L13 Adaptive Immunity
一、Overview of Adaptive Immunity
Major functions:
- recognize nonself
- respond to nonself
- remember nonself
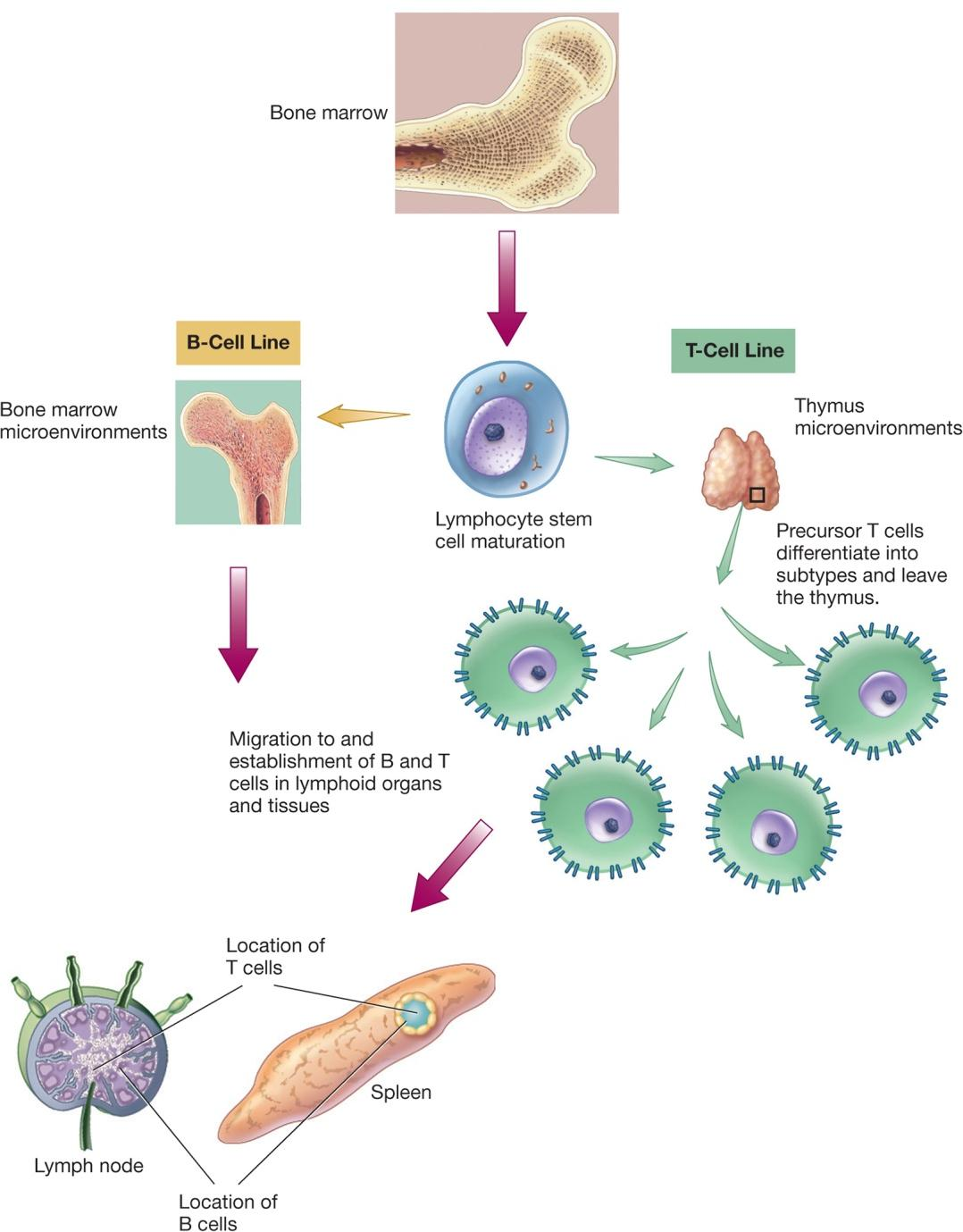
Acquired Immune System Development
Introduction of Specific Immunity
1. Four Characteristics of Specific Immunity
- Discrimination between self and non-self: usually responds selectively to non-self
- Diversity: generates enormous diversity of molecules
- Specificity: against one specific pathogen or foreign substance
- Memory: response to a second exposure to a pathogen is more fast
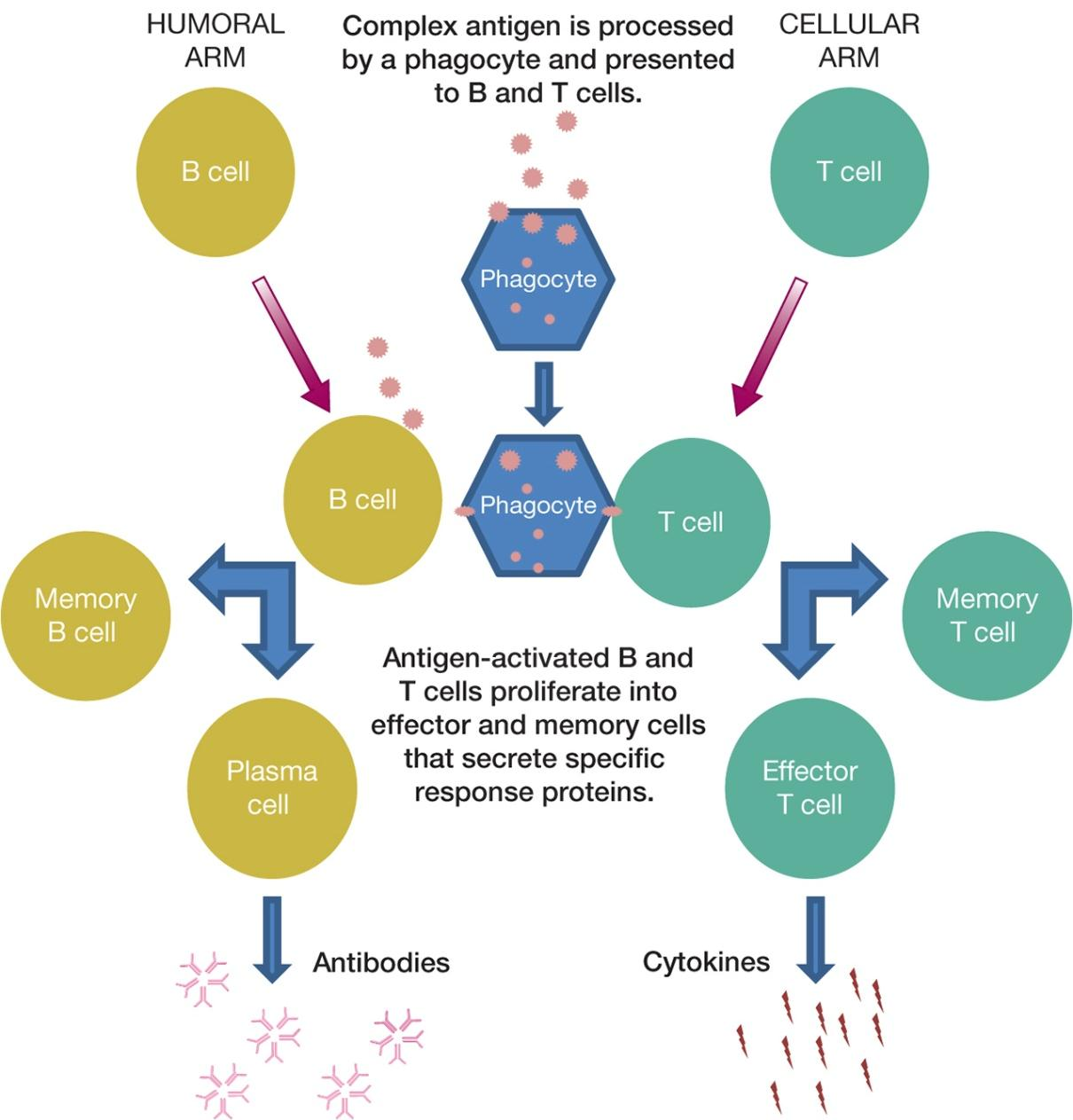
2. Types of Specific Immunity
- Humoral immunity
also called antibody-mediated immunity
based on antibody activity
- Cellular immunity
also called cell-mediated immunity
based on T cell action
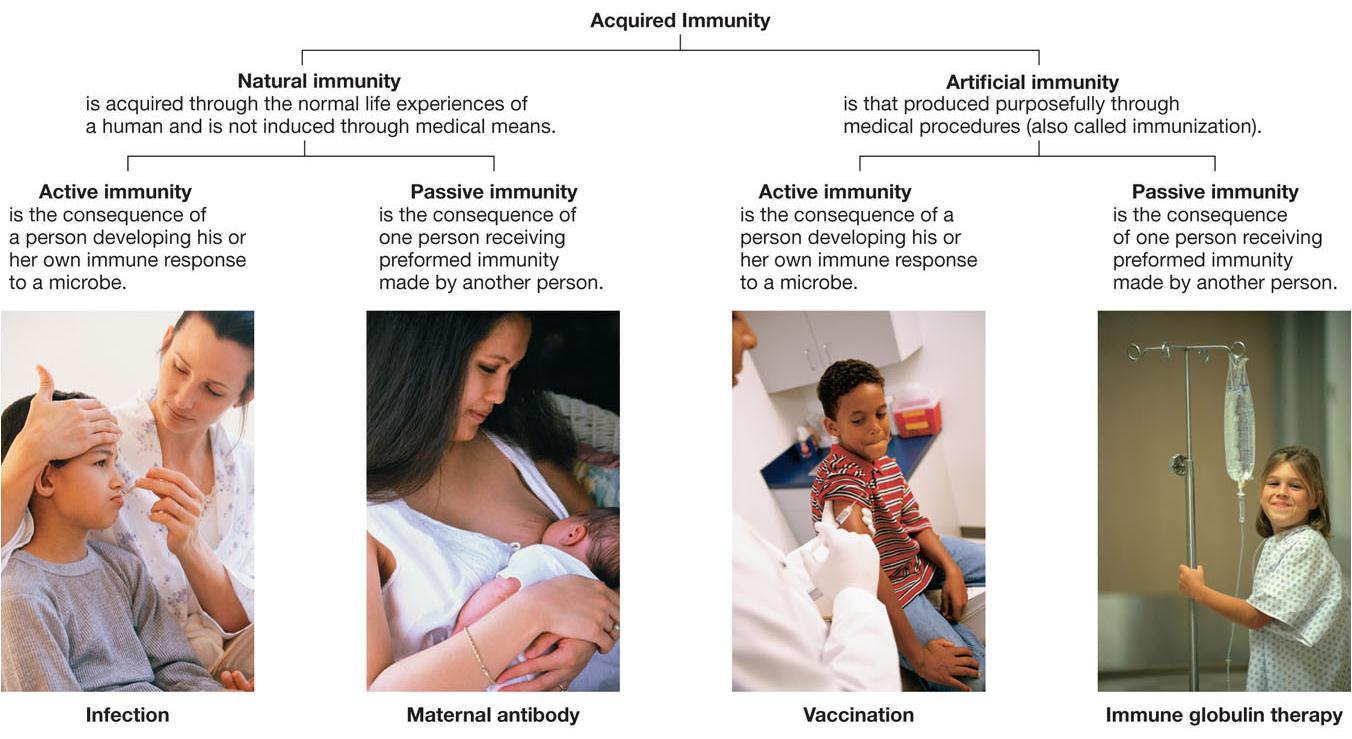
Natural Immunity 先天免疫
Is acquired through the normal life experiences of a human and is not induced through medical means.
**Artificial immunity **人工免疫
Is that produced purposefully through medical procedures (also called immunization).
**Active immunity **自动(主动)免疫
Is the consequence of a person developing his or her own immune response to a microbe.
Passive immunity 被动免疫
Is the consequence of one person receiving preformed immunity made by another person
Components Involved In Adaptive Immunity
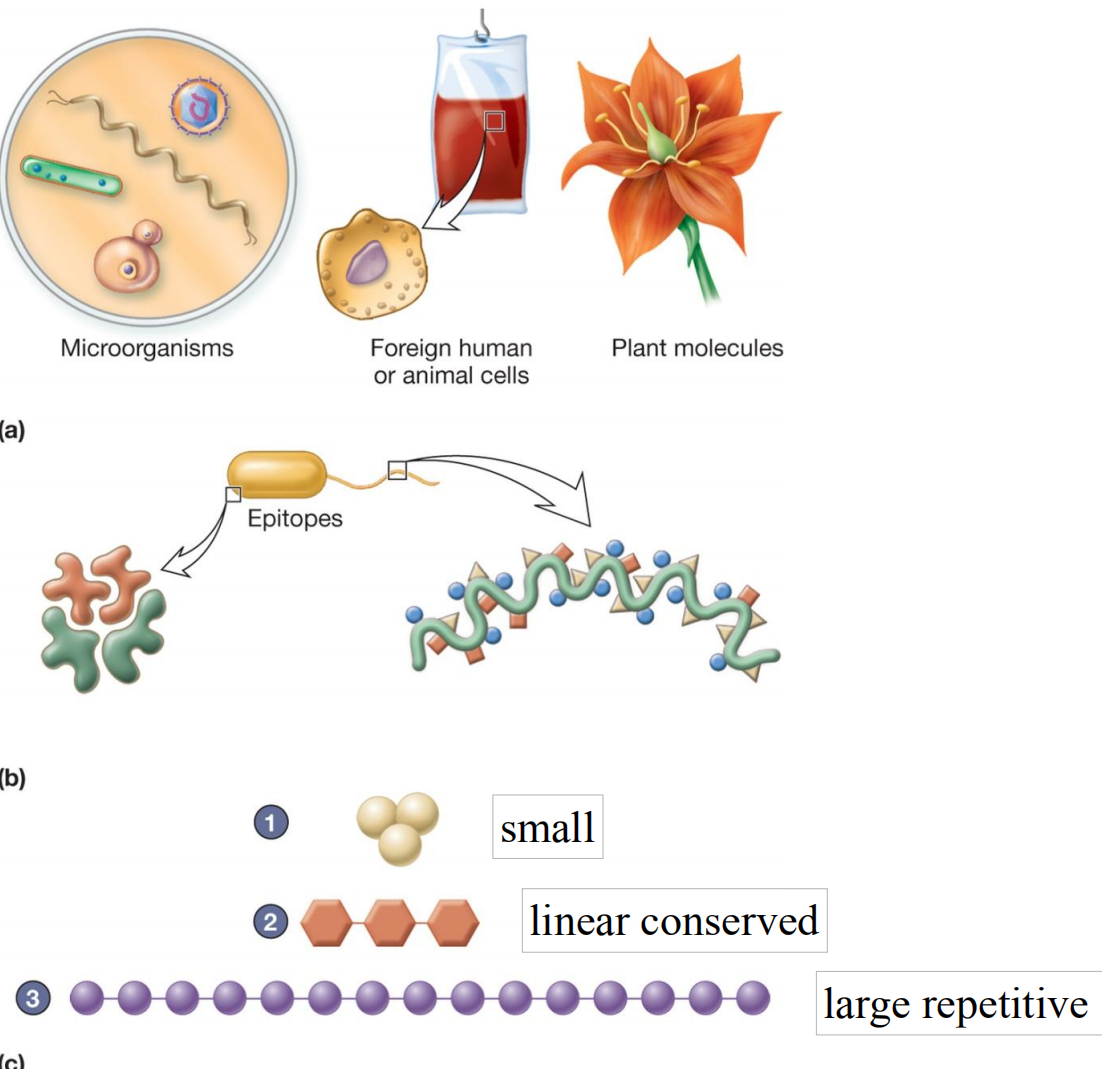
1. Antigens
**Antigenic determinant sites (epitopes) **抗原决定簇位点(表位)
- site on antigen that reacts with antibody or TCR (T cell acceptor)
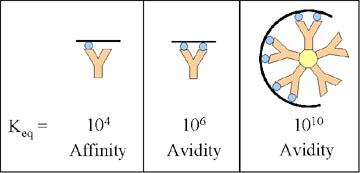
Antibody affinity
- strength with which antibody binds to its antigen at a given antigen-binding site
Avidity of antibody
- overall antigen-binding at all antigen binding sites
2. Haptens 半抗原
半抗原(hapten)是指本身分子量过小,无法刺激免疫反应,必须和载体(carrier)结合成较大的才能刺激发生免疫反应。半抗原能与对应抗体结合出现抗原-抗体反应,又不能单独激发人或动物体产生抗体的抗原,它只有抗原性,不具免疫原性,又称不完成抗原。大多数多糖和所有类脂都属于半抗原,如果用化学方法把半抗原与某种纯蛋白的分子载体(protein carrier)结合,纯蛋白会获得新的免疫原性,并能刺激动物产生相应的抗体。半抗原一旦与纯蛋白质结合,就构成该蛋白质的一个抗原簇。
Small organic molecules
Not antigenic but may become antigenic when bound to larger carrier molecule
- e.g., penicillin
- may elicit hapten specific and carrier specific responses
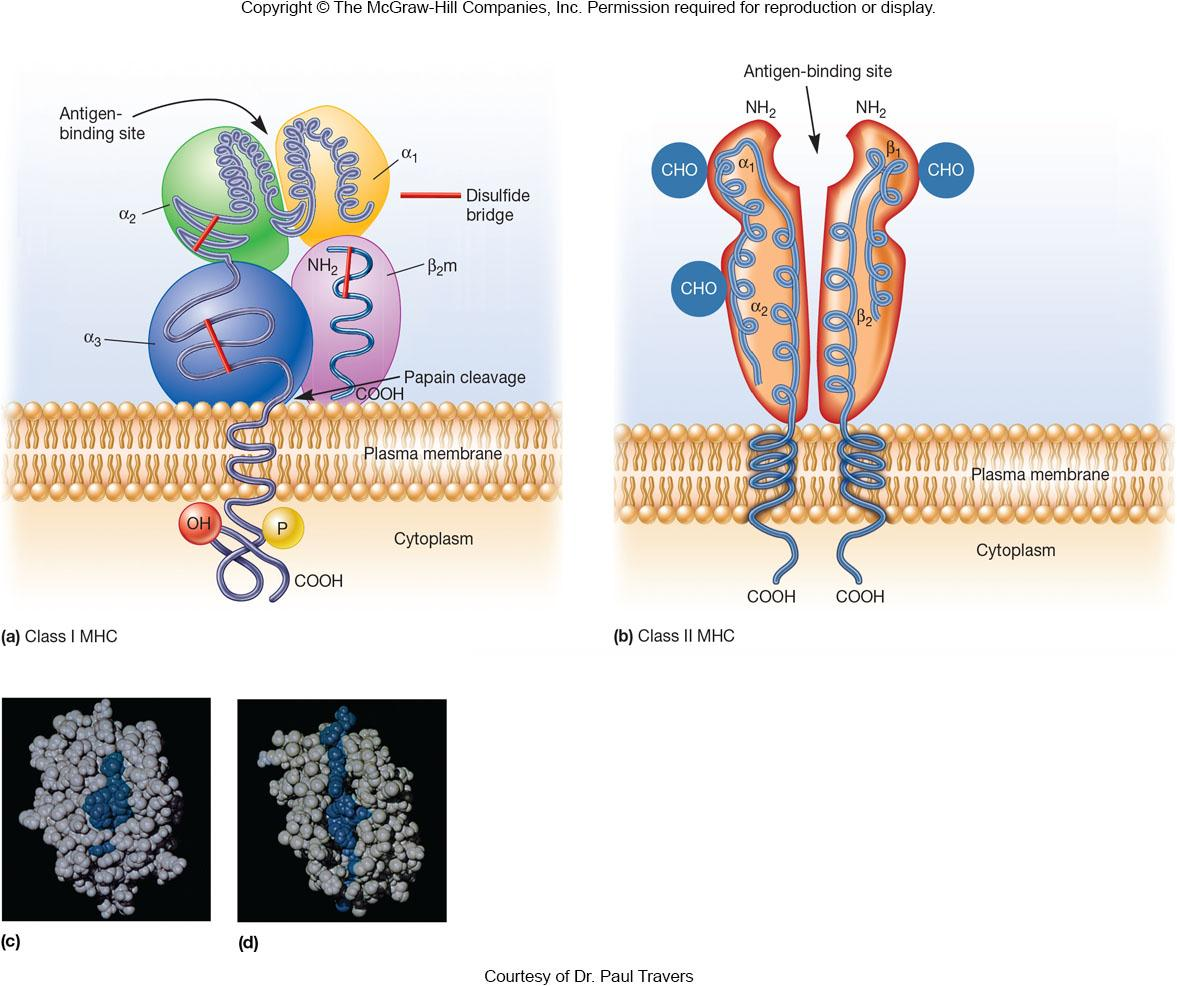
3. Major Histocompatibility Complex (MHC)
Class I molecules found on almost all types of nucleated cells (except RBC)
- important for organ transplantation
Class II molecules found only on antigen presenting cells
- required for T cell communication to macrophages, dendritic cells, B cells
Class III molecules include secreted proteins
- not required for self/nonself recognition
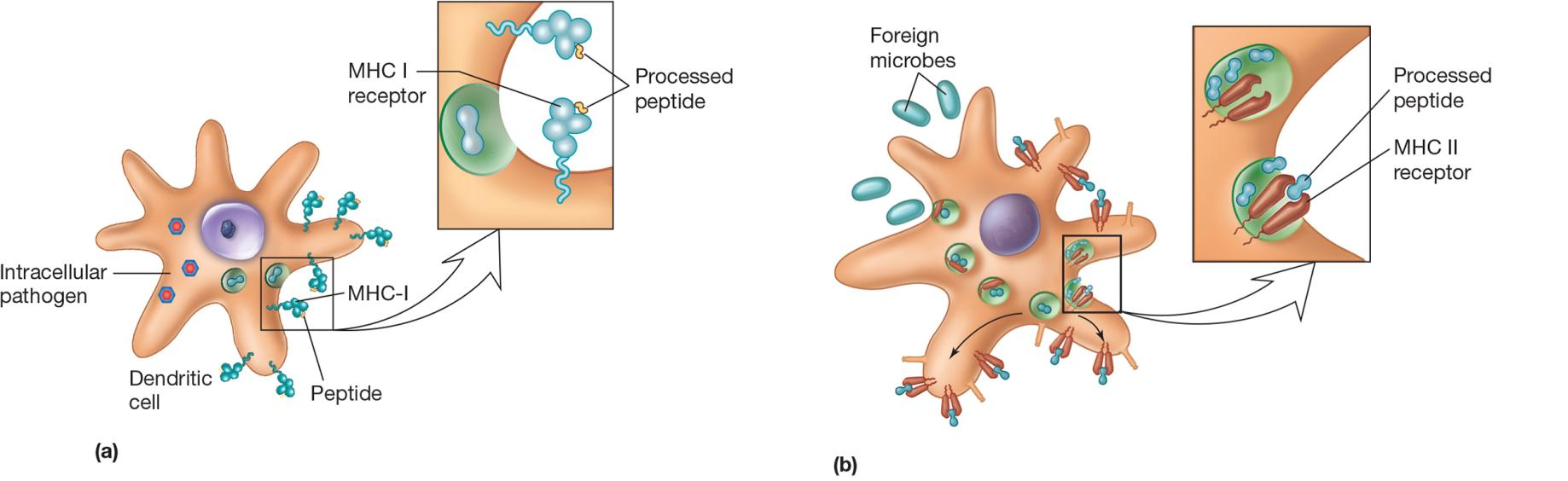
MHC and Antigen Processing
endogenous antigen processing 内源性抗原处理
- class I binds to antigen peptides that originate in the cytoplasm and present antigen to CD8+ T cells
**exogenous antigen processing **外源性抗原处理
- class II binds to antigen fragments that come from outside the cell and present to CD4+ T helper cells
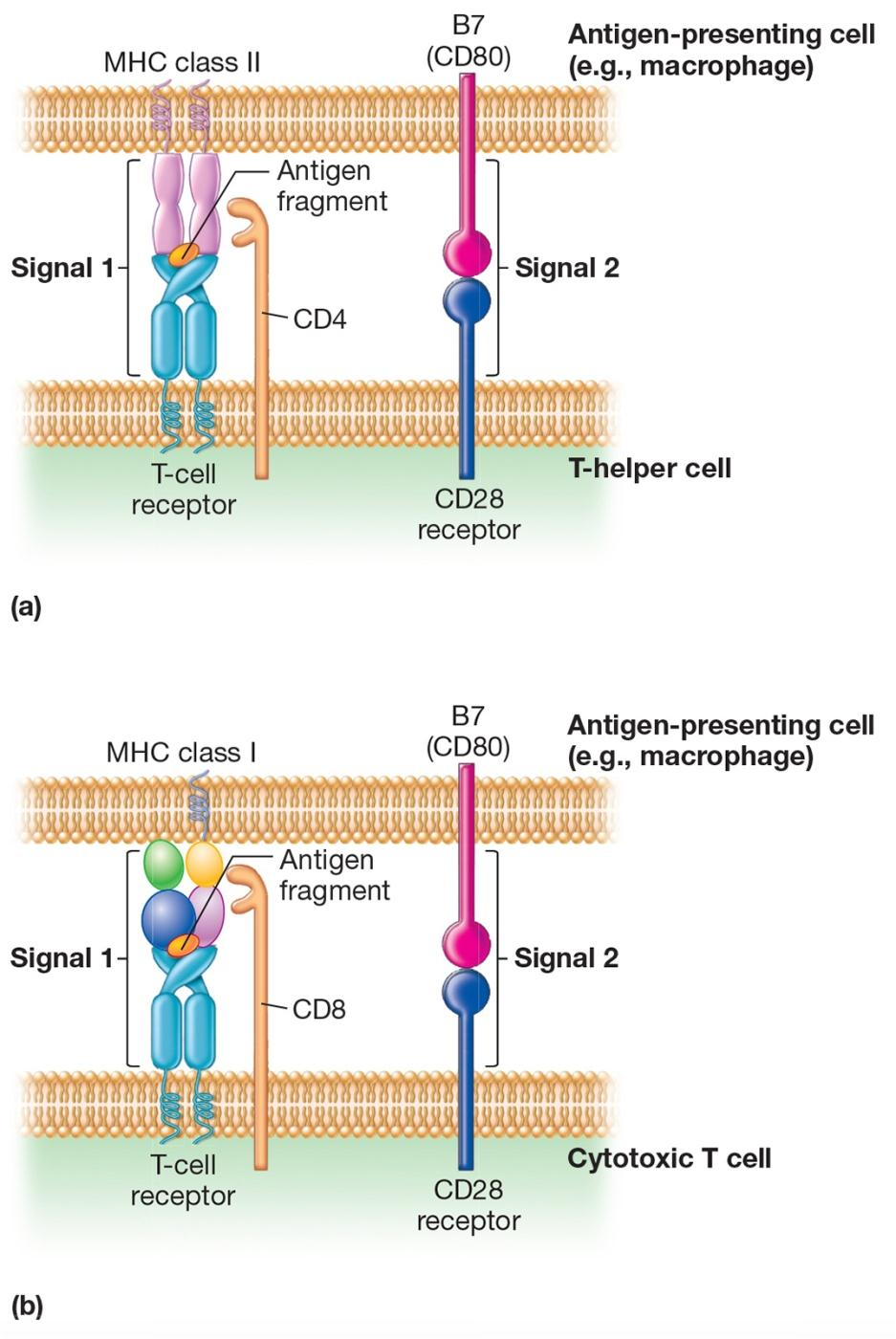
4. Cluster of Differentiation Molecules (CDs)
Membrane proteins on lymphocytes and other cells
- used to identify and differentiate between leukocyte subpopulations
二、T-Cell Biology
Major players in cell-mediated immune response
Originate from CD34+ stem cells in the bone marrow but mature in thymus
Immunologically specific and function in a variety of regulatory and effector ways
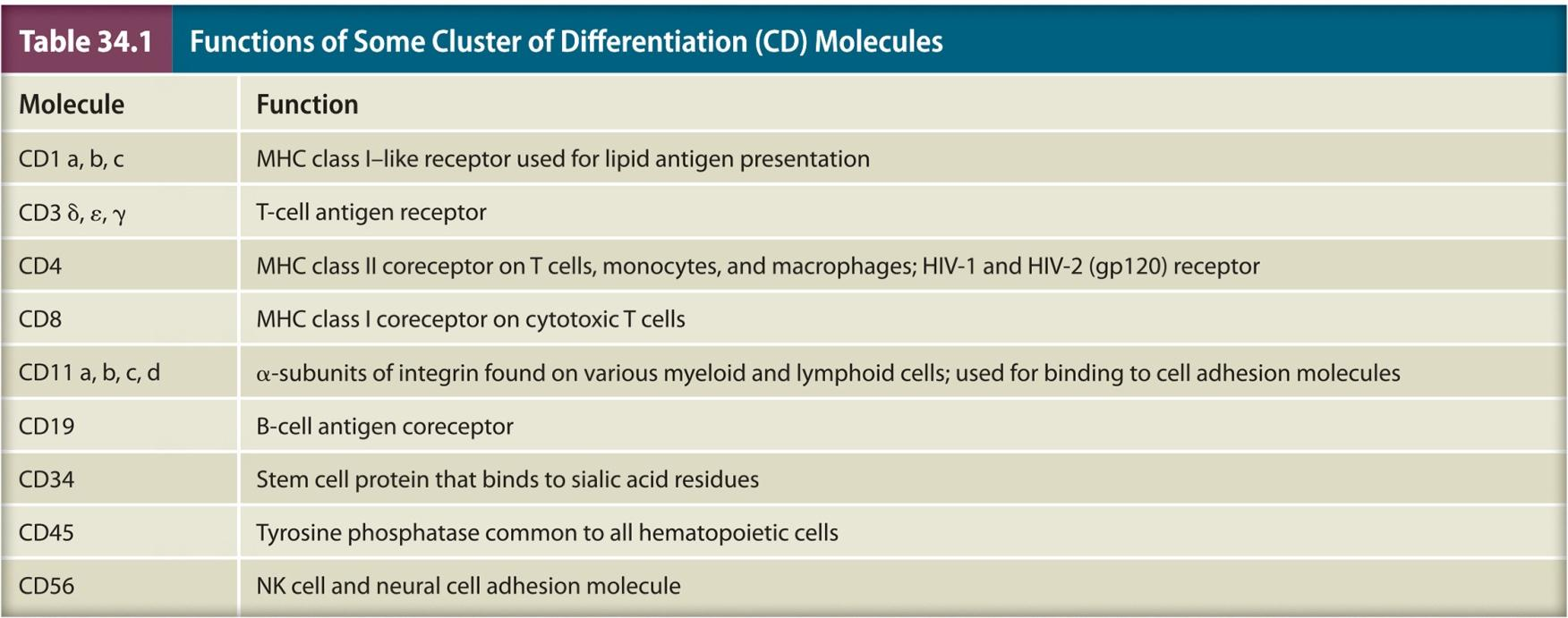
T-Cell Receptors (TCRs)
Membrane proteins
Recognize and bind fragments of antigens
Antigen fragments must be presented by MHC molecules
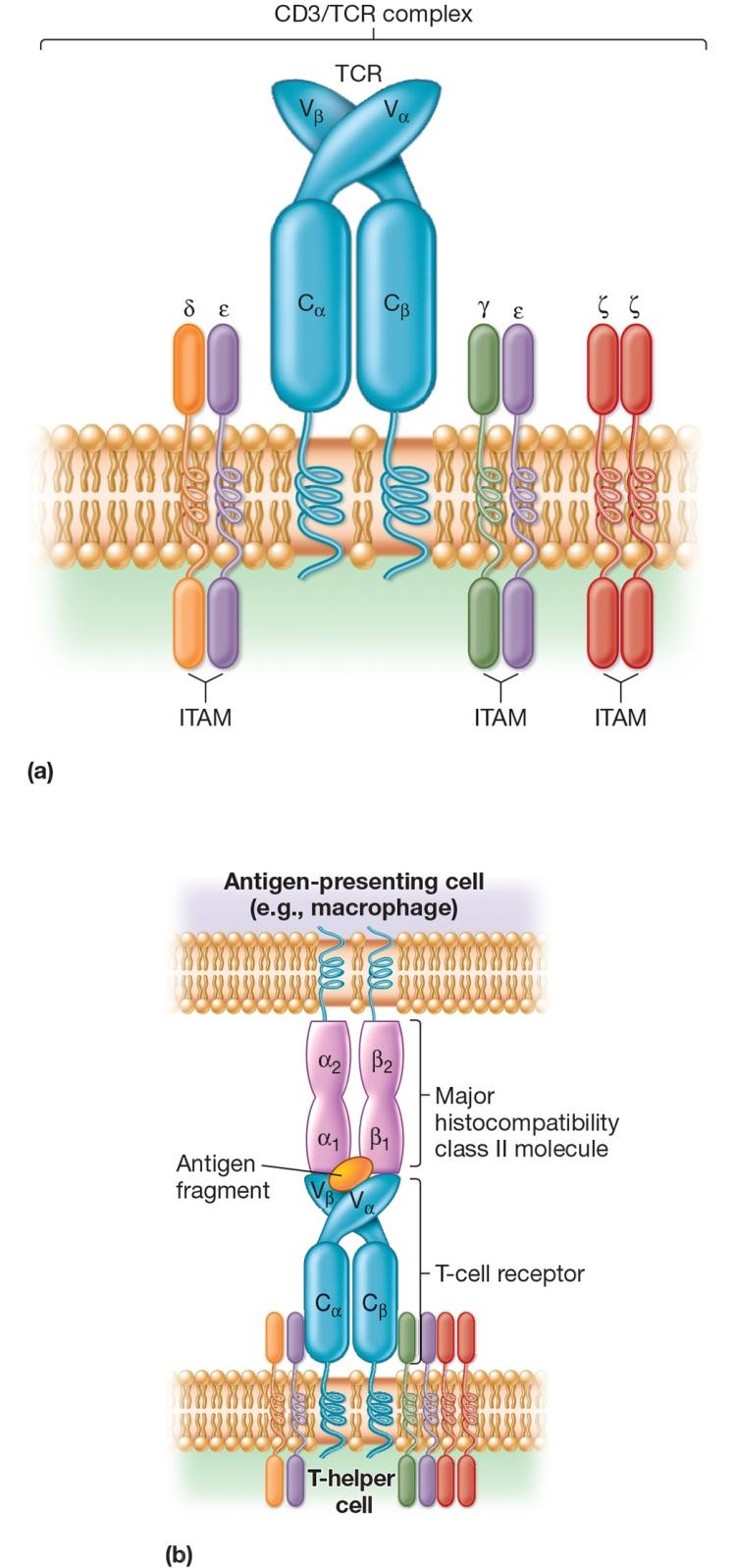
T Cell Activation
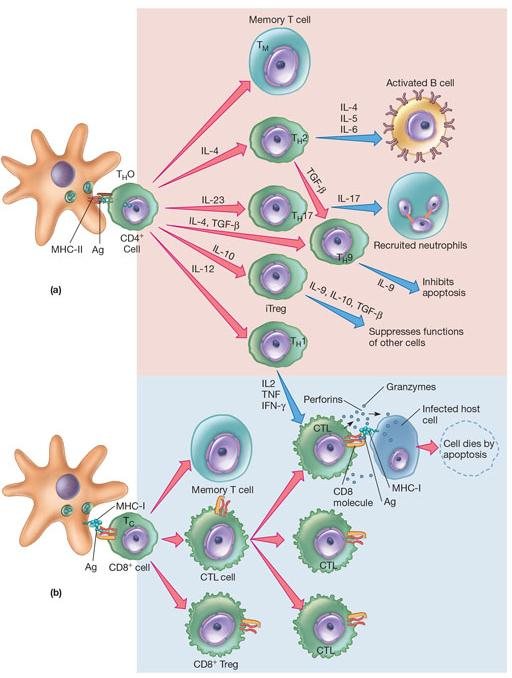
T Cell Types
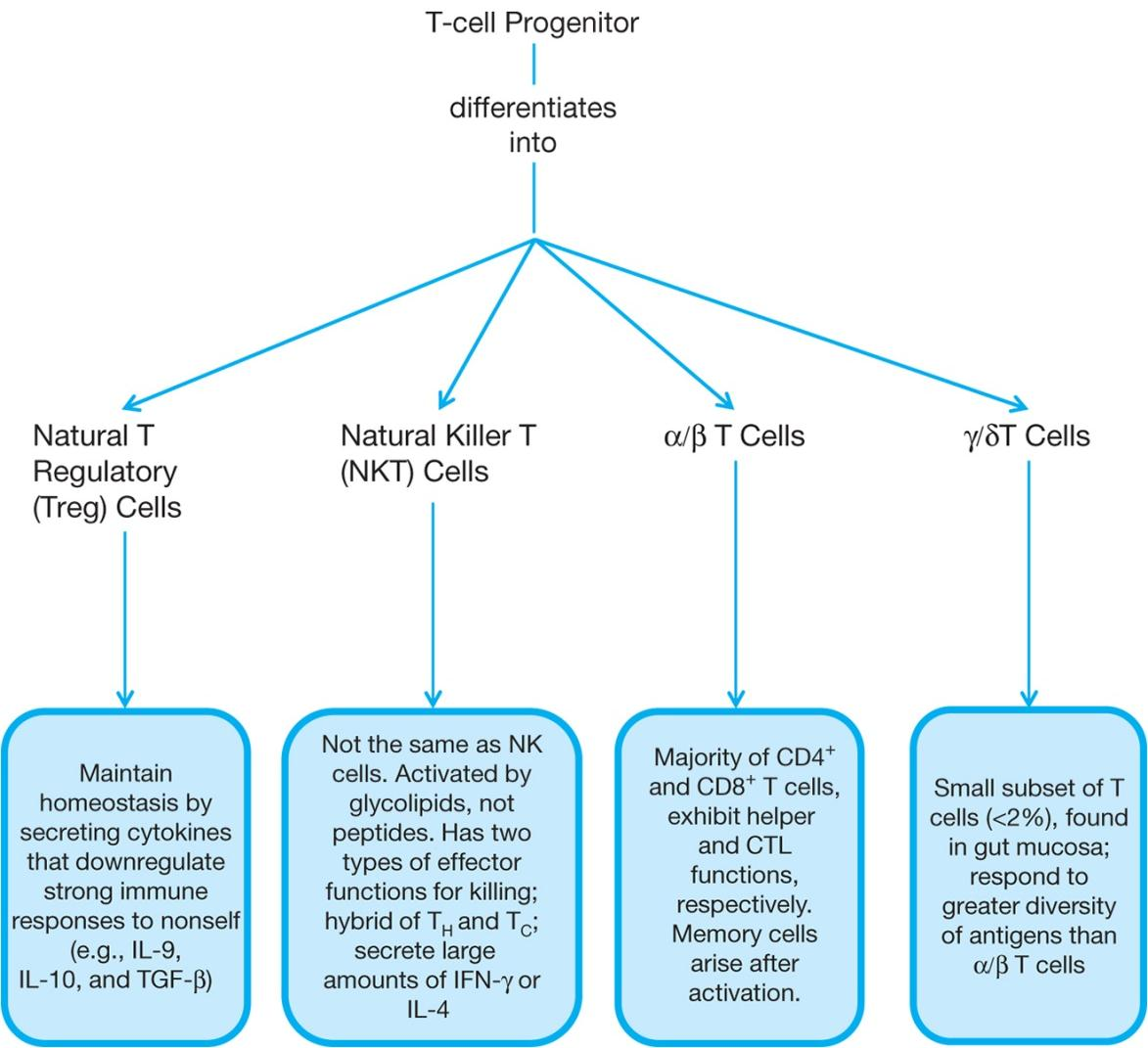
T-cell Progenitor differentiates into:
Natural T Regulatory (Treg) Cells: Maintain homeostasis(稳态) by secreting cytokines that downregulate strong immune responses to nonself (e.g., IL-9, IL-10, andTGF-P)
Natural Killer T (NKT) Cells: Not the same as NK cells. Activated by glycolipids, not peptides. Has two types of effector functions for killing; hybrid of TH and Tc; secrete large amounts of IFN-γ or IL-4
α/β T Cells: Majority of CD4+ and CD8+ T cells, exhibit helper and CTL functions, respectively. Memory cells arise after activation.
γ/δ T Cells: Small subset of T cells (<2%), found in gut mucosa; respond to greater diversity of antigens than α/β T cells
T Cell Development
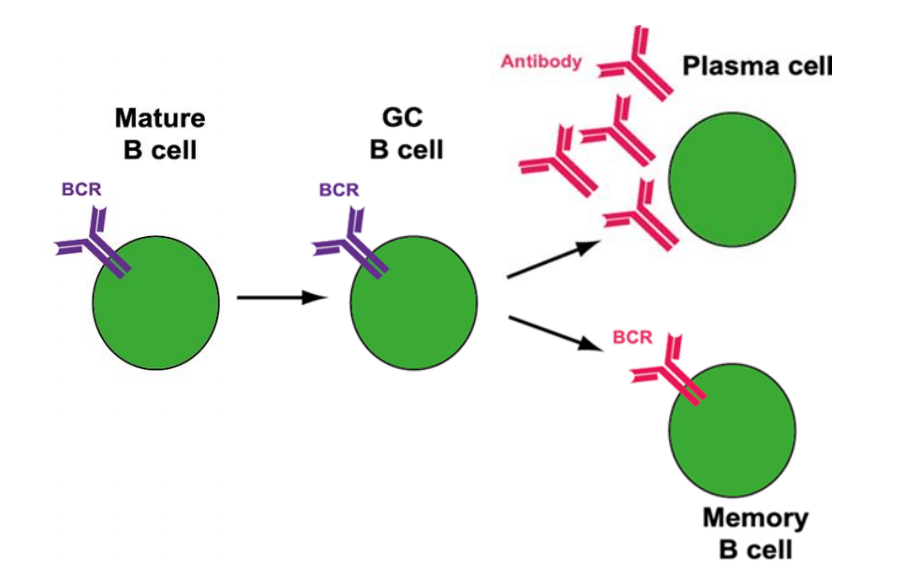
三、B-Cell Biology
B-Cell Activation
Two mechanisms for antigen-specific activation
- T dependent
- T independent
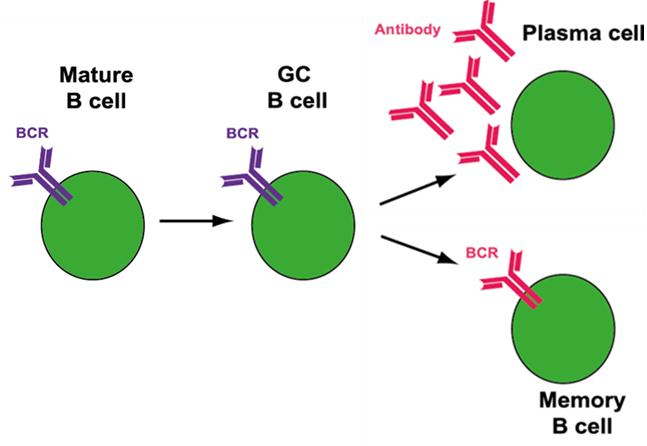
1. T-Dependent Antigen Triggering
Require two signals
- antigen-BCR specific interaction
- T cell signal
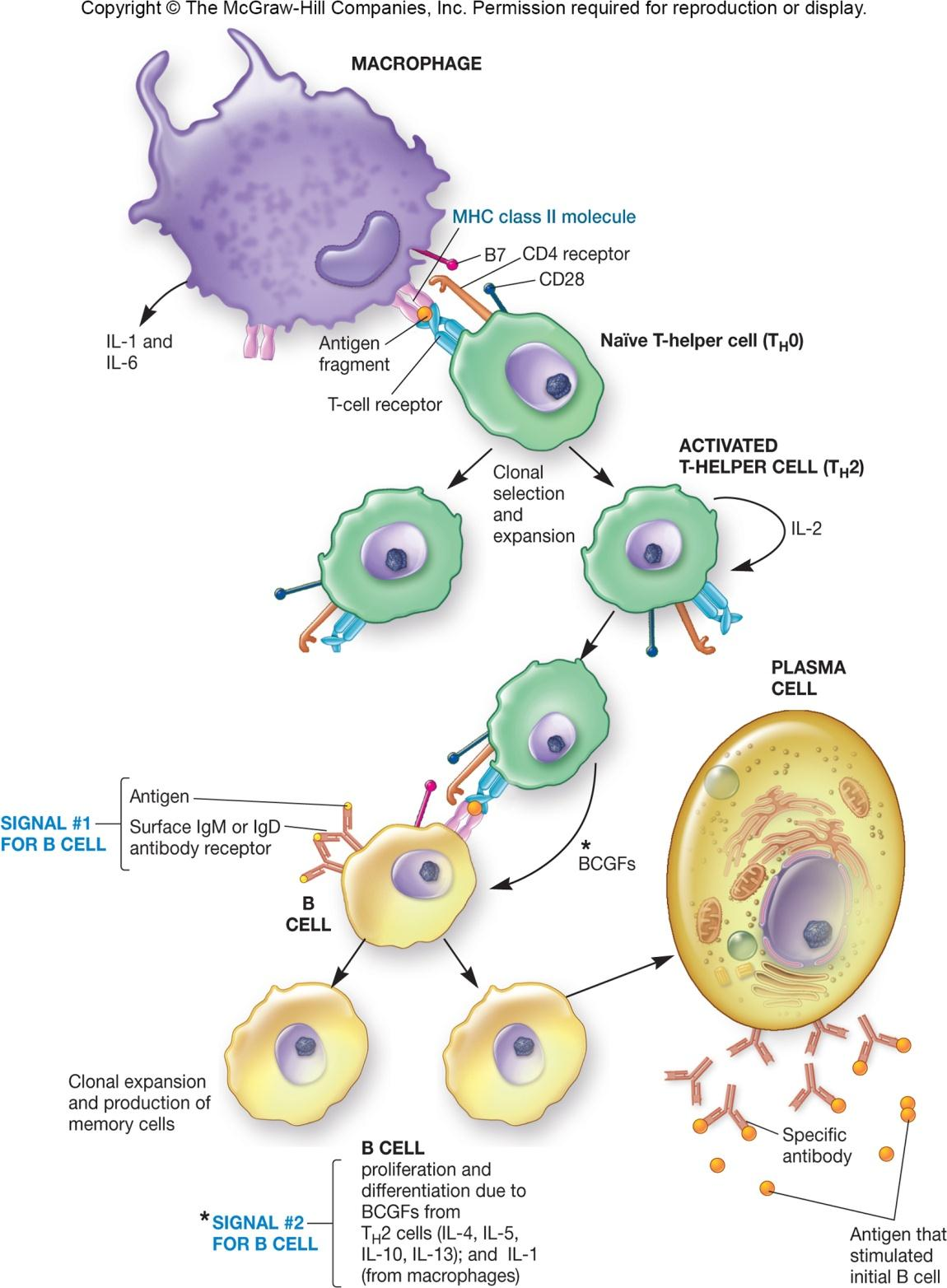
2. T-lndependent Antigen Triggering
T-independent antigens
- polymeric antigens with large number of identical epitopes (e.g., LPS)
Less effective than T-dependent B cell activation
- antibodies produced have a low affinity for antigen
- no memory B cells formed
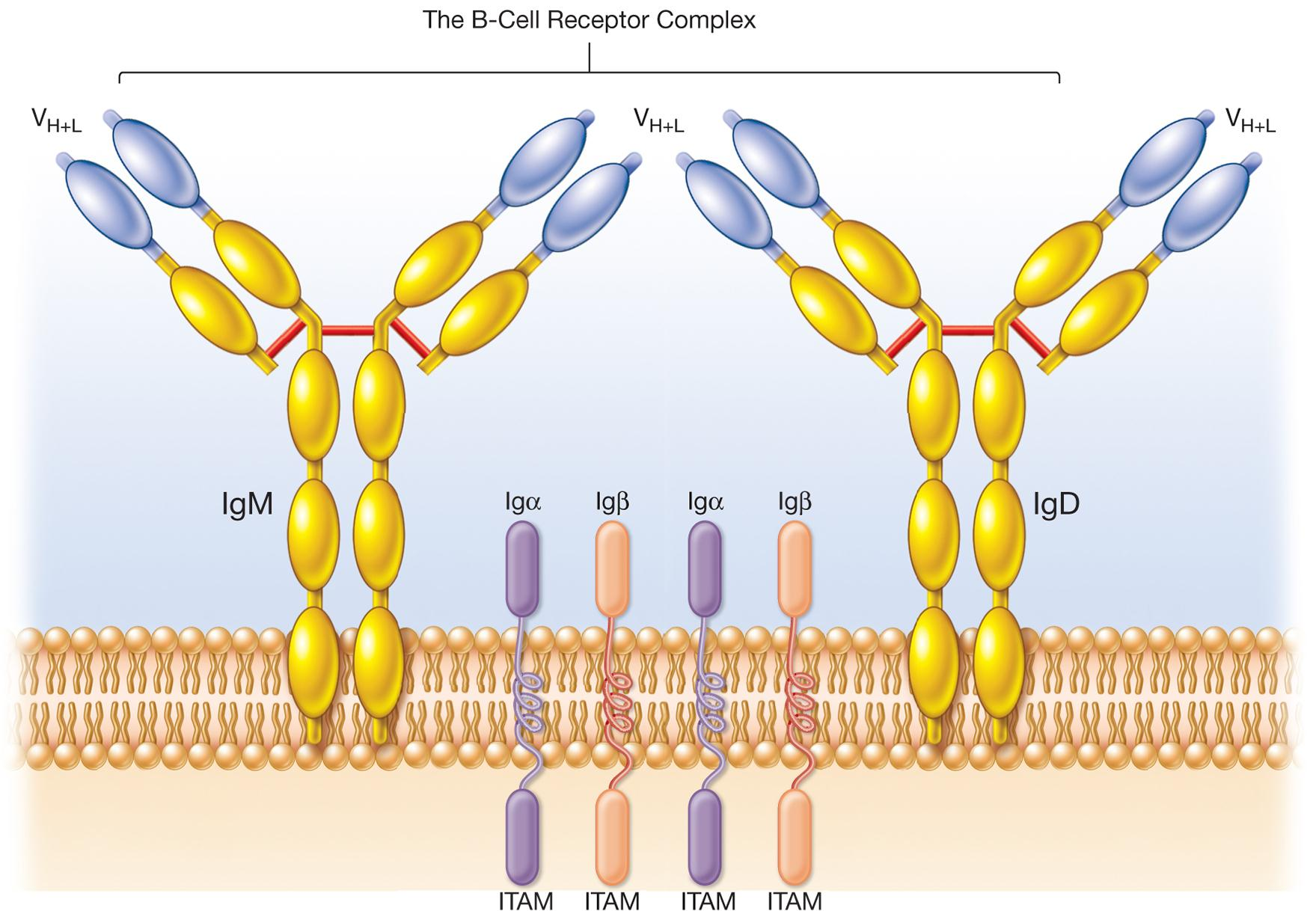
Antibody
Antibody
- immunoglobulin (Ig)
- glycoprotein made by plasma cells
- serves as antigen receptor (BCR) on B cell surface
Found in blood serum, tissue fluids, and mucosal surfaces of vertebrate animals
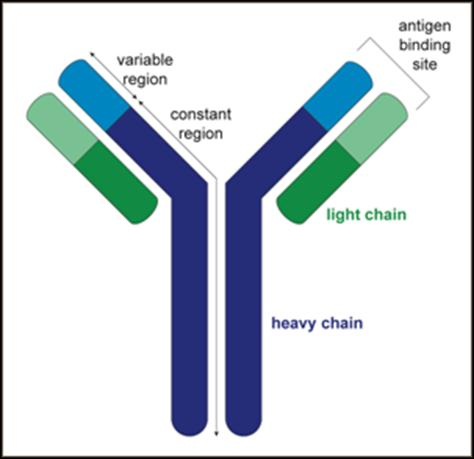
1. Immunoglobulin Structure
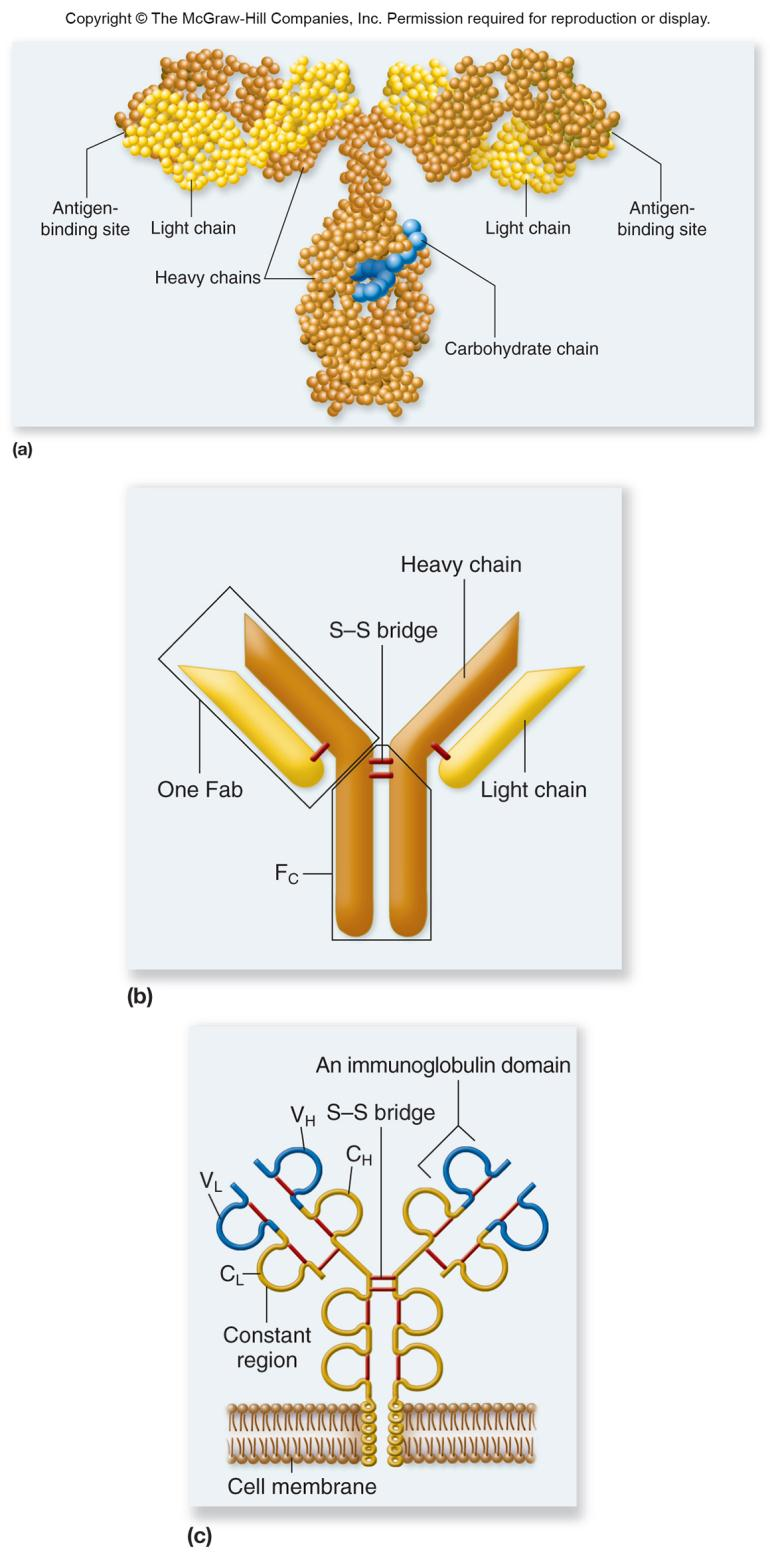
Four chains are arranged in form of a flexible Y shape
Fab fragments (variable and constant regions)
Fc fragment (constant regions only)
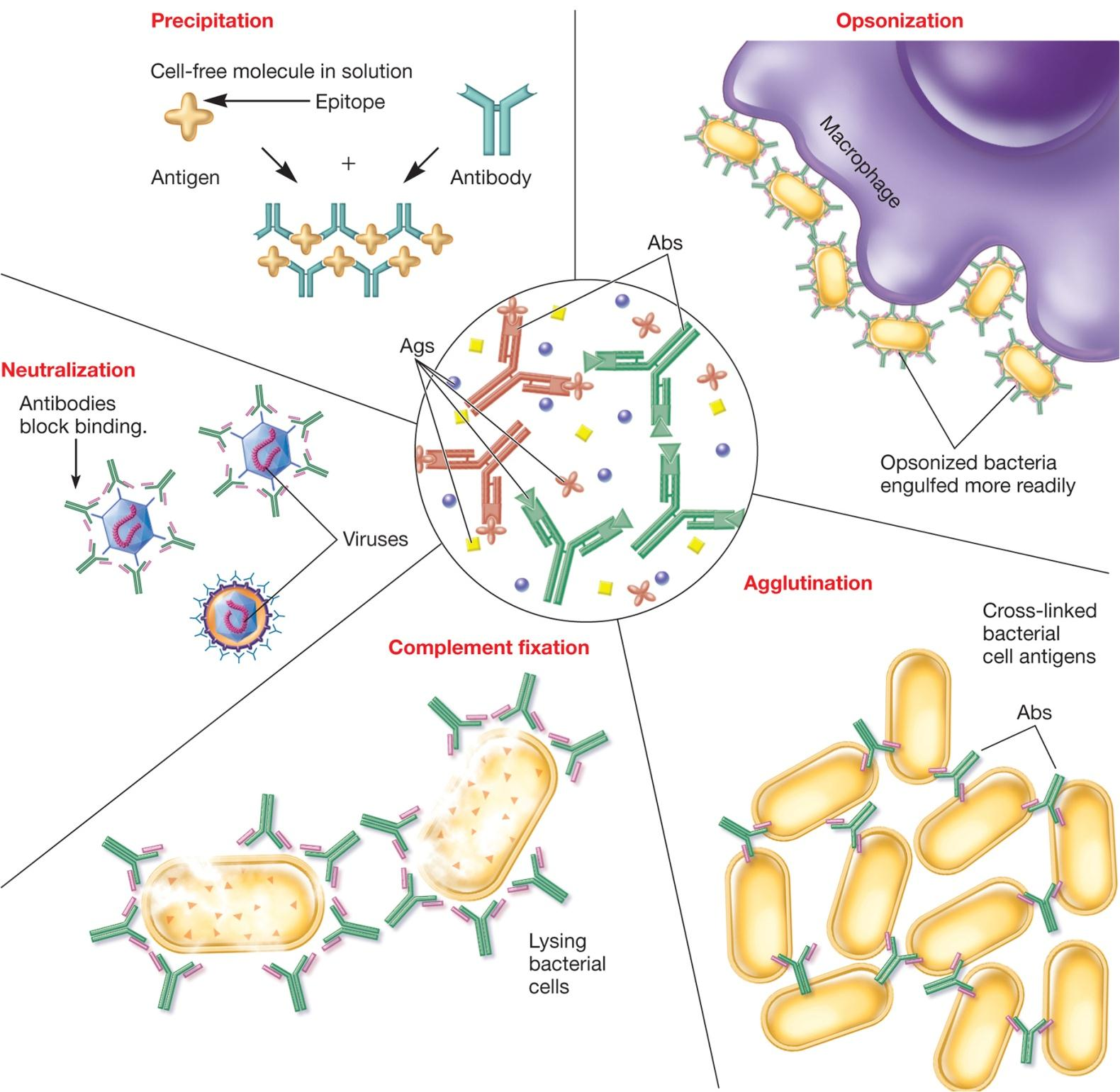
2. Immunoglobulin Function
Fab binds antigen specifically
- activates nonspecific defense mechanisms
- e.g., opsonization for enhanced phagocytosis
Fc mediates binding to:
- host tissue
- various cells of immune system
- first component of complement system
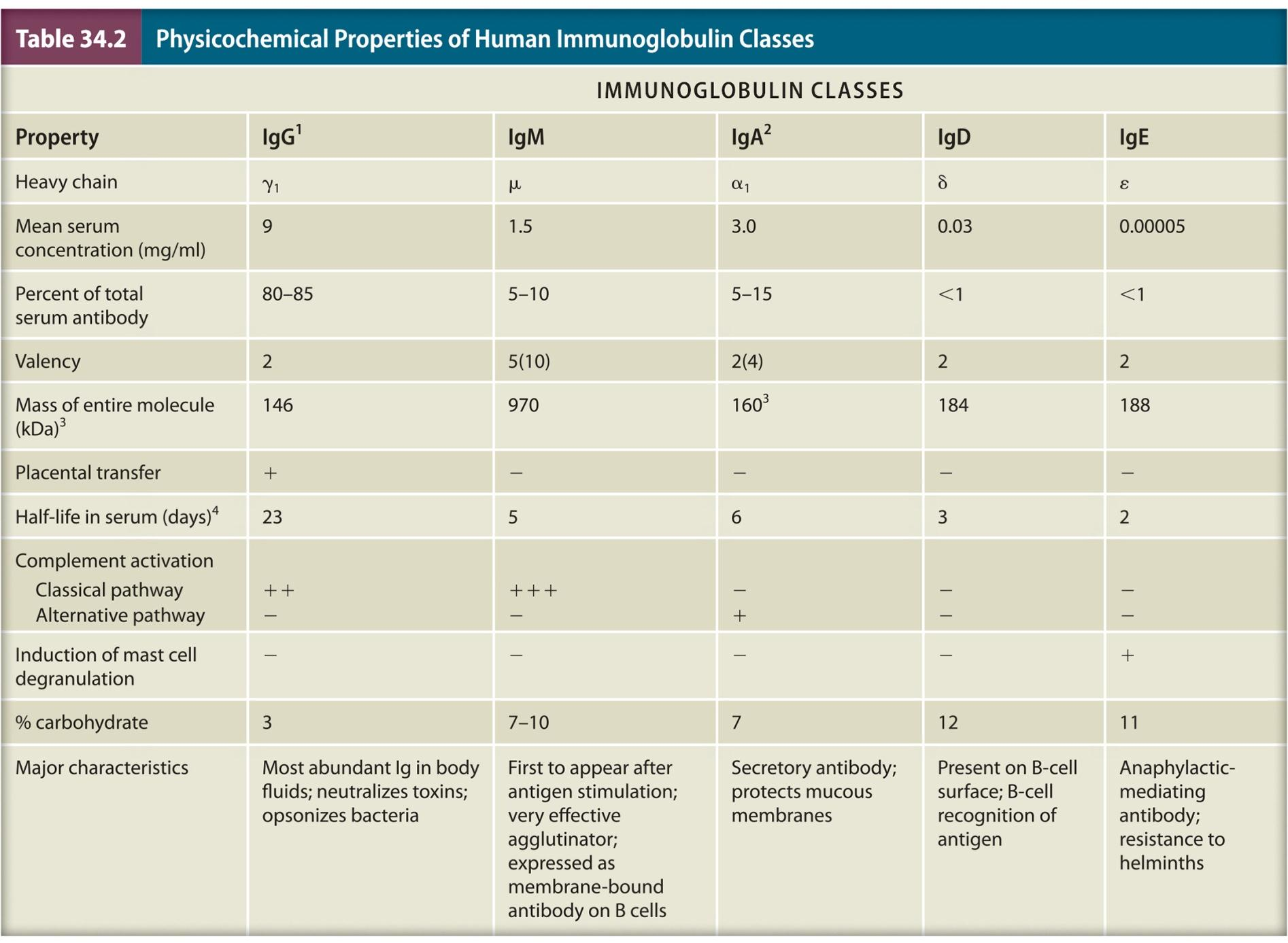
3. Immunoglobulin Classes
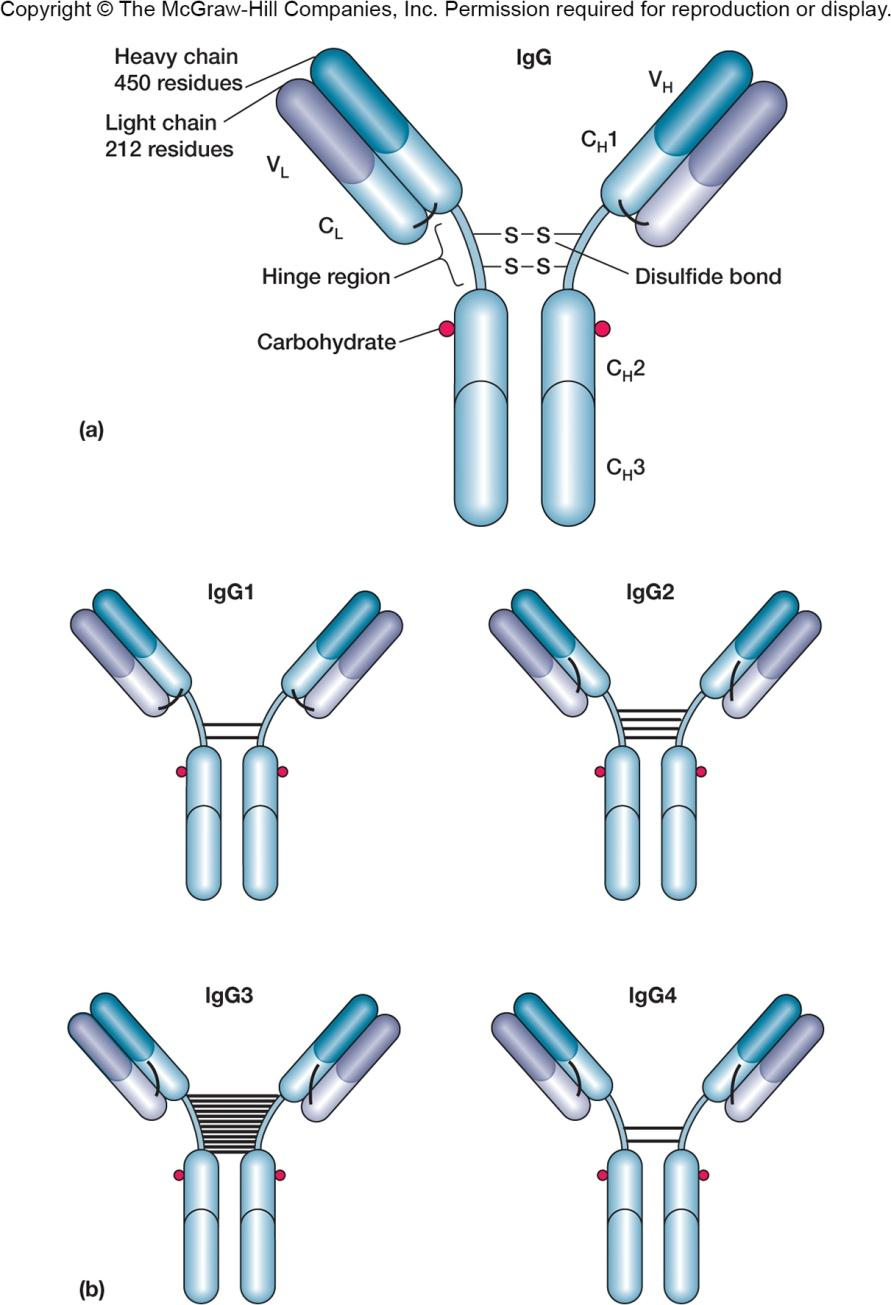
igG
- 80% of serum immunoglobulin
- opsonization, neutralization, activates complement
- only Ig that can cross the placenta
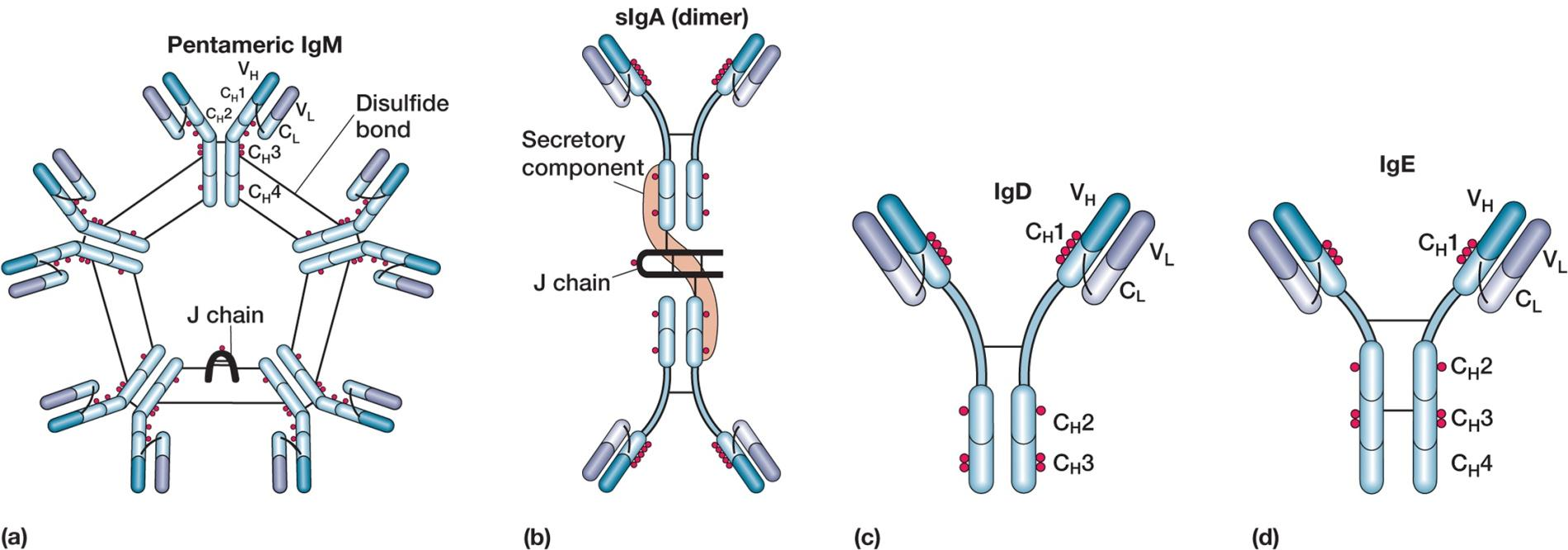
igD
- part of the BCR complex
- signals B cells to startantibody production
igM
- pentamer arranged in pinwheel
- first Ig in all immune responses
- agglutination, activates complement
IgA
- monomers and dimers
- secreted across mucosal surfaces
- tears, saliva, breast milk, MALT
- immune exclusion
igE
lowest Ig serum level, elevated in parasitic infection and allergic reactions
opsonization
mast cells bind Fc portion, activated when Fab portion binds allergens
4. Antibody Production and Kinetics
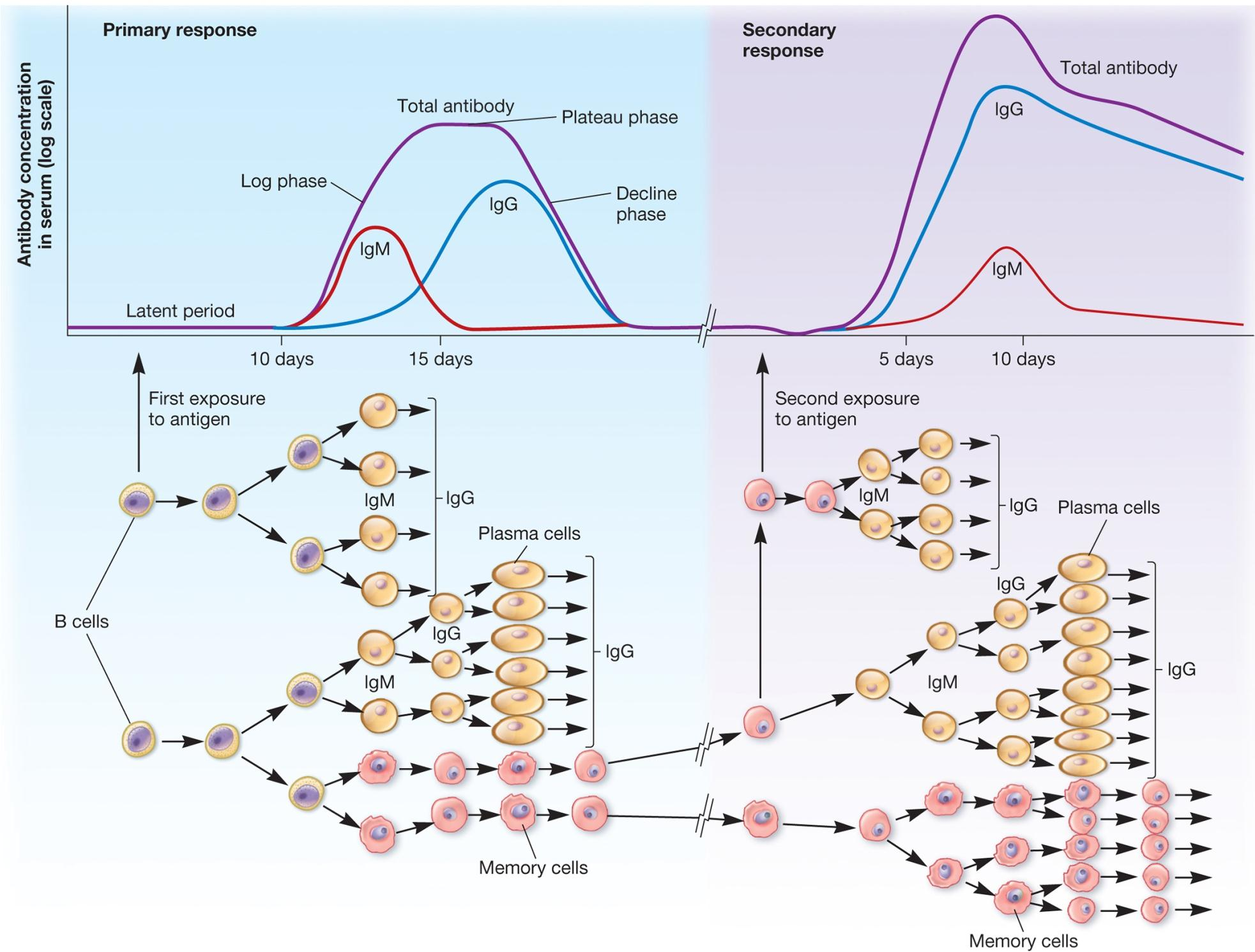
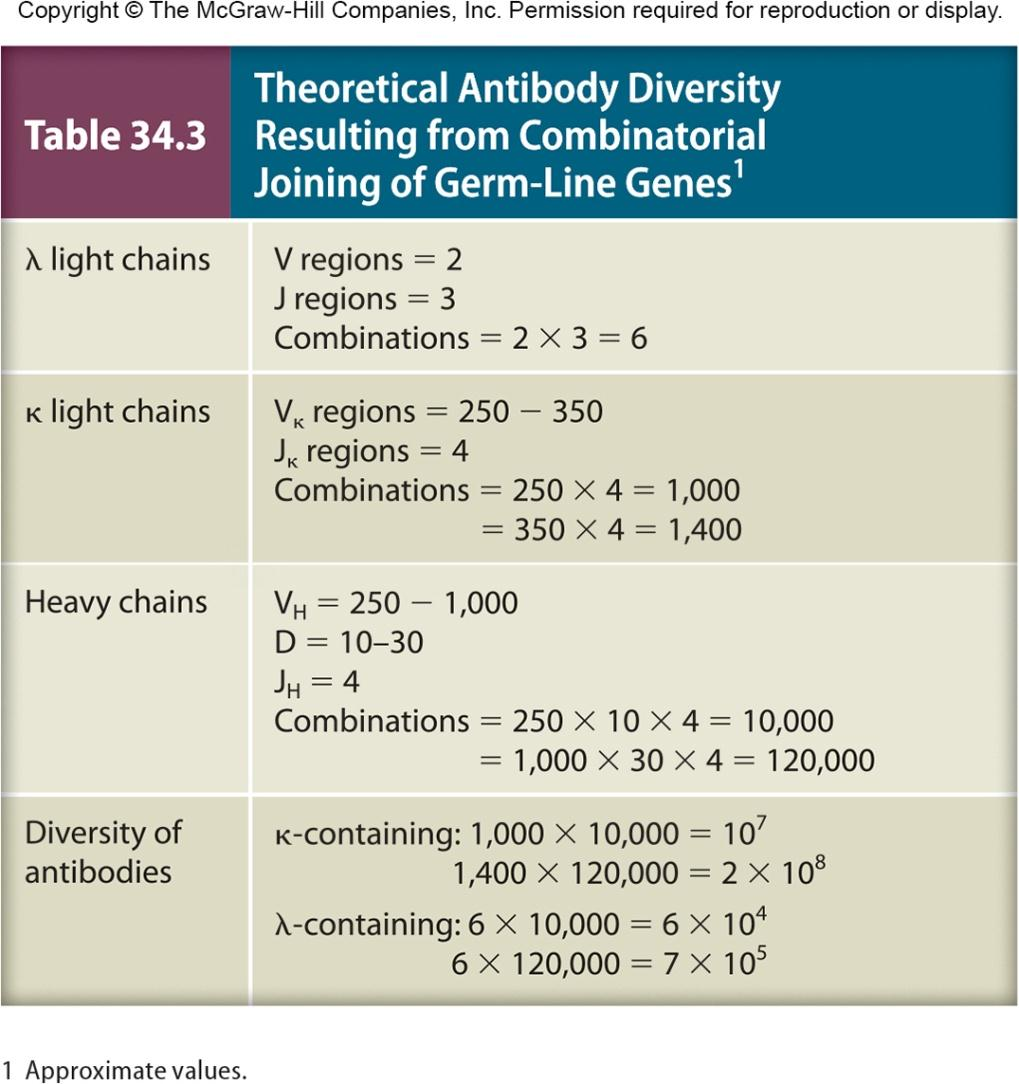
5. Diversity of Antibodies
Major mechanisms contribute to generation of antibody diversity
- rearrangement of antibody gene segments
- somatic mutation 体细胞突变
Light Chain
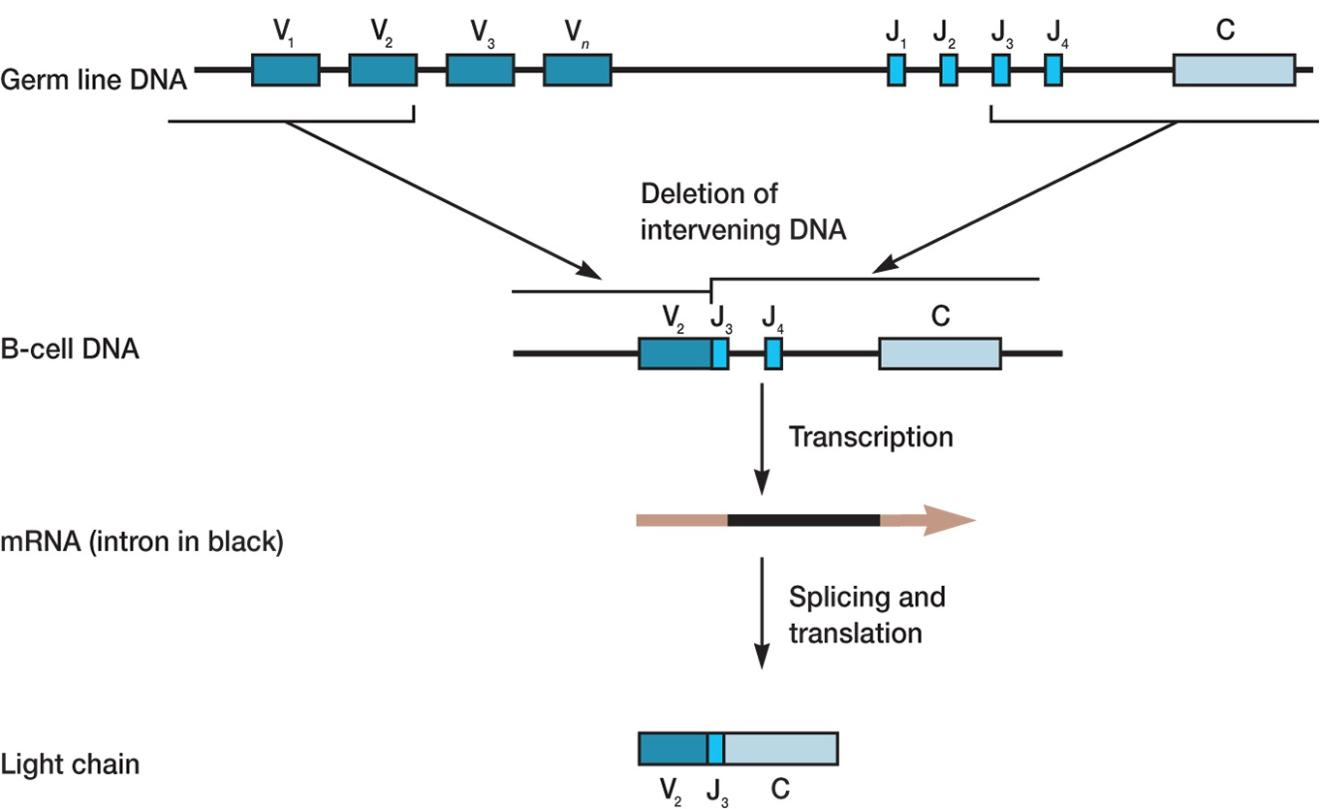
Germ line DNA for light chain contains multiple coding sequences, V and J (joining)
- one V is joined with one J region
- many possible combinations formed
- VJ joined with C (constant) exon after transcription
Heavy Chain
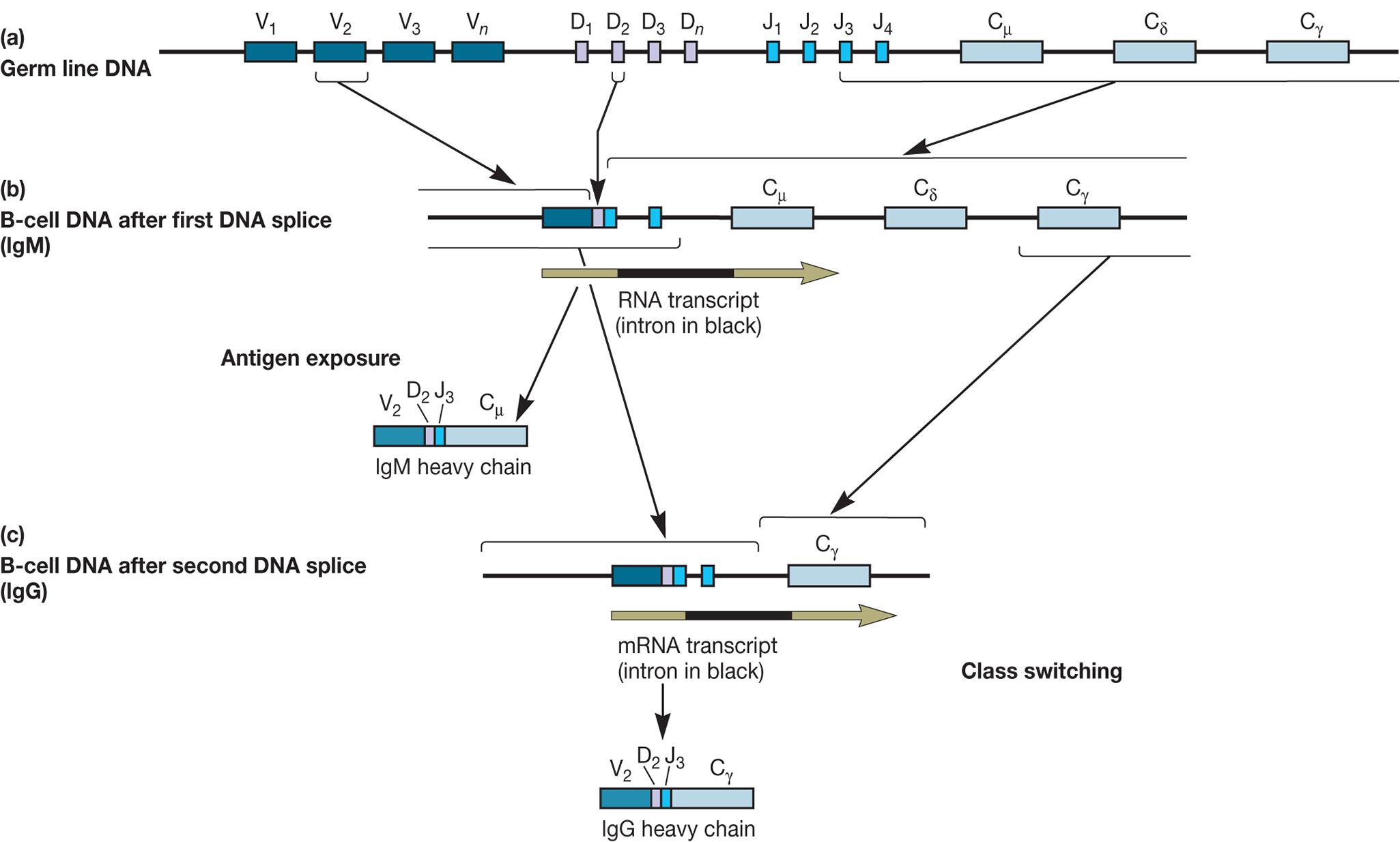
6. Antibody Diversity
Somatic mutation of V regions
- V regions are susceptible to high rate of somatic mutation during an antigen challenge
- produce antibodies with different epitope ( 表位;抗原决定部位,抗原决定基) recognition
Clonal Selection Theory
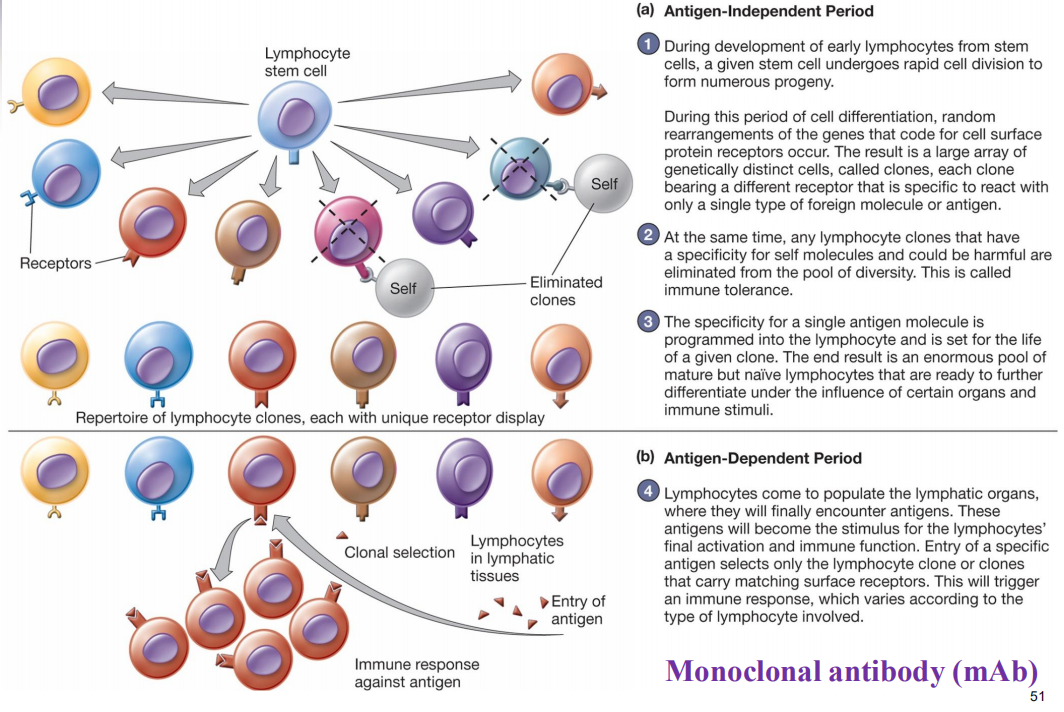
Antigen-Independent Period
During development of eariy lymphocytes from stem cells, a given stem cell undergoes rapid cell division to form numerous progeny.
During this period of cell differentiation, random rearrangements of the genes that code for cell surface protein receptors occur. The result is a large array of genetically distinct cells, called clones, each clone bearing a different receptor that is specific to react wfth only a single type of foreign molecule or antigen.At the same time, any lymphocyte clones that have a specificity for self molecules and could be harmful are eliminated from the pool of diversity. This is called immune tolerance.
The specificity for a single antigen molecule is programmed into the lymphocyte and is set for the life of a given clone. The end result is an enormous pool of mature but naive lymphocytes that are ready to further differentiate under the influence of certain organs and immune stimuli.
Antigen-Dependent Period
Lymphocytes come to populate the lymphatic organs, where they will finally encounter antigens. These antigens will become the stimulus for the lymphocytes final activation and immune function. Entry of a specific antigen selects only the lymphocyte clone or clones that carry matching surface receptors. This will trigger an immune response, which varies according to the type of lymphocyte Involved.
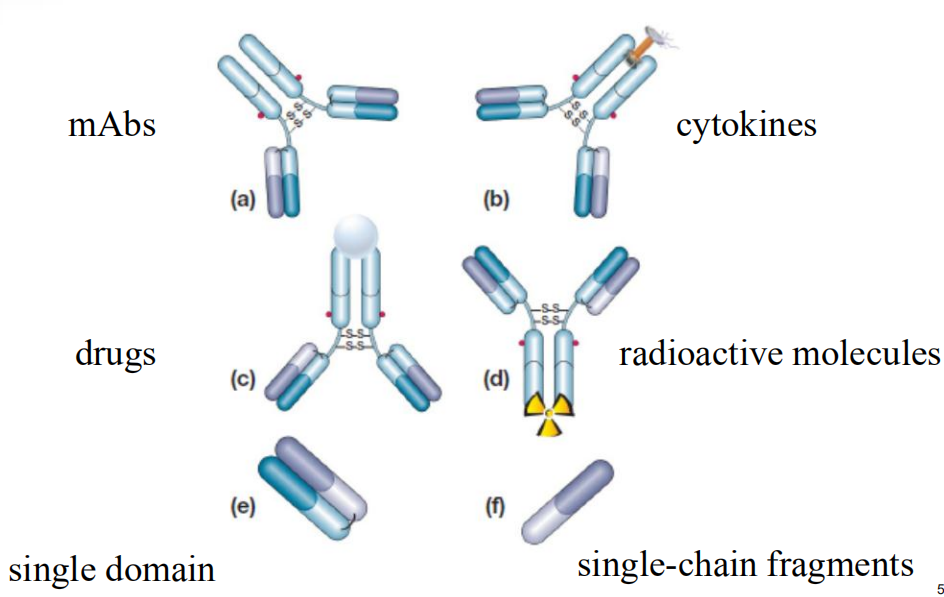
7. Monoclonal Antibody Therapeutics
8. Action of Antibodies
- Precipitation
- Neutralization
- Complement fixation
- Opsonization
- Agglutination
Acquired Immune Tolerance
How do we ‘know’ to respond to foreign but not self antigens?
Proposed mechanisms
- Negative selection of autoreactive lymphocytes
- Central tolerance
- Induction of anergy (peripheral tolerance)
- Partial or incomplete stimulation (no 2nd signal)
- Inhibition of anti-self reactivity by Treg cell activity and cytokine release
四、Immune Disorders
Hypersensitivities 超敏反应
Autoimmune diseases
Transplantation (tissue) rejection
Immunodeficiencies
congenital (先天的,天生的)
acquired
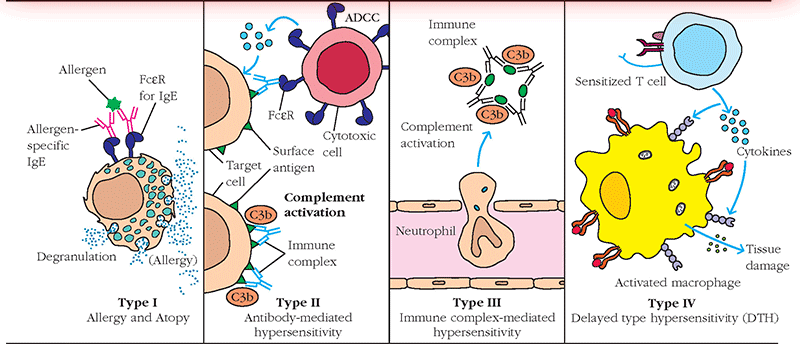
Hypersensitivities 超敏反应
Exaggerated immune response upon second or subsequent contact with antigen
Four different types of hypersensitivity: I,II, III, and IV
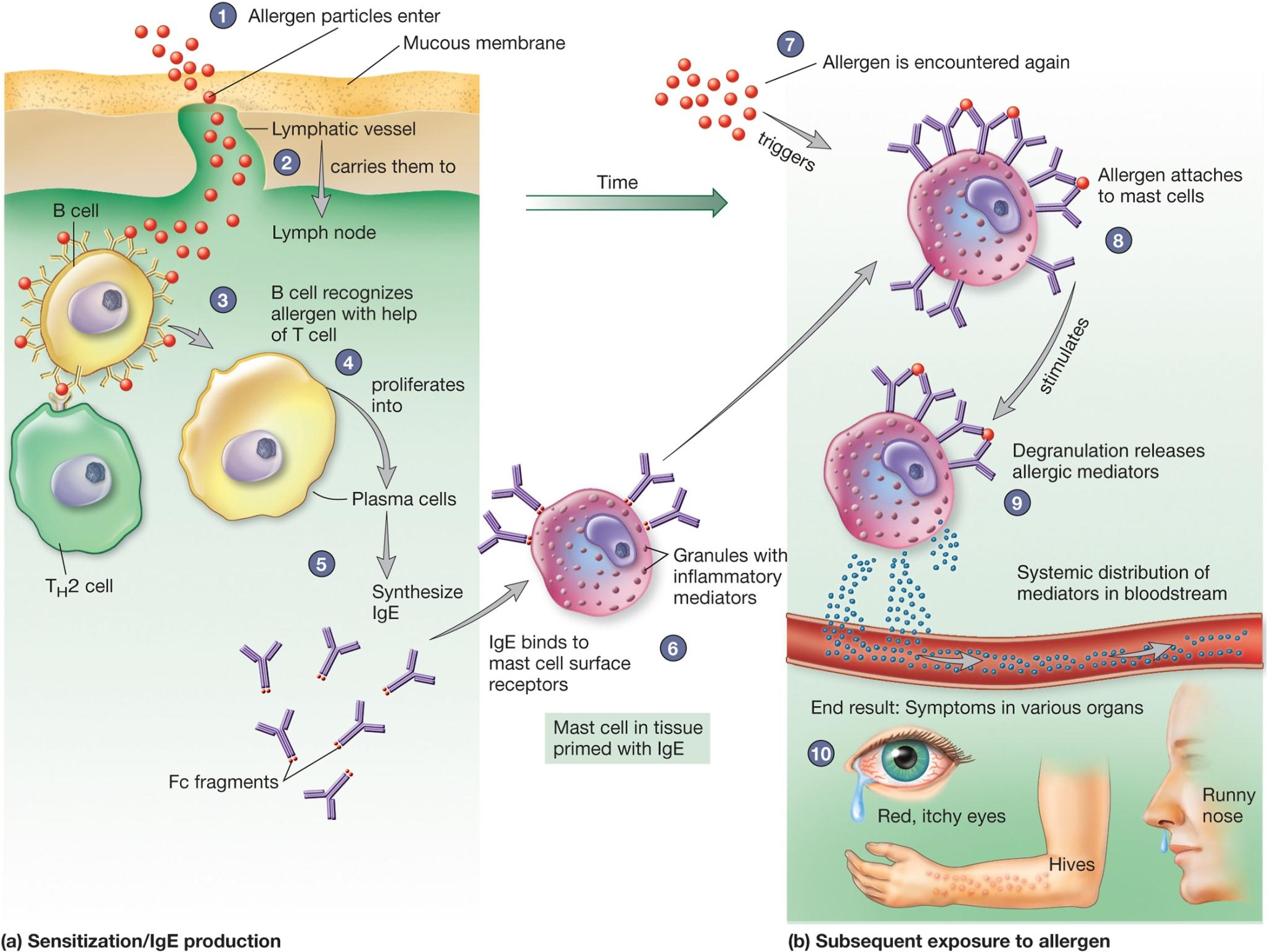
1. Type I Hypersensitivity
Allergy (对食物、花粉、虫咬等的)过敏症
- one kind of Type I hypersensitivity
Occurs immediately following second contact with allergen
Involves production and action of IgE and mast cells
- basophils or eosinophils may be involved as well
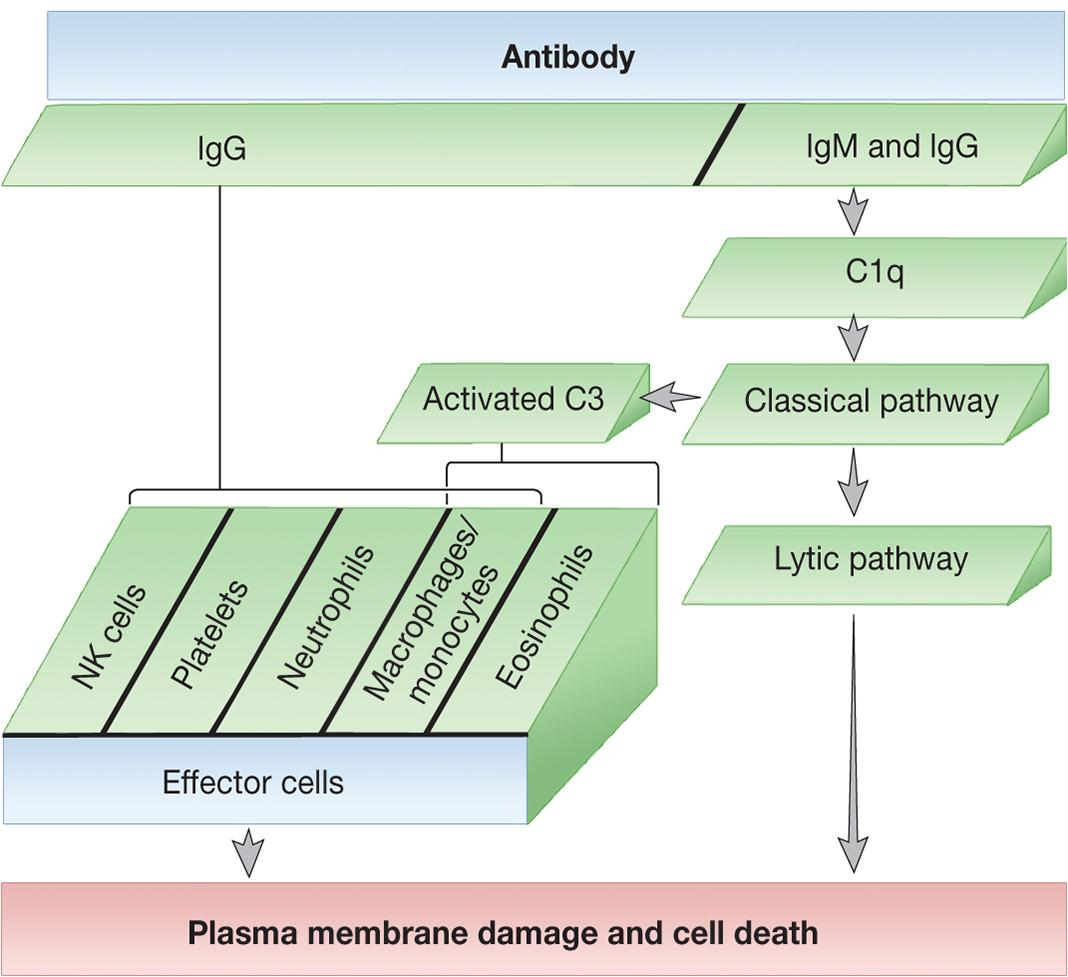
2. Type II Hypersensitivity
Involves IgG and IgM antibodies
- stimulate complement pathway and effector cells
Example: ABO Blood Group
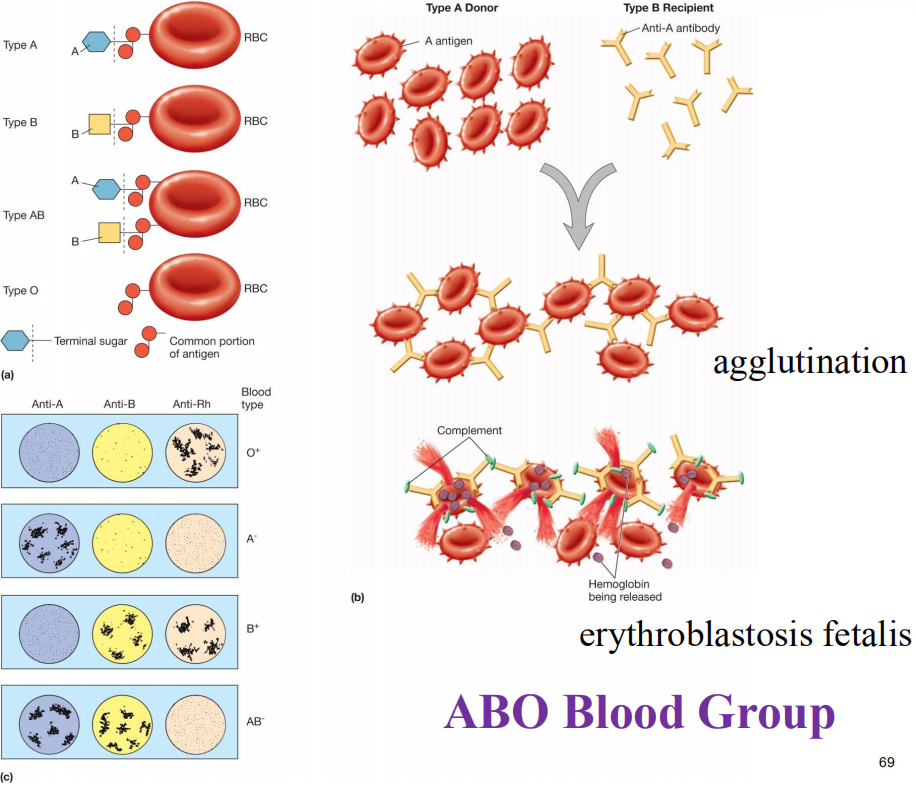
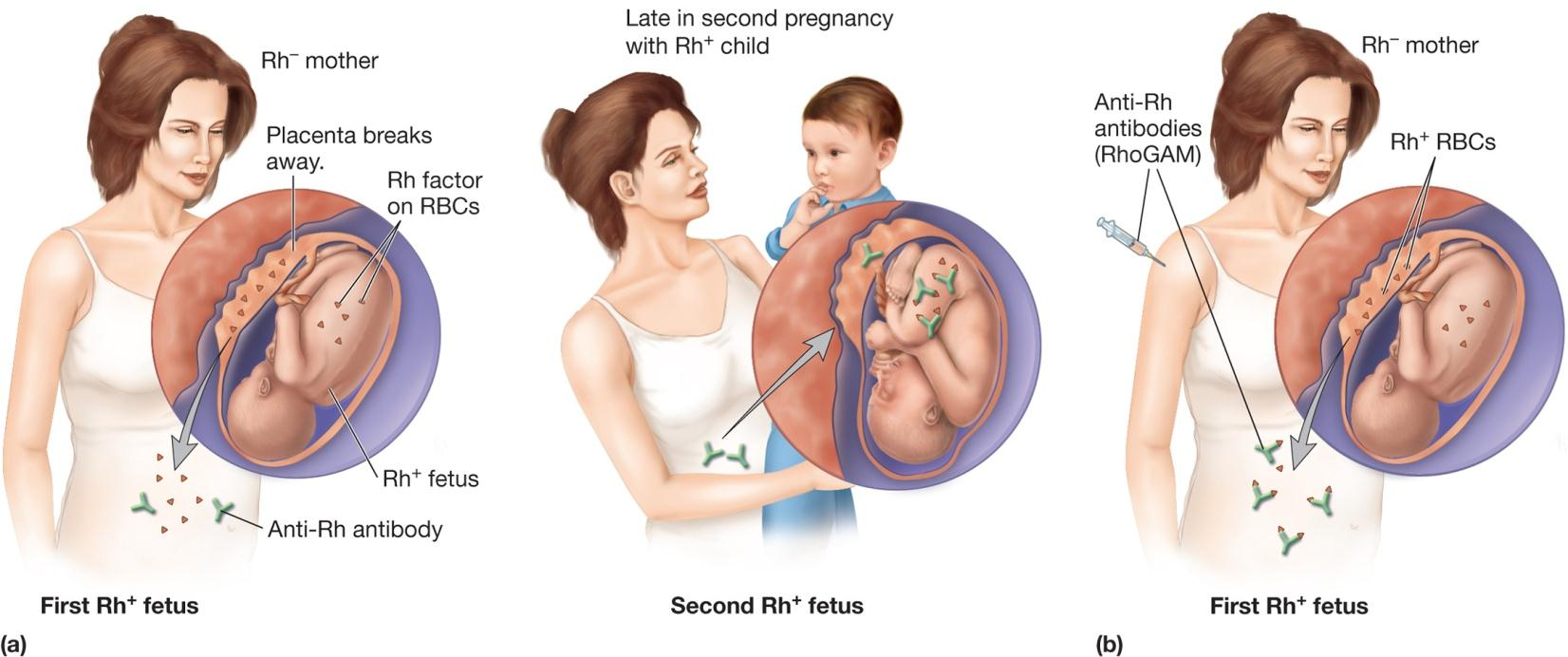
(1) Rh Incompatibility
Erythroblastosis fetalis [医]胎儿成红细胞增多病,新生儿溶血症
– mother can be passively injected with anti Rh factor antibodies or RhoGam to control this disease
3. Type III Hypersensitivity
Involves formation of immune complexes
usually removed by monocytes and macrophages
if accumulate, leads to hypersensitivity reaction
e.g., arthritis (关节炎) and systemic lupus erythematosis (系统性红斑狼疮)
4. Type IV Hypersensitivity
Involves delayed, cell-mediated immune reactions
T cells, monocytes, and macrophages
Examples
- transplantation rejection 移植排斥
- some autoimmune diseases 部分自身免疫性疾病
- cancer cell killing
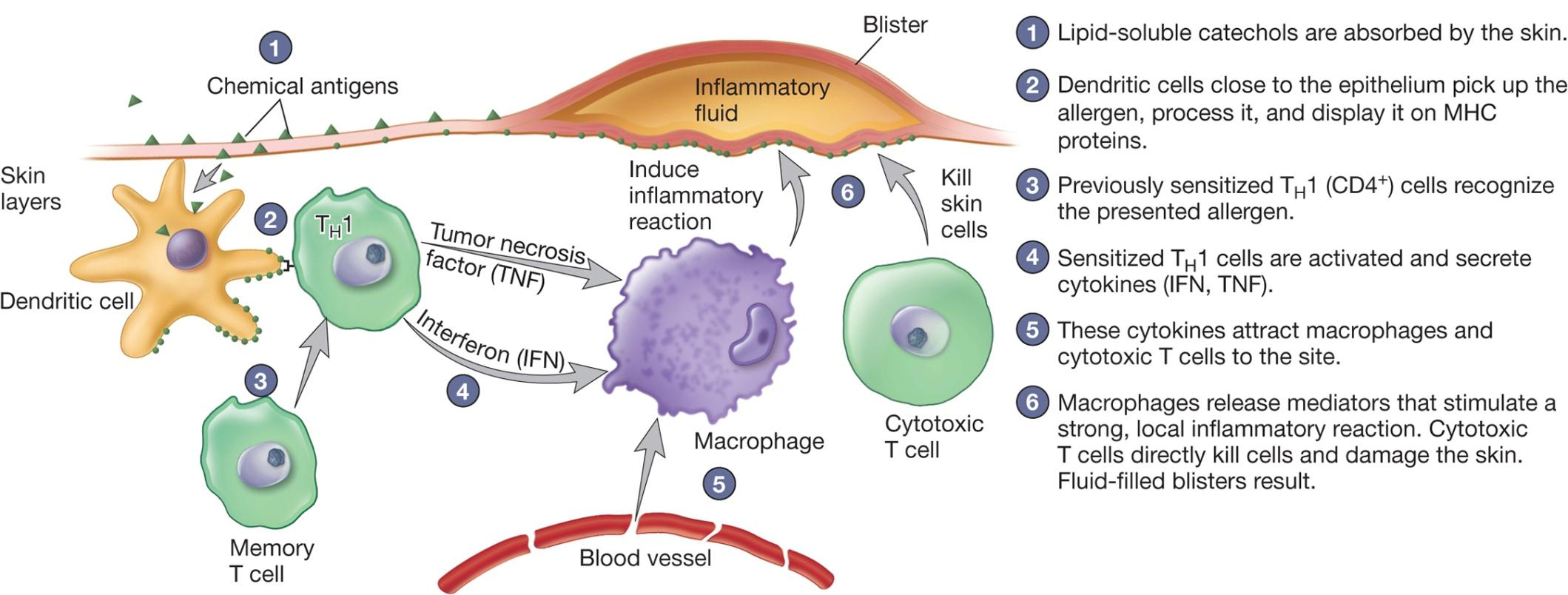
- allergic contact dermatitis 过敏性接触性皮炎
contact dermatitis
- Lipid-soluble catechols(邻苯二酚) are absorbed by the skin.
- Dendritic cells close to the epithelium pick up the allergen, process it, and display it on MHC proteins.
- Previously sensitized TH1 (CD4+) cells recognize the presented allergen.
- Sensitized TH1 cells are activated and secrete cytokines (IFN, TNF).
- These cytokines attract macrophages and cytotoxic T cells to the site.
- Macrophages release mediators that stimulate a strong, local inflammatory reaction. Cytotoxic T cells directly kill cells and damage the skin. Fluid-filled blisters result.
5. Summary
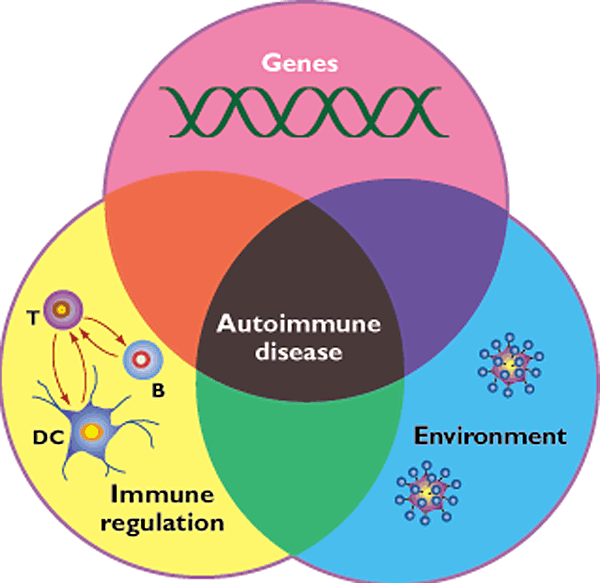
Autoimmune Diseases 自身免疫性疾病
Autoimmunity
- presence of serum antibodies that react with self antigens (autoantibodies)
- natural consequence of aging
- induced by numerous stimuli (e.g., mutation, infection, drugs)
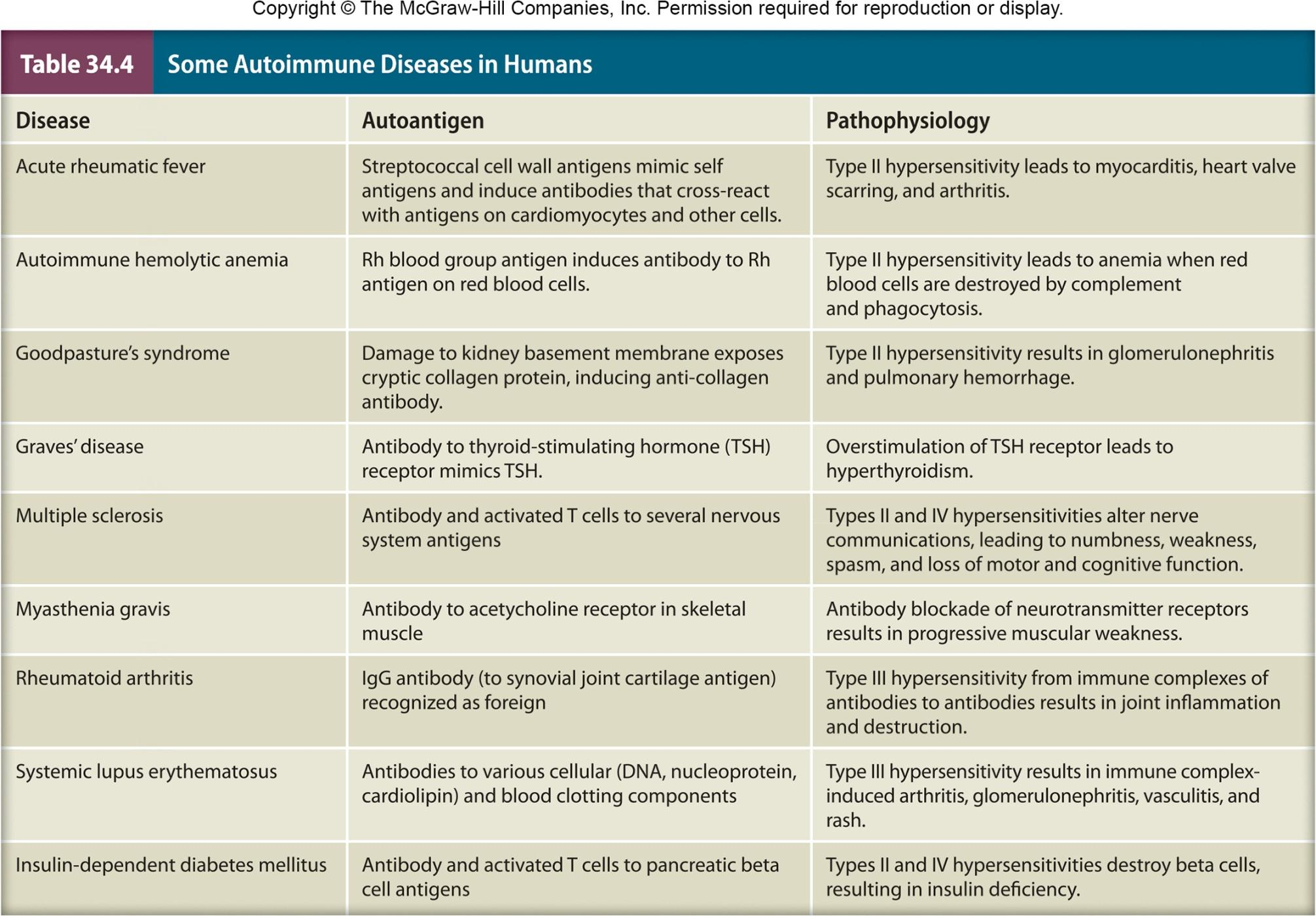
| Disease | Autoantigen | Pathophysiology |
|---|---|---|
| Acute rheumatic fever | Streptococcal cell wall antigens mimic self antigens and induce antibodies that cross-react with antigens on cardiomyocytes and other cells. | Type II hypersensitivity leads to myocarditis, heart valve scarring, and arthritis. |
| Autoimmune hemolytic anemia | Rh blood group antigen induces antibody to Rh antigen on red blood cells. | Type II hypersensitivity leads to anemia when red blood cells are destroyed by complement and phagocytosis. |
| Goodpasture’ s syndrome | Damage to kidney basement membrane exposes cryptic collagen protein, inducing anti-collagen antibody. | Type II hypersensitivity results in glomerulonephritis and pulmonary hemorrhage. |
| Graves’ disease | Antibody to thyroid-stimulating hormone (TSH) receptor mimics TSH. | Overstimulation ofTSH receptor leads to hyperthyroidism. |
| Multiple sclerosis | Antibody and activated T cells to several nervous system antigens | Types II and IV hypersensitivities alter nerve communications, leading to numbness, weaknessz spasm, and loss of motor and cognitive function. |
| Myasthenia gravis | Antibody to acetycholine receptor in skeletal muscle | Antibody blockade of neurotransmitter receptors results in progressive muscular weakness. |
| Rheumatoid arthritis | IgG antibody (to synovial joint cartilage antigen) recognized as foreign | Type III hypersensitivity from immune complexes of antibodies to antibodies results in joint inflammation and destruction. |
| Systemic lupus erythematosus | Antibodies to various cellular (DNA, nucleoprotein, cardiolipin) and blood clotting components | Type III hypersensitivity results in immune complex- induced arthritis, glomerulonephritis, vasculitis, and rash. |
| Insulin-dependent diabetes mellitus | Antibody and activated T cells to pancreatic beta cell antigens | Types II and IV hypersensitivities destroy beta cells, resulting in insulin deficiency. |
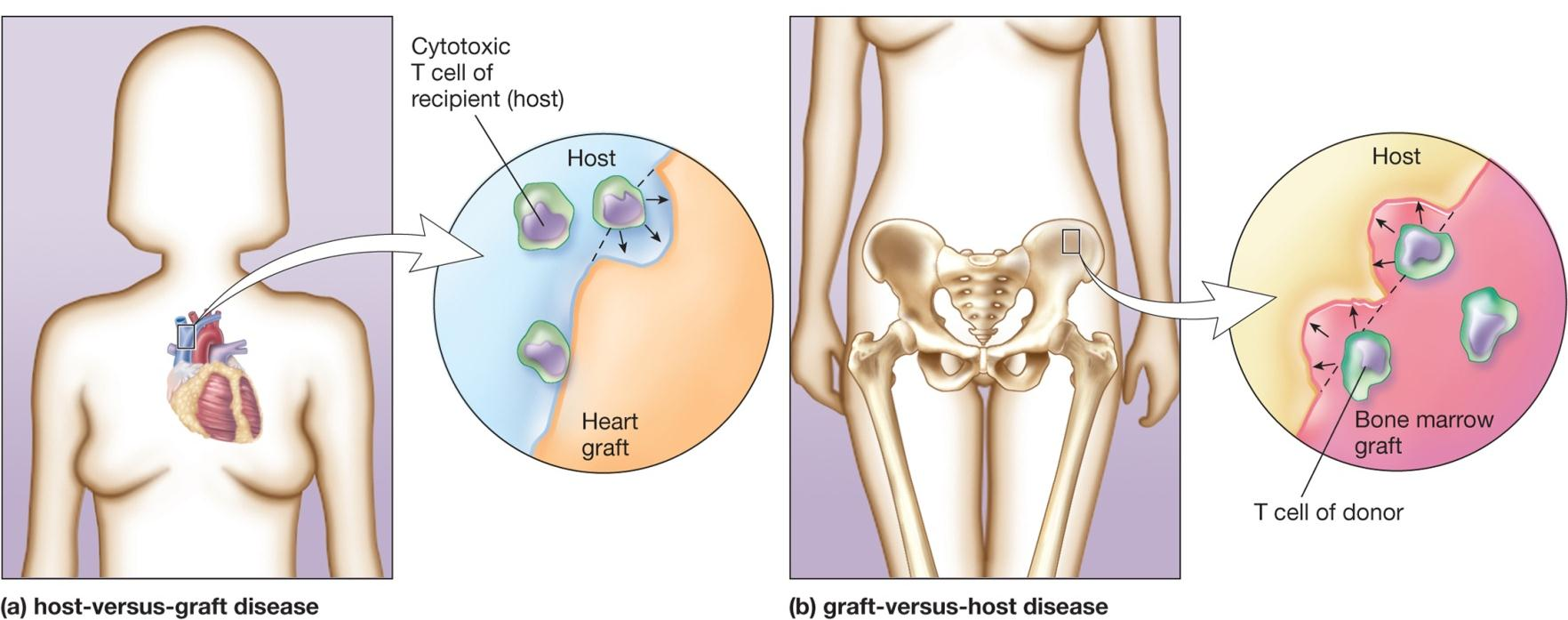
Transplantation (Tissue) Rejection 移植(组织)排斥
Types of transplants
**allograft ** (同种)异基因移植物
- transplants between different individuals within a species
xenograft 异种移植物
- donor and recipient are different species
Mechanisms can occur
- MHC molecules (HLA) on transplanted tissue — host Th cells → Tc cells and macrophage
1. Tissue Transplantation
To be successful, the ABO blood group and the MHC molecules of the donor and recipient must be as closely matched as possible
- family members are the first choice
2. Graft-Versus-Host Disease 移植物抗宿主病
Immune cells in donor tissue reject host
e.g., in bone marrow transplants
- disease prevented by treating donor with immunosuppressive drugs
3. Immunodeficiency
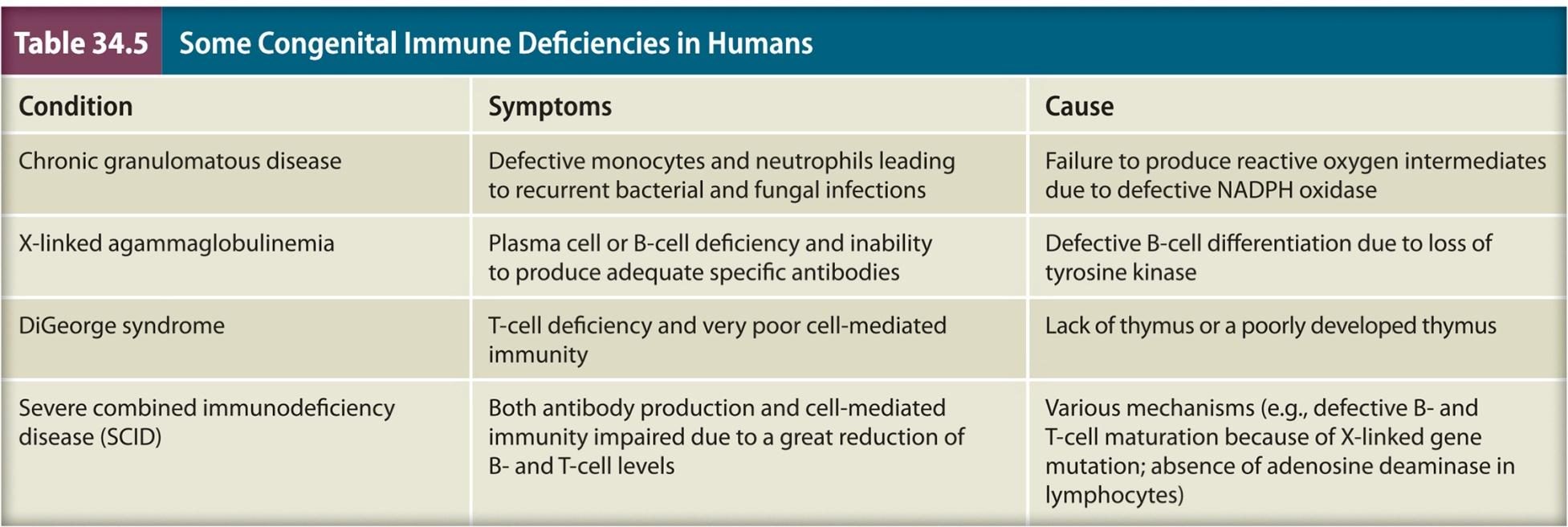
| Condition | Symptoms | Cause |
|---|---|---|
| Chronic granulomatous disease | Defective monocytes and neutrophils leading to recurrent bacterial and fungal infections | Failure to produce reactive oxygen intermediates due to defective NADPH oxidase |
| X-llnked agammaglobulinemia | Plasma cell or B-cell deficiency and Inability to produce adequate specific antibodies | Defective B-cell differentiation due to loss of tyrosine kinase |
| DiGeorge syndrome | T-cell deficiency and very poor cell-mediated immunity | Lack of thymus or a poorly developed thymus |
| Severe combined immunodeficiency disease (SCID) | Both antibody production and cell-mediated Immunity impaired due to a great reduction of B- and rcell levels | Various mechanisms (e.g., defective B- and T-cell maturation because of X-linked gene mutation; absence of adenosine deaminase in lymphocytes) |
Failure to recognize and/or respond to foreign Ag
Primary (congenital) immunodeficiency
- result from genetic disorder
Acquired immunodeficiency
- result from infection (e.g., HIV)