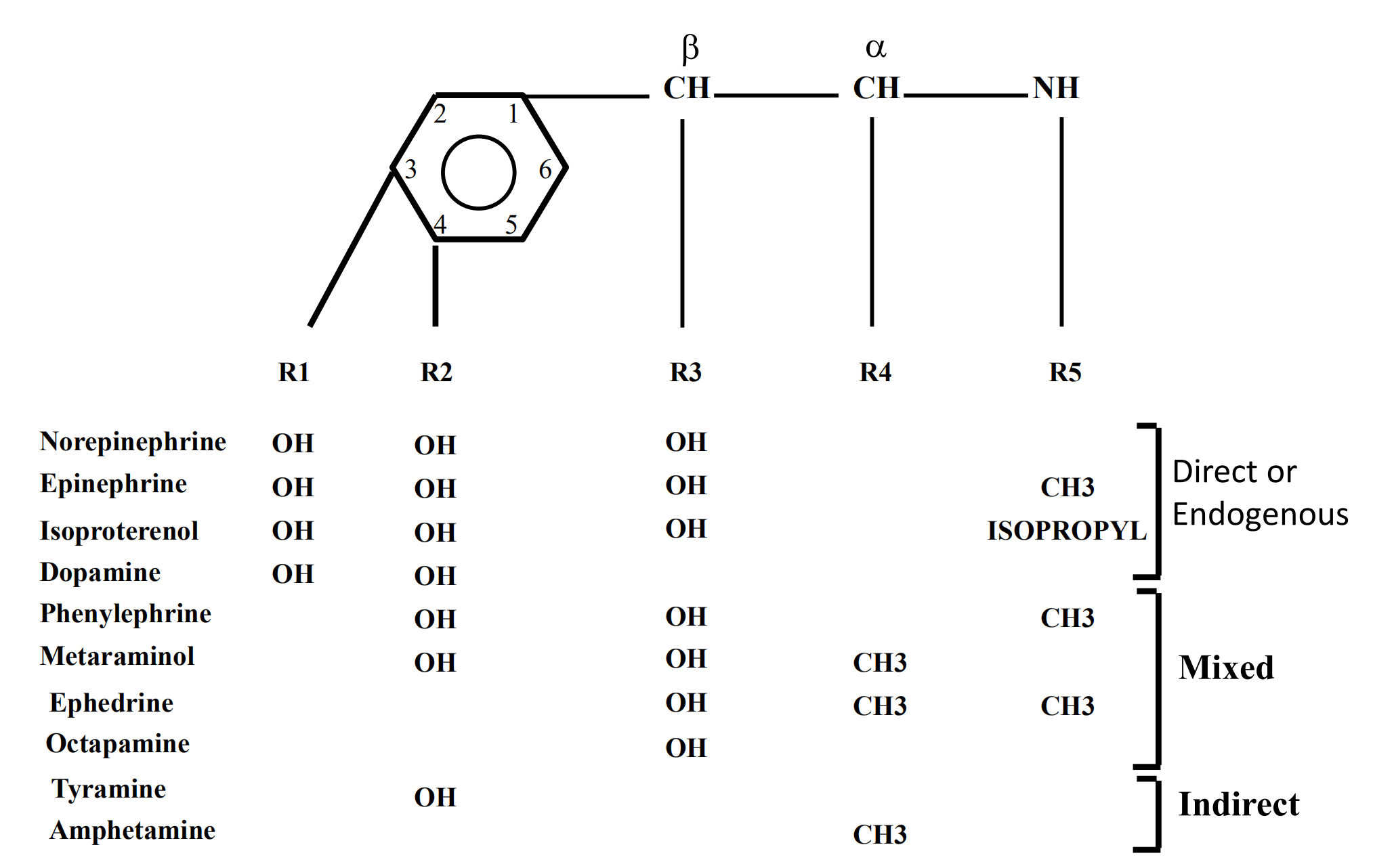
1. Adrenoceptor Activating Drugs And Other Sympathomimetics
Sympathomimetics are drugs that partially or completely mimic the action of Epinephrine (E) Or Norepinephrine (NE)
- Directly – acts on adrenergic receptor
- Indirectly – stimulates the release Catecholamines (CA) from nerve ending
Classifications: the endogenous biogenic amines (NE, E, DA, ISO)
- ephedrine and other vasocontractors
- bronchodilators
- CNS stimulants
Their effects can be predicted from the knowledge of:
- The type of adrenergic receptor
- Property for penetration into CNS
- Receptor selectivity
Pharmacological responses of α and β–R agonists
1. Cardiovascular system
2. Eye
Mydriasis (radial pupillary dilator muscle of iris contains → receptors, → stimulation → muscle contraction → pupil dilation)
3. Respiratory tract
Bronchial smooth muscle: ß2 receptor → relaxation → bronchodilation
Upper respiratory tract mucosa: → receptors; → stimulants → decongestion
4. Gastrointestinal tract
Both α and ß stimulants induce the relaxation of GIT smooth muscle
ß receptor activation (smooth muscle cells) → hyperpolarization → relaxation
α stimulants act indirectly; reduce presynaptically the release of acetylcholine
5. Genitourinary tract
Human uterus (α and ß receptors). ß2 receptor stimulation → relaxation
Bladder base and urethral sphincter: α receptor → contraction → continence
Bladder wall: ß2 receptors → relaxation
Ejaculation is dependent upon normal α receptor activity
6. Exocrine glands
Salivary gland: increased secretion (mucinous rich saliva,)
Apocrine sweat gland (eg. palms of hands): α stimulants → sweat production ↑
7. Metabolic effects
Fat cells: ß3 receptor activation → increased lipolysis
Lipocytes: α receptor activation → inhibited lipolysis
Liver: ß2 & α1 receptor activation → glycogenolysis → blood glucose ↑
Skeletal muscle: ß1 receptor activation → glycogenolysis → lactate ↑
8. Endocrine function
Insulin secretion is stimulated by ß1 and inhibited by α2 stimulation
Renin secretion is stimulated by ß1 and inhibited by α2 receptors
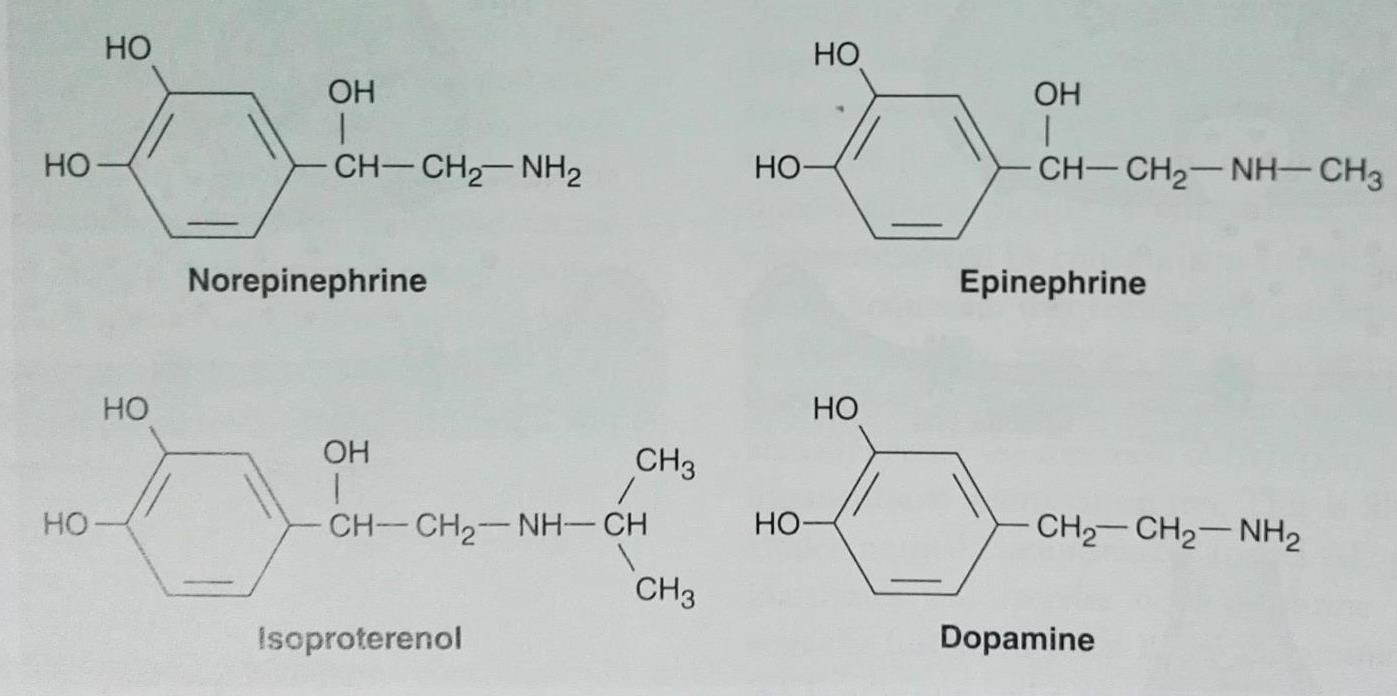
Endogenous catecholamines: - norepinephrine, epinephrine, dopamine
Synthetic catecholamines: - isoproterenol
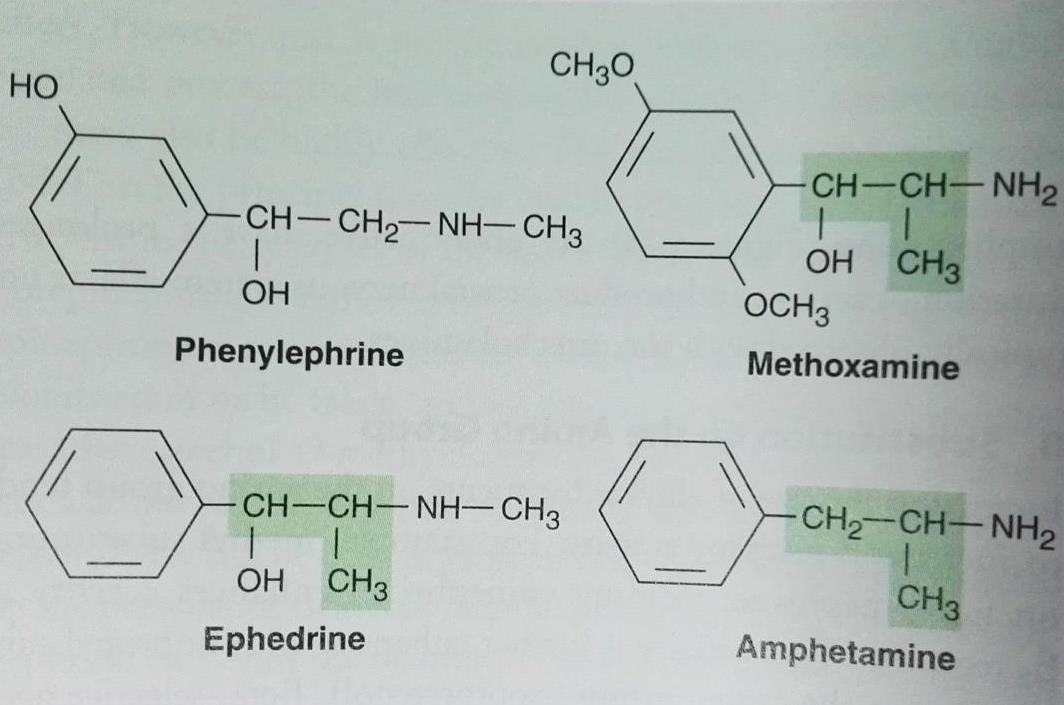
Substitutions:
On the amino group
- Increasing the size of the alkyl group → increased ß and decreased α activity
On the benzene ring
- Maximal α and ß activity is found with CAs (R1 and R2 = OH)
- Absence of one or two -OH increases bioavailability
- Absence of -OH groups increases lipid solubility (potential CNS effects)
On the α carbon
- Substitution blocks the oxydation by MAO and prolongs the action
On the β carbon
- Mostly hydroxyl except Dopamine; facilitates receptor activation and for storage in neural vesicles
Specific Sympathomimetic Drugs
Catecholamines Epinephrine (E, Adrenaline)
Acts on both α and ß receptors(low concentration -ß effects, high dose - α effect dominated
1. Effects on blood pressure
Low doses of E: BP ↓ (ß2 receptor stimulation → Vasodilatation, cAMP effect on endothelium)
Large doses of E: BP ↑ (α receptor stimulation → Vasoconstriction, Ca2+ effect on muscle)
Norepinephrine (NE, Noradrenaline)
NE is almost equipotent with E on ß1and α receptors but with little effect on ß2 receptors
1. Pharmacokinetics of Epinephrine and Norepinephrine
Poor absorption following oral administration (rapid conjugation and oxydation)
Slow absorption following subcutaneous administration → local vasoconstriction
Inhaled solutions are used in the disease of respiratory tract
They can be given intravenously
Metabolism in the liver (COMT and MAO); excretion in the urine
2. Chemistry and pharmacokinetics
Catecholamines:
Noncatecholamines:
- Ephedrine: from TCM, 麻黄
Non-Catecholamines
1. Phenylephrine
Pure α receptor agonist, with long duration of action (not inactivated by COMT)
- Direct acting sympathomimetic, its effects are similar to those of NE but less potent
- Vasoconstriction, BP ↑, reflex bradycardia occurs after parenteral administration
Therapeutic uses
nasal decongestant (endothelium less dilated)
local vasoconstrictor
- as 10 % ophthalmic solution
- as an adjunct for use of LA
for relief of paroxysmal atrial tachycardia
Adverse effects
Large doses → ventricular arrhythmias (eg. after systemic absorbtion)
Rebound nasal congestion may occur after chronic use
Anti-adrenergic Drugs
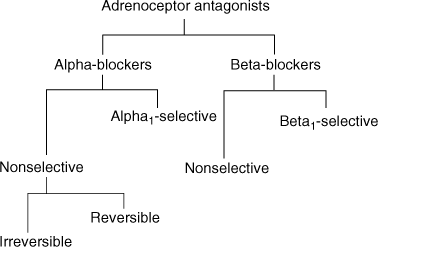
Classification
- α-Adrenoceptor Antagonists (α adrenergic bolckers)
- β- Adrenoceptor Antagonists (β adrenergic bolckers)
- α,β- Adrenoceptor Antagonists (mixed α,β adrenergic bolckers)
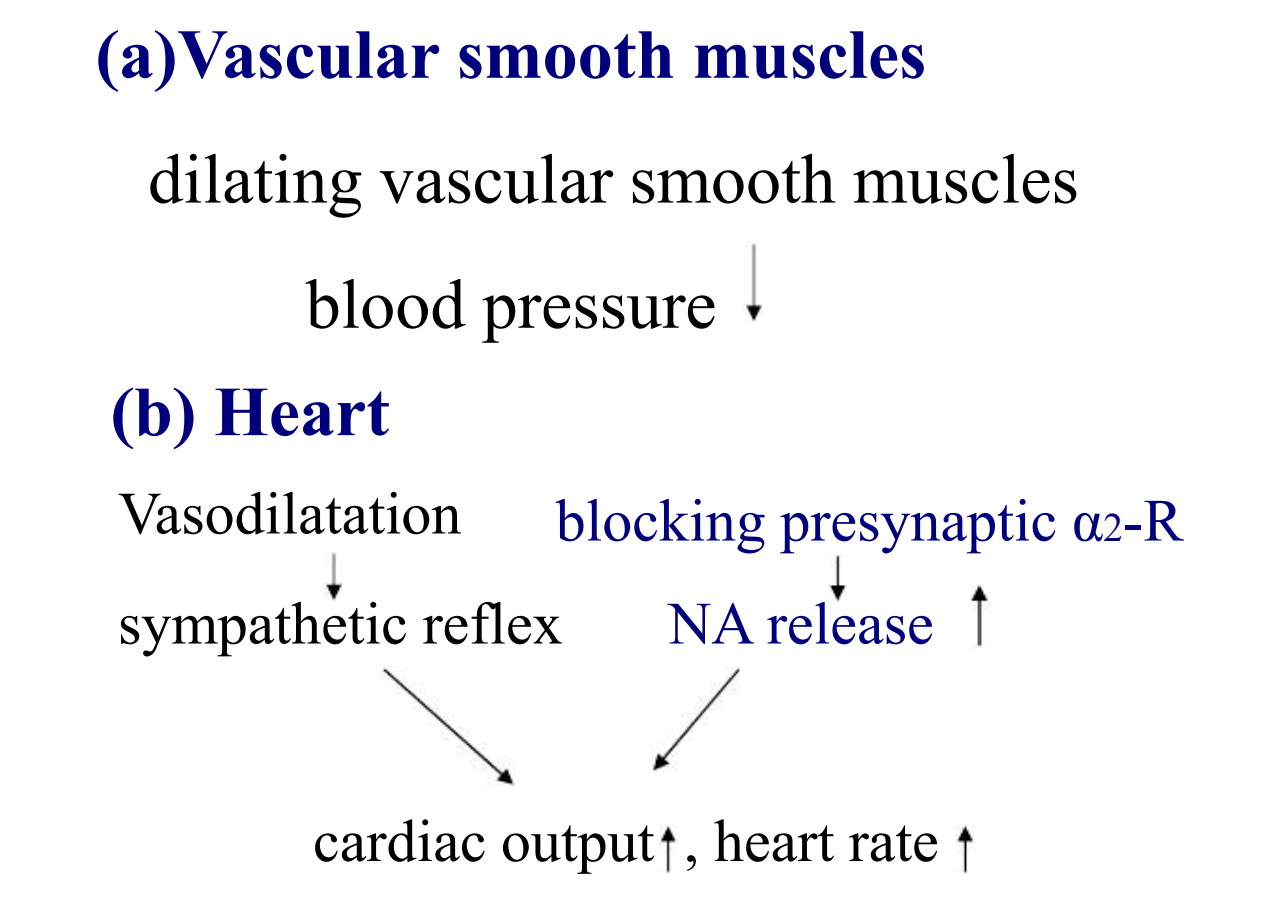
Pharmacological effects
1. blocking α1-R effects
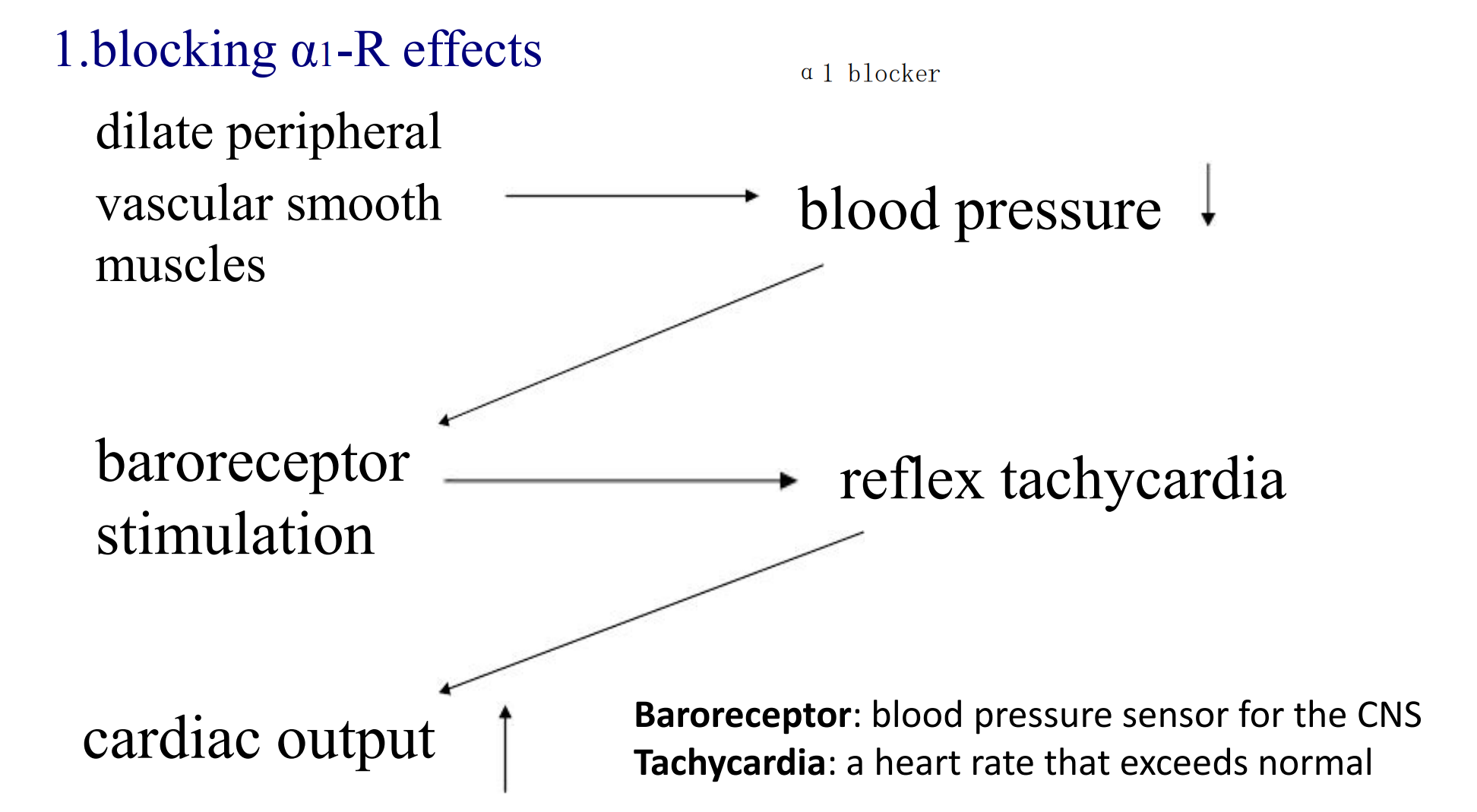
2. Blocking α2-R effects
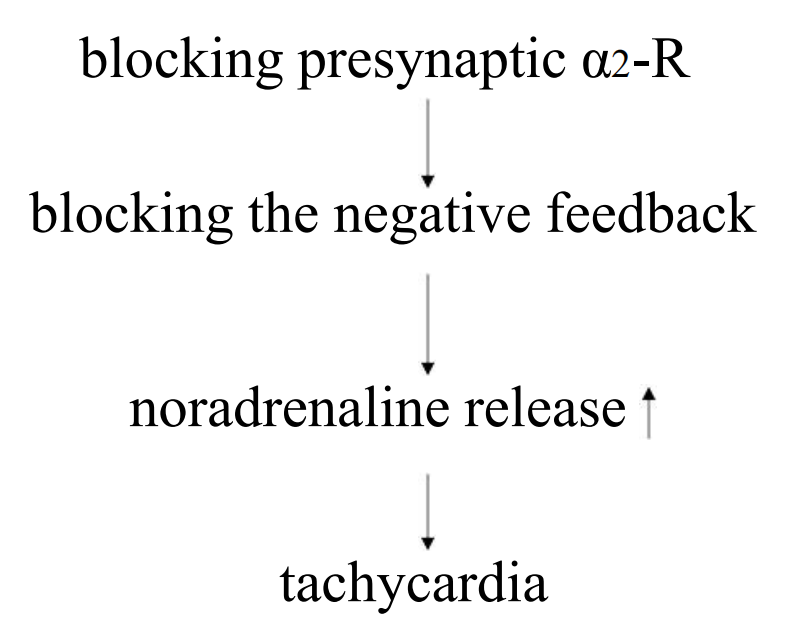
- block α2 will increase heart rate, because block the negative feedback
- α2 exixts on the presynaptic surface, end up with lots of NA
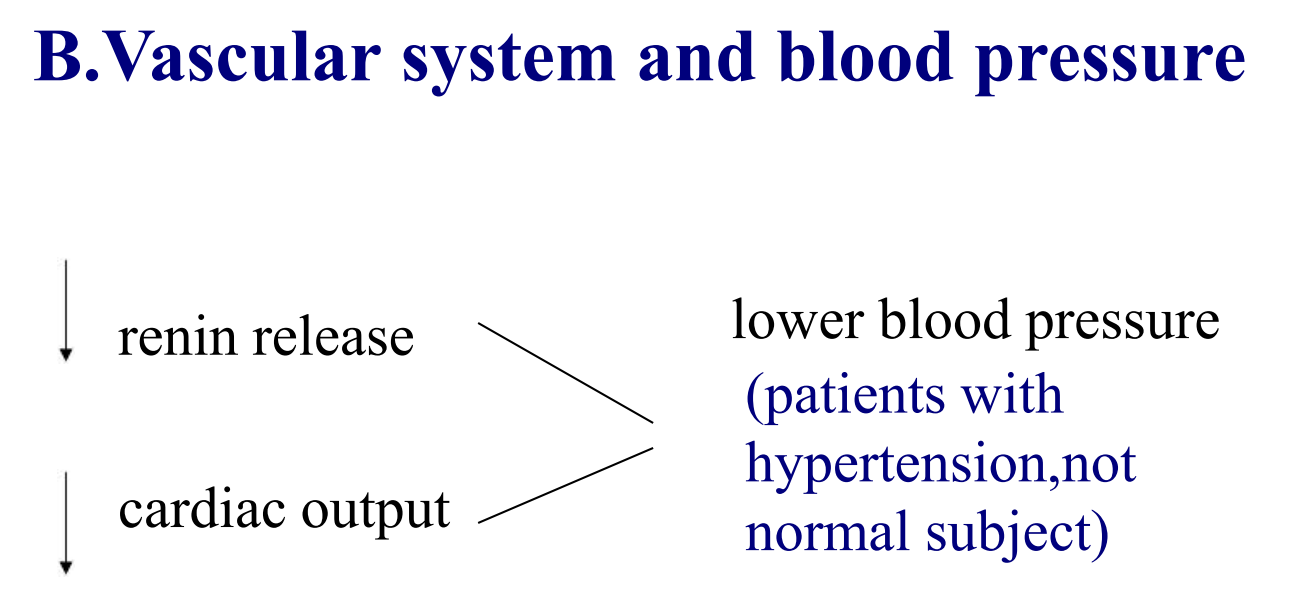
3. blocking β1-R effects
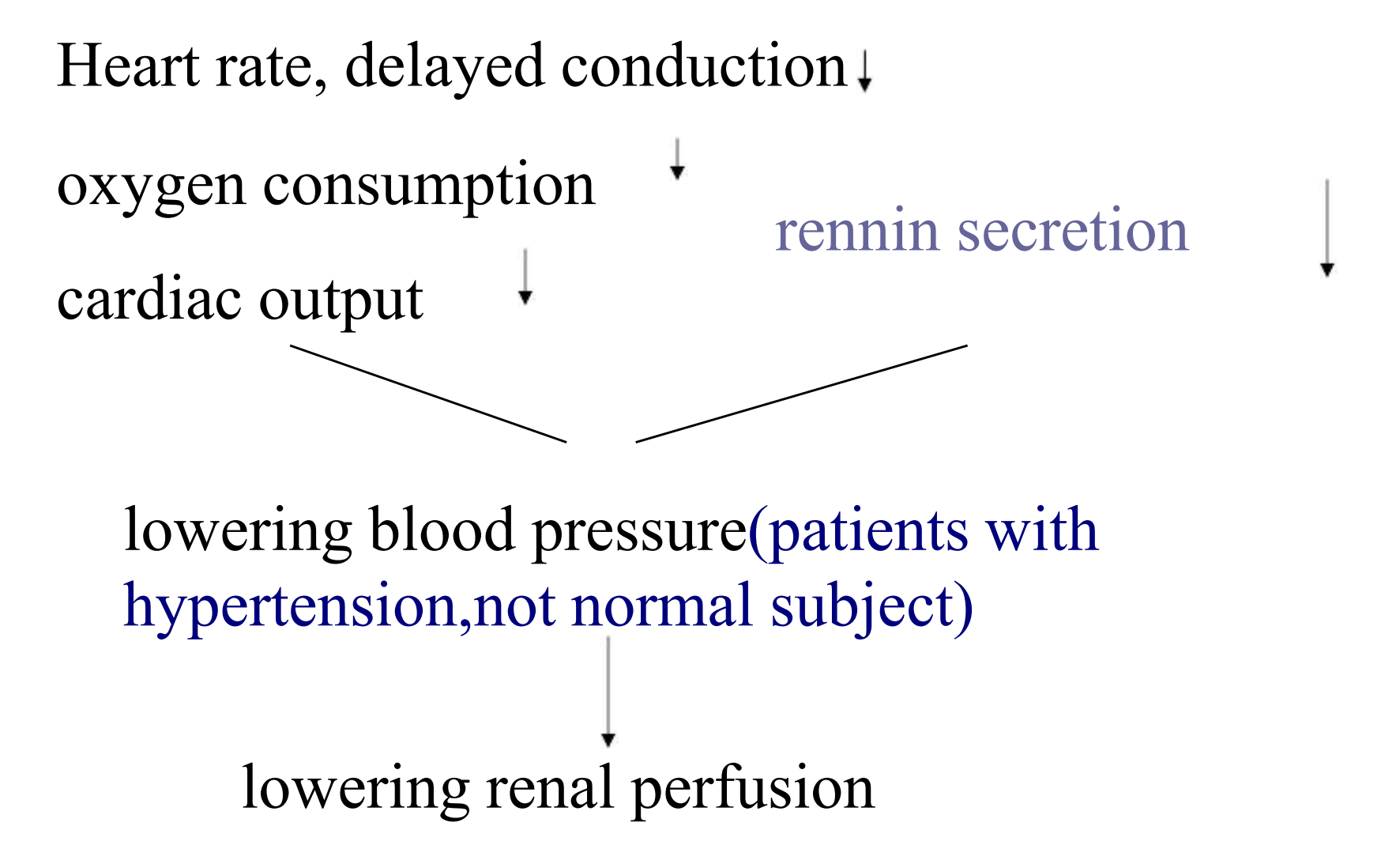
- rennin secretion 凝乳酶分泌
- lowing renal perfusion 降低肾灌注
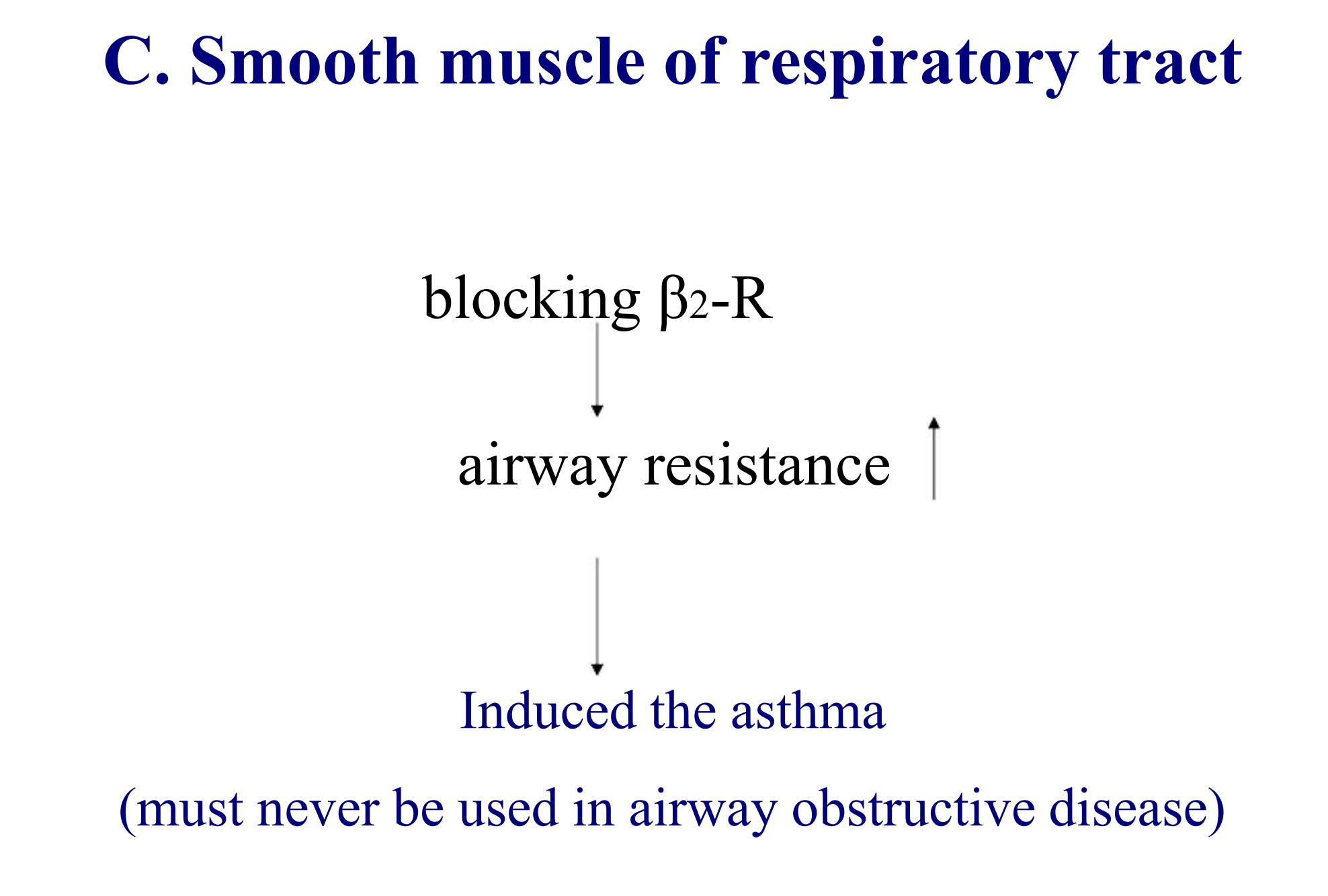
4. blocking β2-R effects
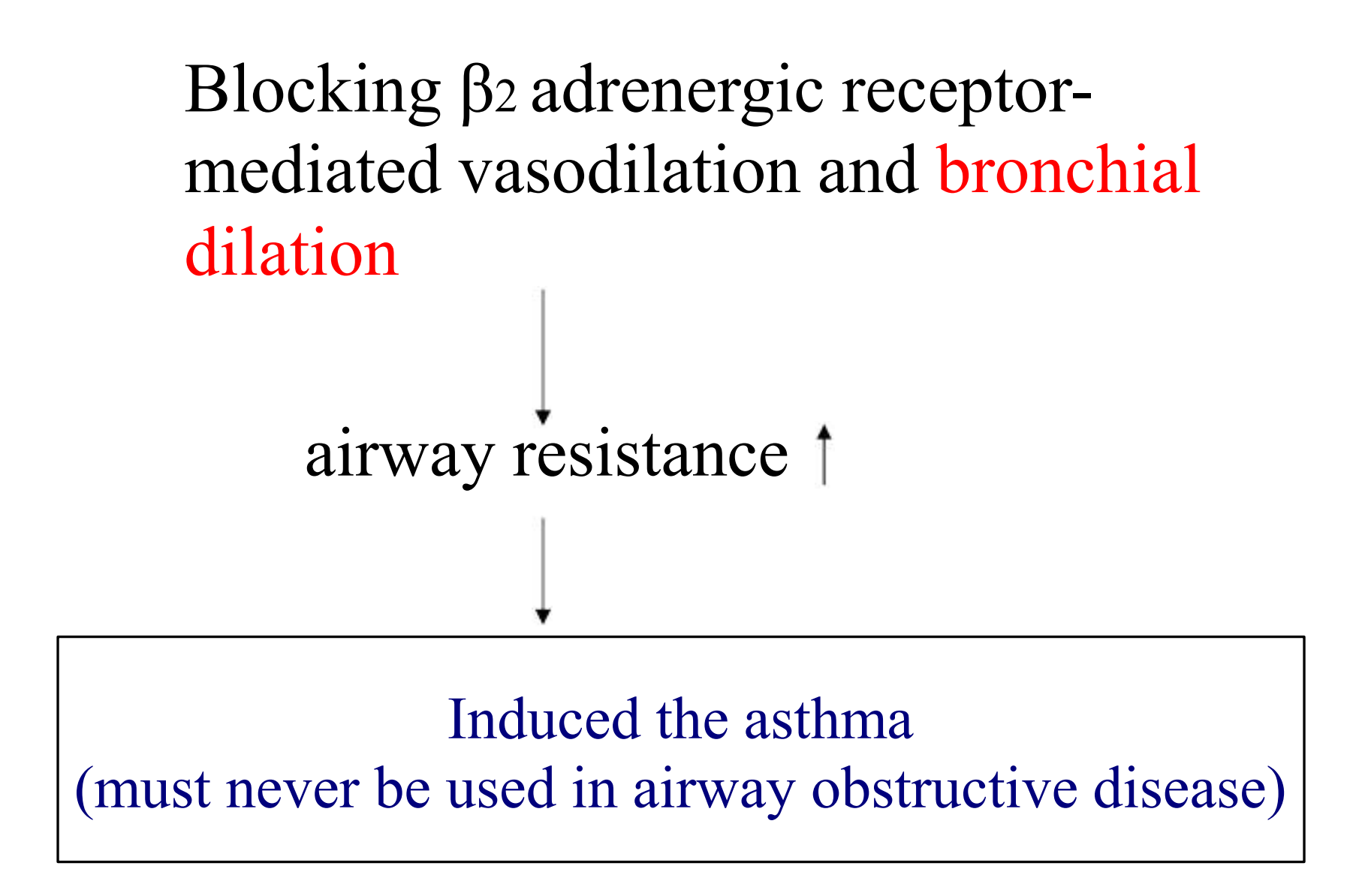
- bronchial dilation 支气管扩张
- block beta 3 will cause some severe effects (such as 低血糖)
5. α-R block drugs
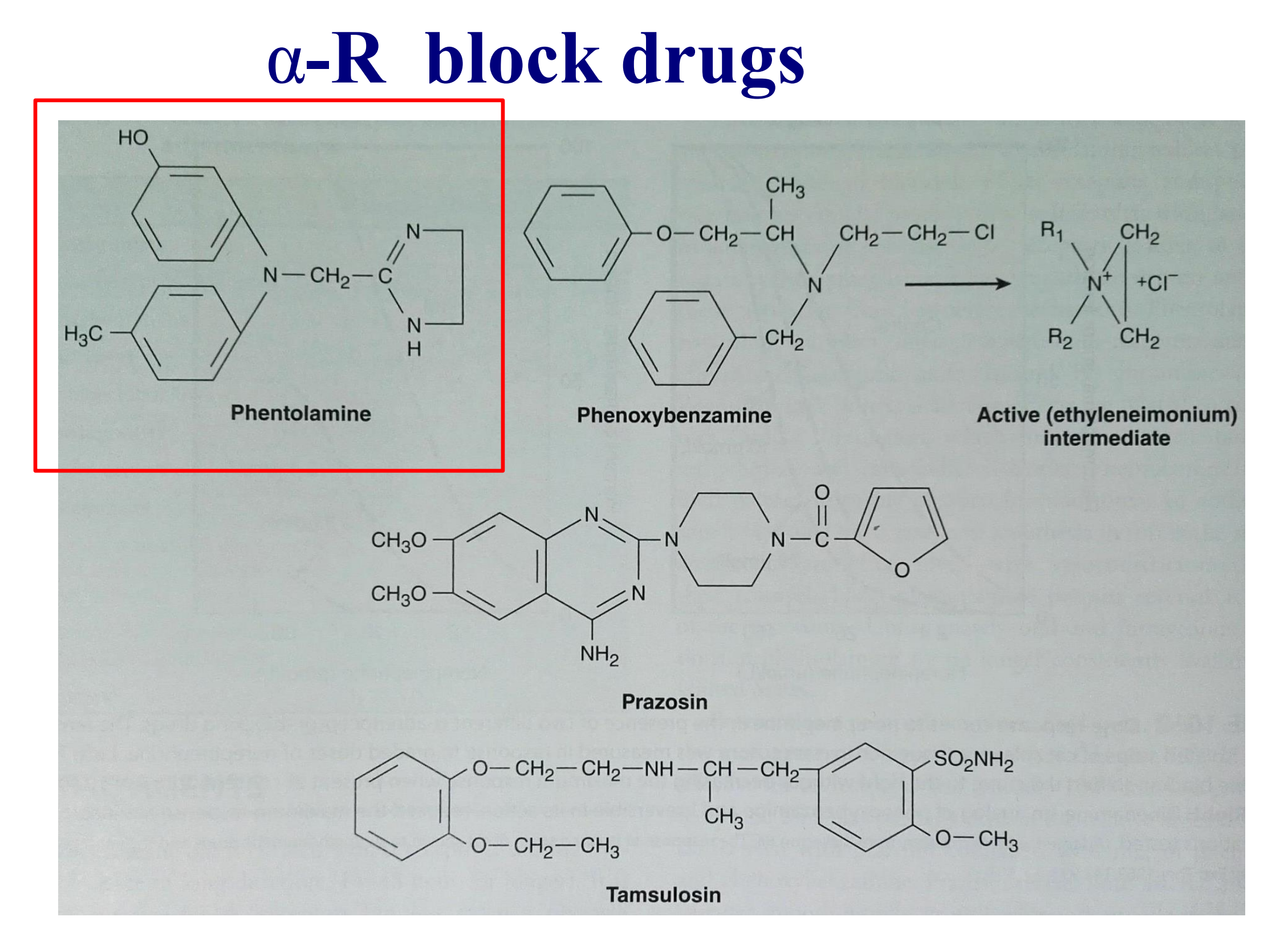
Phentolamine
1. Pharmacological effects
β-adrenergic blocking drugs
1. Classification
Nonselective β-R blockers
full blockers: propranolol, timolol, sotalol, nadolol
with ISA: alprenolol, oxprenolol, pindolol
Selective β1-R blockers
full blockers: metoprolol, esmolol,atenolol
with ISA: acebutolol
2. Pharmacological effects
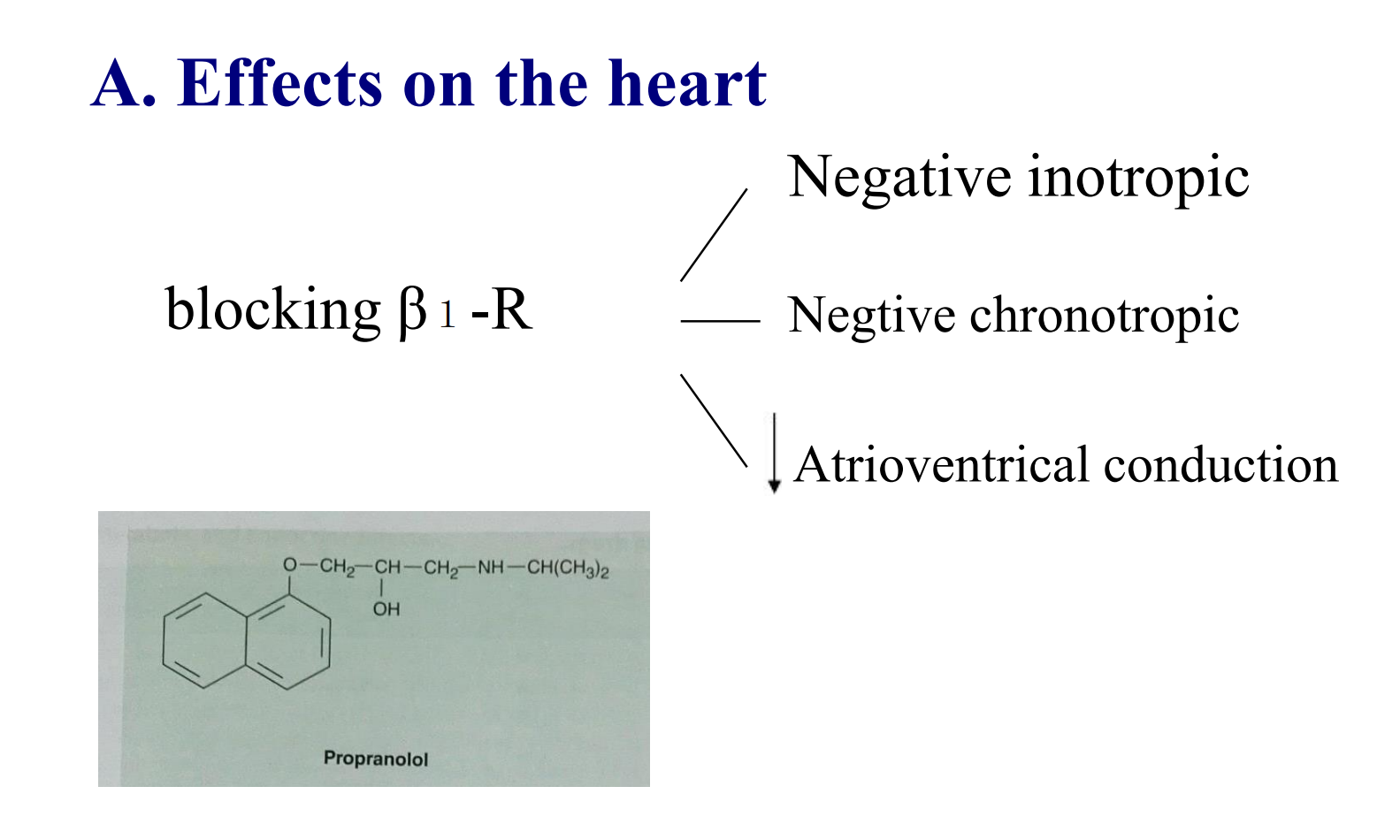
- negative inotropic 负性肌力
- negative chronotropic 负性变时
- decreased atrioventrical conduction 房室传导阻滞
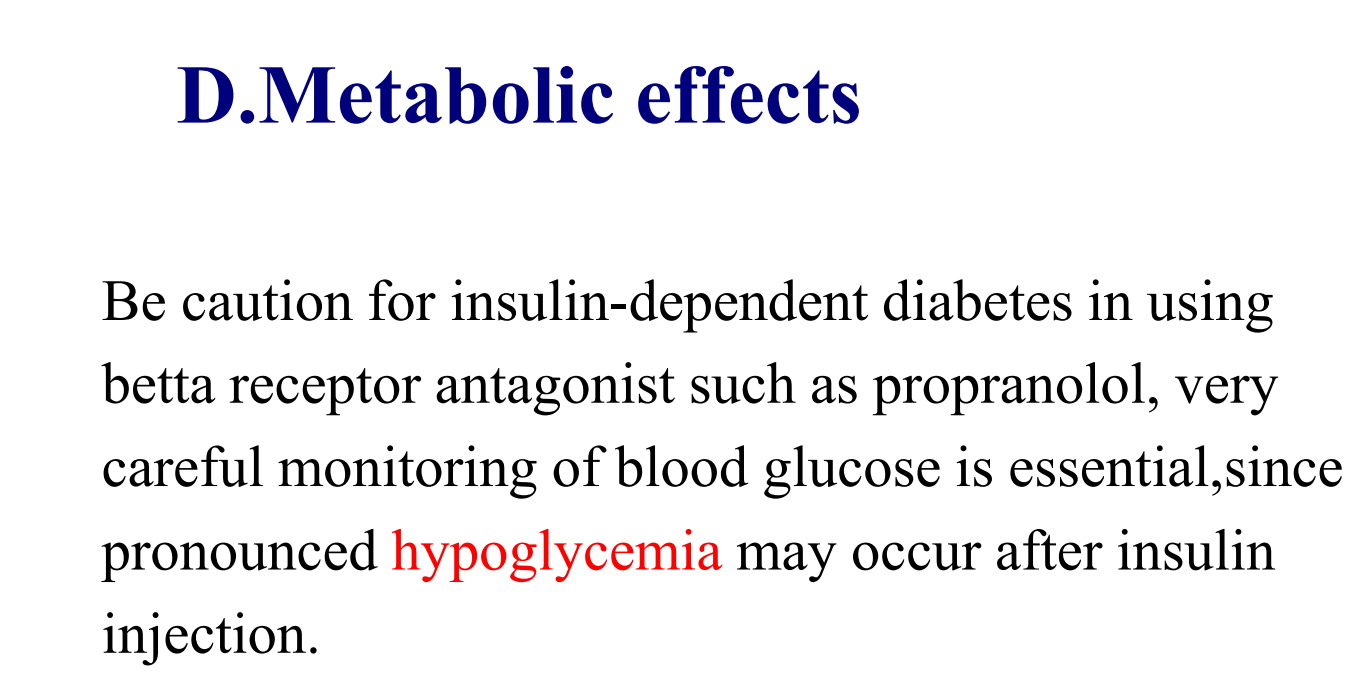
- hypoglycemia for a long time will cause people to die, therefore the hypoglycermia is more dangerous