L16 Antidiabetic Drugs
一、The Pancreas
An organ that makes insulin and enzymes for digestion (excorine function).
Both endocrine system and digestive system (exocrine)
Pancreatic islet cells and their secretory products
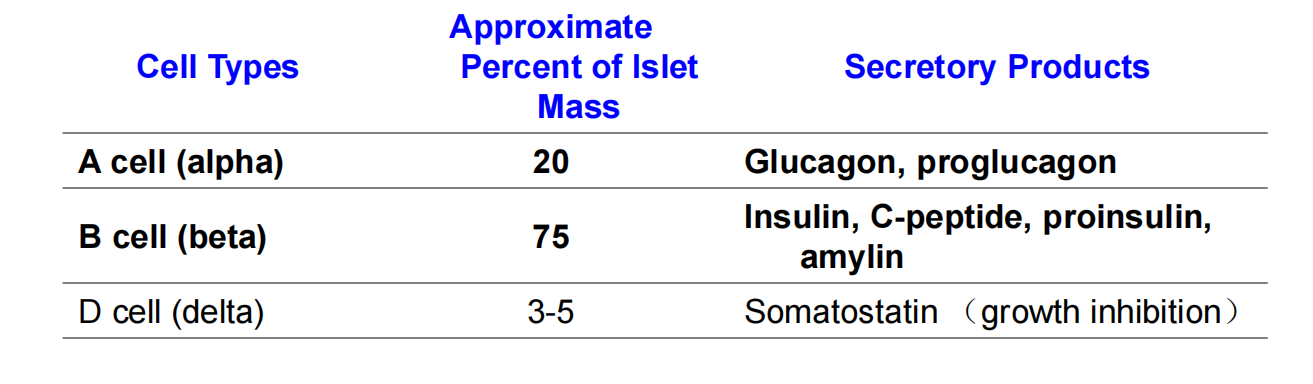
- Insulin: the storage and anabolic hormone of the body (glycometabolism)
- Amylin: modulates appetite, gastric emptying, and glucagon and insulin secretion
- Glucagon: the hyperglycemic factor that mobilizes glycogen stores
Disorders of the Pancreas: Diabetes Mellitus
Caused by:
- Insufficient secretion of insulin
- Resistance of body cells to the effects of insulin

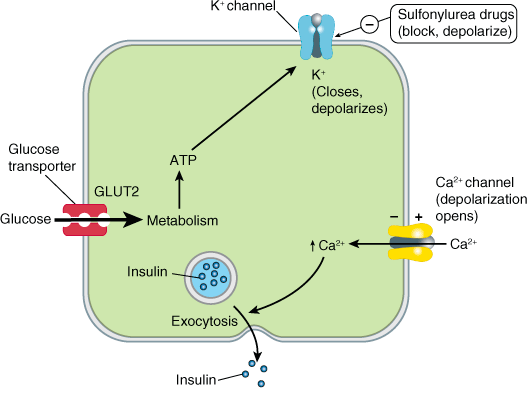
One model of control of insulin release from the pancreatic B cell
Insulin-induces glucose uptake in muscle, fat, liver, and brain
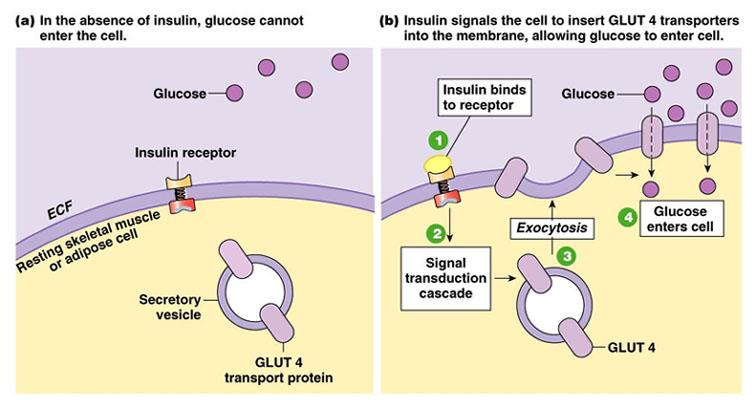
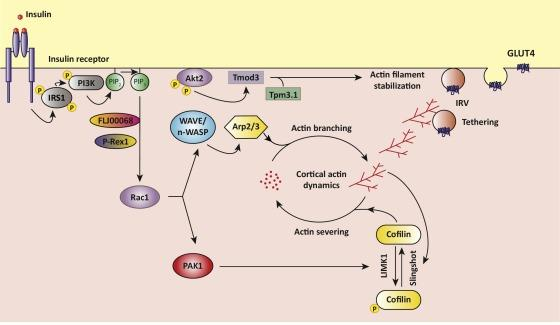
Insulin induces glucose transporter (Glut) surface relocation
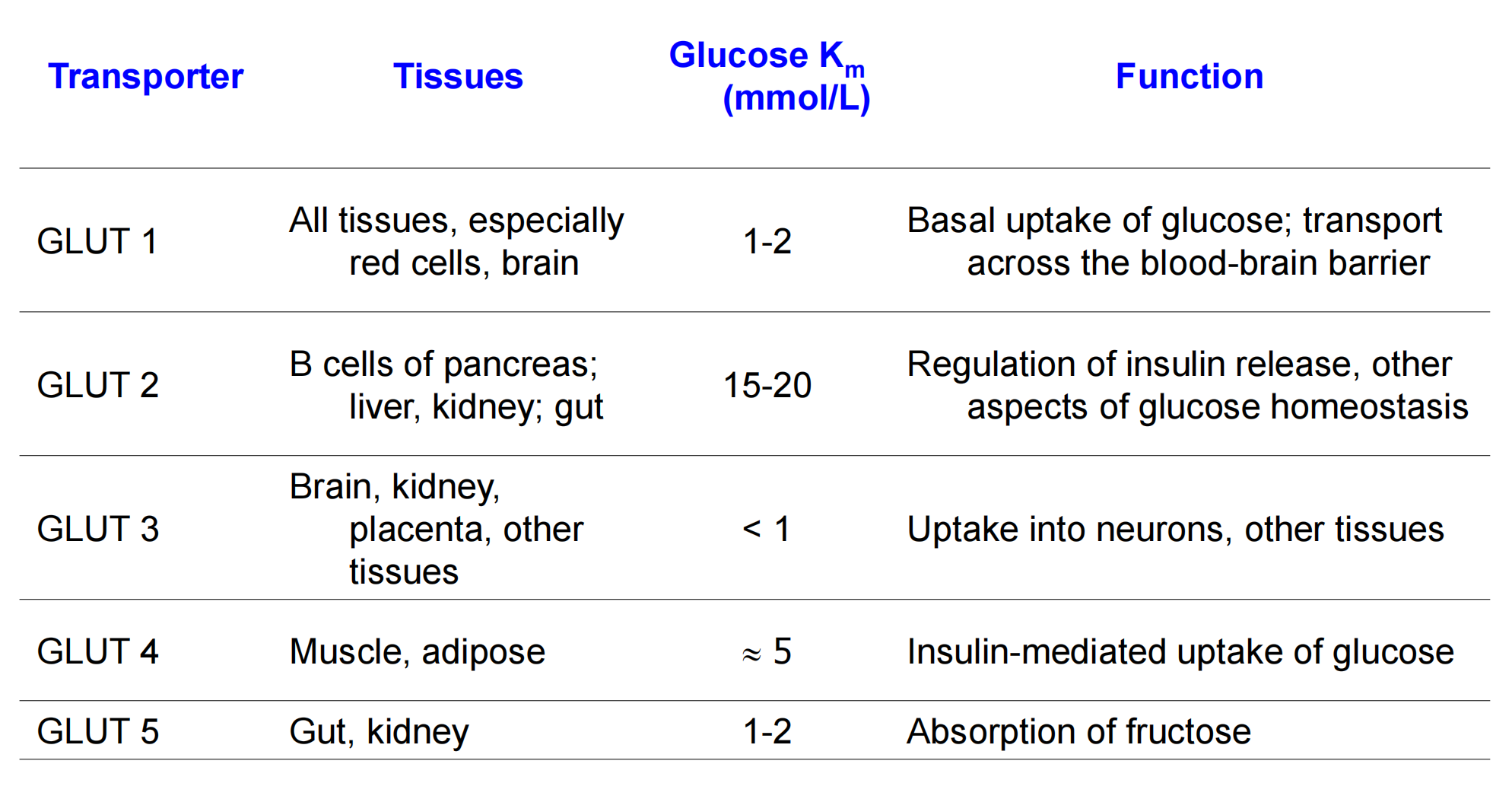
Glucose transporters (GLUT)
Insulin promotes glycogen synthesis and storage
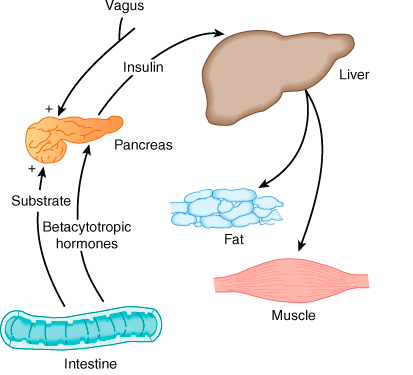
1. Endocrine effects of insulin
Effect on liver:
- Inhibits glycogenolysis
- Inhibits conversion of fatty acids and amino acids to Acetyl-CoA
Anabolic action
- Promotes glucose storage as glycogen (induces glucokinase and glycogen synthase, inhibits phosphorylase)
- Increases triglyceride synthesis and very-low-density lipoprotein formation
Effect on muscle:
- Increased protein synthesis
- Increases amino acid transport
- Increases ribosomal protein synthesis
- Increased glycogen synthesis
- Increases glucose transport
- Induces glycogen synthase and inhibits phosphorylase
Effect on adipose tissue:
- Increased triglyceride storage
- Glucose transport into cell provides glycerol phosphate to permit esterification of fatty acids supplied by lipoprotein transport
- Intracellular lipase is inhibited by insulin
二、Diabetes Mellitus
Types
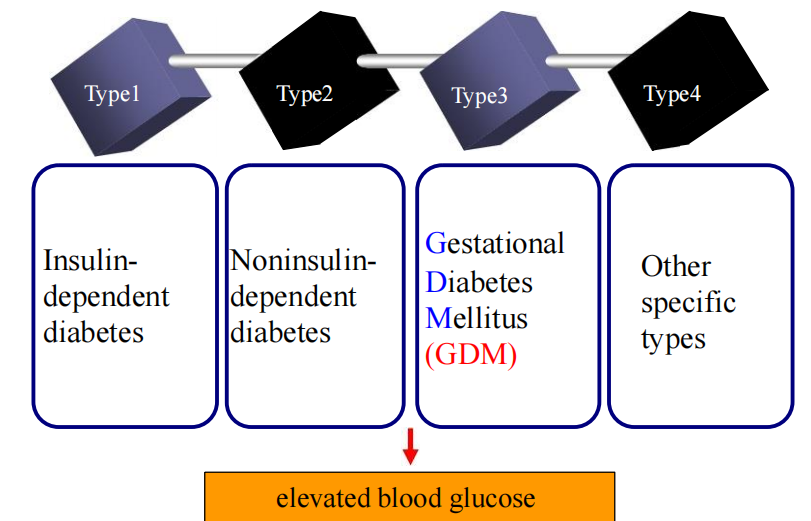
1. TypeⅠ Diabetes
develops suddenly, usually before age 15
- results in insulin dependence
- severe or absolute insulin deficiency
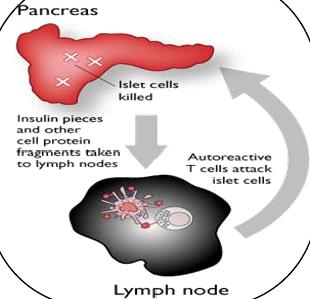
- Type I diabetes occurs when insulin producing cells are destroyed by the body’s own immune system
2. Treatment of Type Ⅰ Diabetes
Injection of insulin
Surgery: replacing the pancreas or just the beta cells
- pancreas-kidney transplant
- Stem cell research
3. Type Ⅲ Diabetes – GDM
Gestational diabetes mellitus (GDM, 妊娠期糖尿病) is a condition in which women without previously diagnosed diabetes exhibit high blood glucose levels during pregnancy
Most patients are treated only with diet modification and moderate exercise but some take anti-diabetic drugs, including insulin therapy.
4. Type Ⅳ Diabetes
Other specific types
Drug-induced diabetes :
- 1992, anti-hypertensive vasodilator diazoxide, and corticosteroids in high doses could cause diabetes.
- 2006, antipsychotic drugs: Olanzapine: induces hyperinsulinemia. dozens of those patients died from diabetes-related complications.
5. Type Ⅱ Diabetes
adult onset, usually occurs after age 40
Etiology: Insulin resistance; relative deficiency in insulin secretion (late stage).
blood glucose levels rise due to :
- Lack of insulin production
- Insufficient insulin action (resistant cells)
6. Treatment of TypeⅡ Diabetes
Drugs
Oral hypoglycemic agent = OHA
OHA s + Insulin therapy
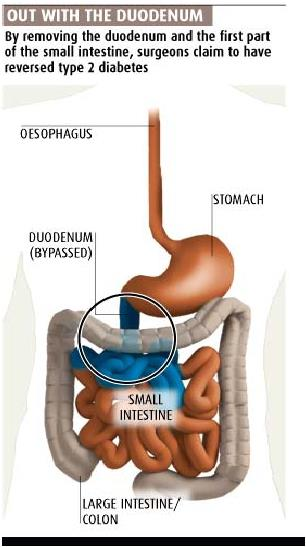
Surgery
Surgery: Type 2 diabetes can be cured gastric bypass surgery in 80-100% of Severely obese patients
Treatment
Antidiabetic Drugs
- Insulin
- Insulin Secretagogues: Sulfonylureas; Meglitinides
- Insulin Sensitisers: Biguanides; Thiazolidinediones
- Alpha-glucosidase inhibitors
- Peptide analogs:
- Glucagon-like peptide (GLP) analogs
- DPP-4 inhibitors
- Amylin analogues
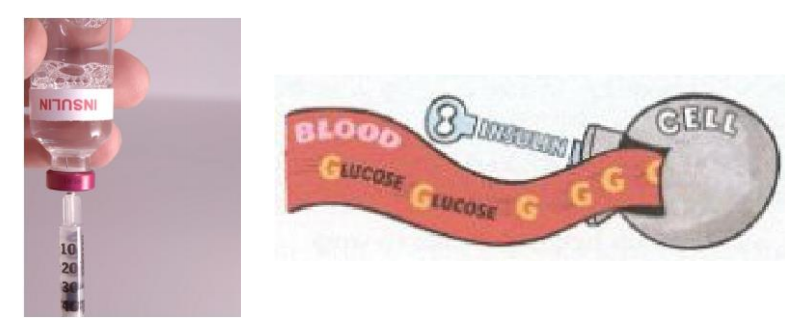
1. Insulin
Application
Diabetes mellitus type 1 is a disease caused by the lack of insulin
Insulin must be used in Type I, which must be injected or inhaled.
Pharmacological effects of insulin
- Decrease the blood glucose concentration (BGC)
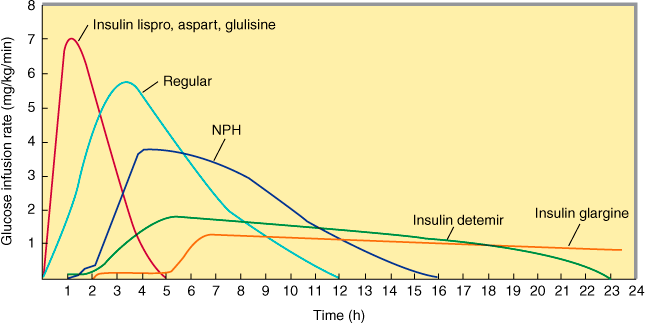
Insulin preparation
- Rapid-acting, Short-acting, Intermediate-acting, Long-acting
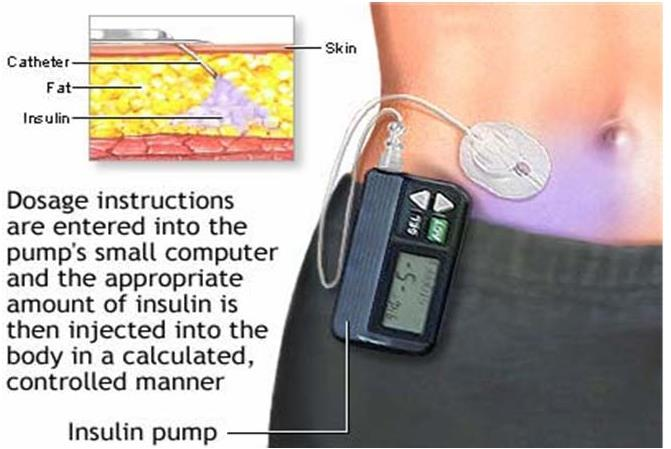
Delivery
Insulin Delivery System
- Regular injections (Subcutaneous)
- Portable pen injections
- Continuous subcutaneous insulin infusion devices (CSII, insulin pumps)
- Inhaled insulin
Portable pen injections
- It is an insulin injection tool that resembles a pen.
- This is great for people who need to give themselves an insulin injection when out in public but do not like it to be noticeable.
- The Insulin Pen also contains memory of your last 16 injections
Continuous Subcutaneous Insulin Infusion CSII
- Continuous infusion of a short-acting insulin driven by mechanical force and delivered via a needle or soft cannula under the skin.
Inhaled insulin
- Inhaled insulin is a powdered form of insulin absorbed by the lungs through use of a hand-held inhaler.
- Inhaled insulin is the first noninjectable option.
Complications of Insulin Therapy
Hypoglycemia
Immunopathology: Insulin allergy; Immune insulin resistance (potential vicious cycle)
Lipodystrophy (abnormal accumulation of fat tissue) at injection sites
Treatment of Hypoglycemia
- Glucagon
- A hormone produced by the alpha cells in the pancreas.
- It raises blood glucose.
- An injectable form of glucagon
2. Oral hypoglycemic agents
Insulin Secretagogues
Insulin Secretagogues: agents which increase the amount of insulin secreted
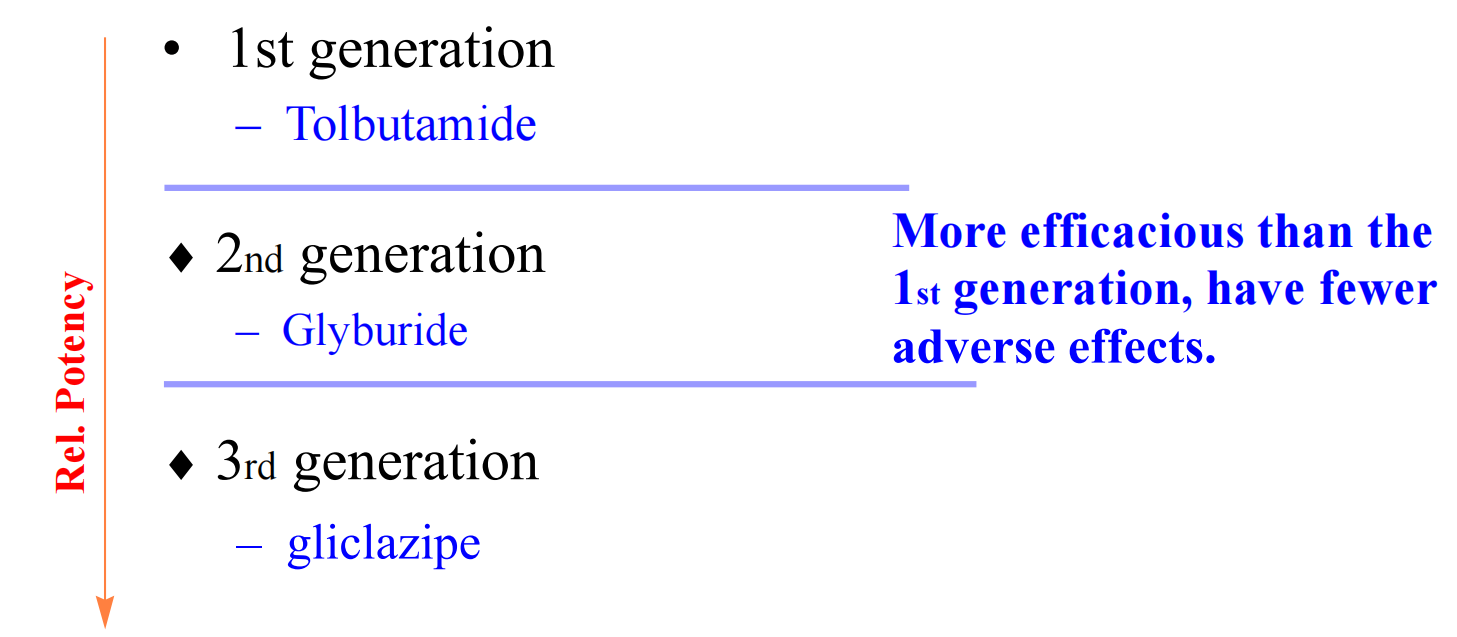
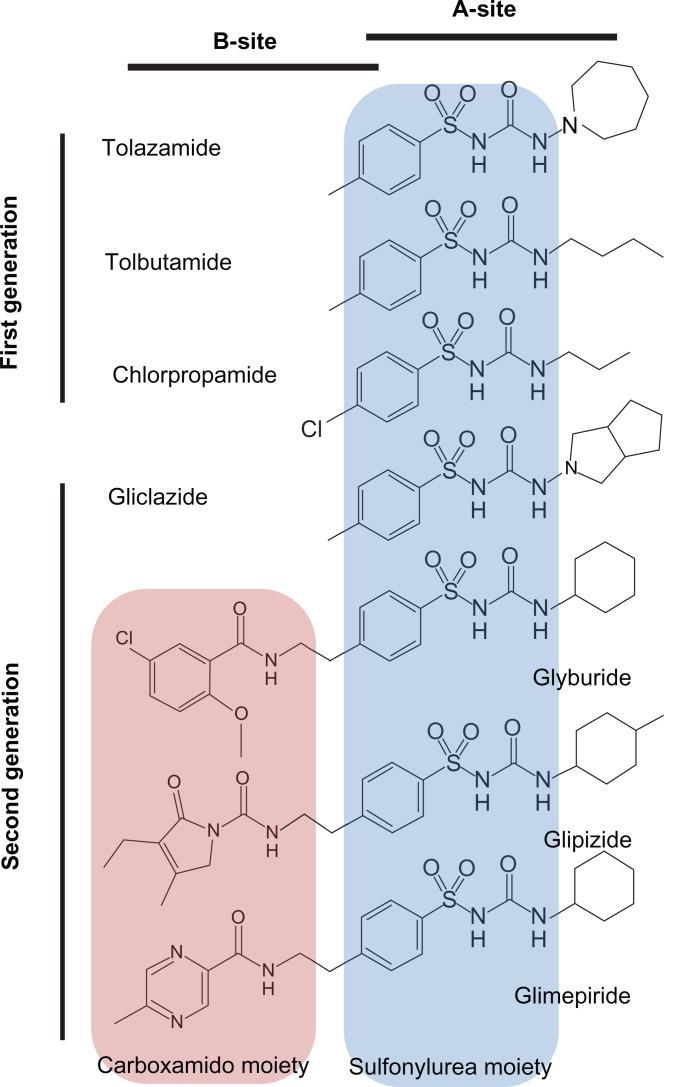
(1) Sulfonylureas (SU)
Sulfonylureas were the first widely used oral hypoglycemic medications
Mechanism of Action
trigger insulin release by direct action on the K channel of the pancreatic beta cells.
Therapeutic uses
Only useful in Type II diabetes
- They work best with patients over 40 years old, who have had diabetes mellitus for under ten years
Diabetes insipidus (large amount of urine)
- Chlorpropamide has also an antidiuretic effect and may be used to treat diabetes insipidus.
Adverse reactions
Serious adverse reaction is hypoglycemia
Common adverse effects: gastrointestinal reactions such as nausea and vomiting
(2) Meglitinides
Uses
Meglitinides help the pancreas produce insulin and are often called “short-acting secretagogues.”
Their mode of action is original, affecting potassium channels
By closing the potassium channels of the pancreatic beta cells, they open the calcium channels, hence enhancing insulin secretion.
They are taken with meals to boost the insulin response to each meal.
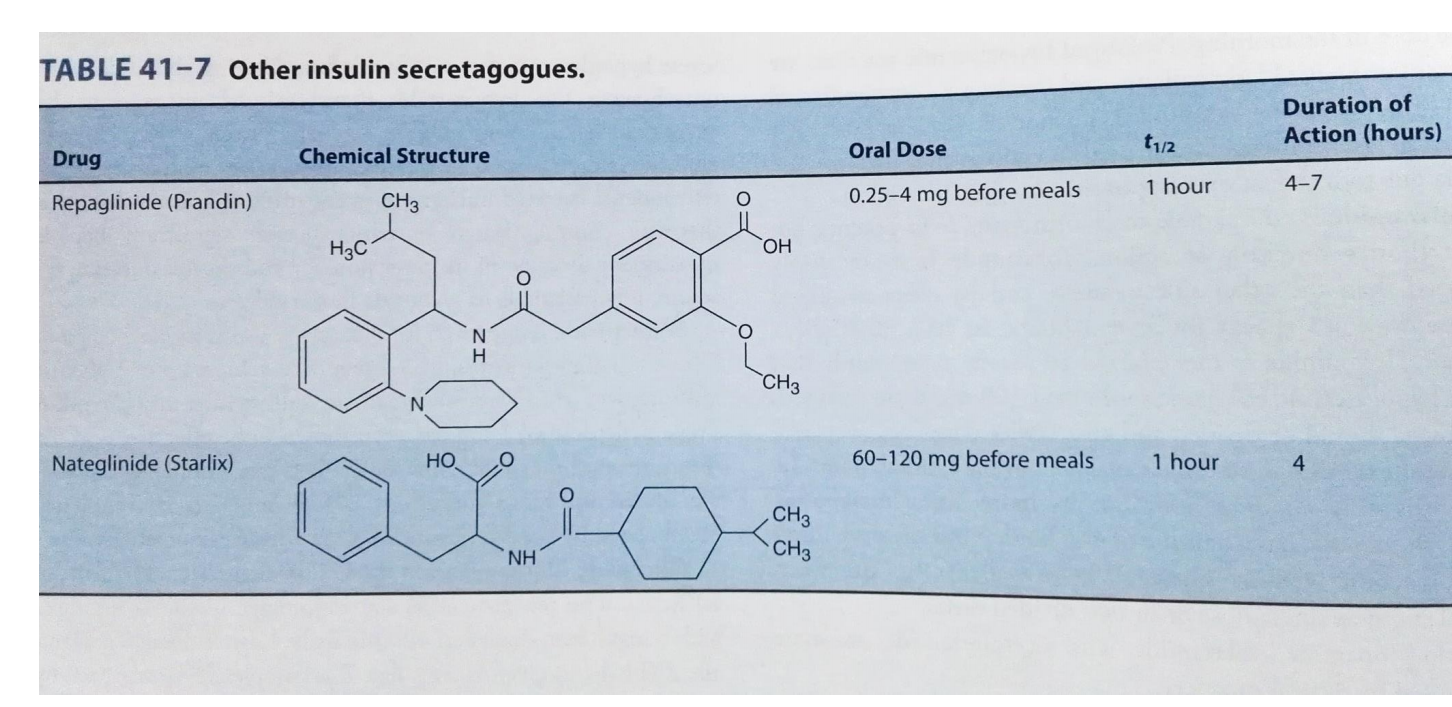
repaglinide (Prandin) The maximum dosage is 16 mg/day, taken 0 to 30 minutes before meals. If a meal is skipped, the medication is also skipped.
nateglinide (Starlix) The maximum dosage is 360 mg/day, usually 120 mg three times a day (TID).
Adverse reactions
weight gain
hypoglycemia
Insulin Sensitisers
Insulin Sensitisers: agents which increase the sensitivity of target to insulin
(1) Biguanides
Mechanism of action
- Direct stimulation of glycolysis in tissues, with increased glucose removal from blood
- inhibiting gluconeogenesis
- reducing the absorption of glucose from the intestine (influence on gut microbiota)

Therapeutic uses
Metformin is usually the first-line medication used for treatment of type-2 diabetes.
Adverse reactions
- The main adverse reactions of Phenformin are lactic acidosis (due to high glycolysis)
- The most frequent toxic effects of Metformin are gastrointestinal symptoms including nausea, vomiting, and diarrhea.
(2) Thiazolidinediones (TZDs)
Drugs
- Pioglitazone
- Rosiglitazone
- Ciglitazone
- Englitazone
- Troglitazone
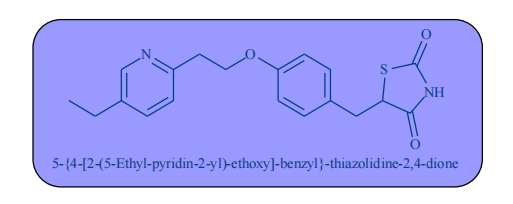
Mechanism of action
Enhance the target tissue’s sensitivity to insulin through PPARγ pathway
PPAR-γ is a type of nuclear regulatory proteins involved in transcription of genes regulating glucose and fat metabolism. These PPARs act on Peroxysome Proliferator Responsive Elements (PPRE). The PPREs influence insulin sensitive genes, which enhance production of mRNAs of insulin dependent enzymes. The final result is better use of glucose by the cells.
α-Glucosidase Inhibitors
Alpha-glucosidase inhibitors: agents which decrease the rate at which glucose is absorbed from the gastrointestinal tract.
(1) Acarbose
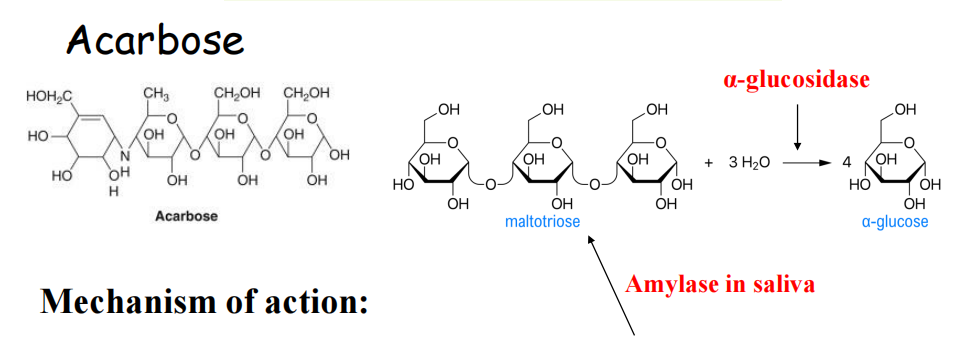
Mechanism of action
Reduces intestinal absorption of starch and dextrin by inhibiting the action of α-glucosidase in intestinal brush border.
Clinical use
The agents are effective by themselves only in the earliest stages of impaired glucose tolerance, but can be helpful in combination with other agents in type 2 diabetes
They do have the potential to cause weight loss by lowering the amount of sugar metabolized
Peptide analogs
Overview of insulin secretion
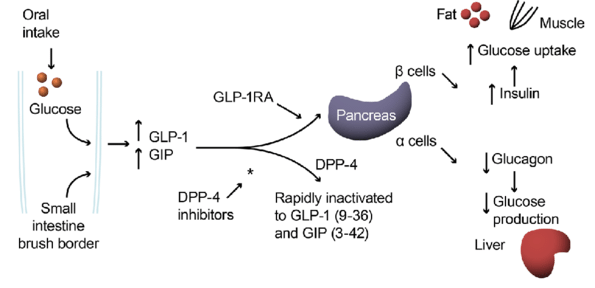
Incretin mimetics
- Incretins like GLP1 are insulin secretagogues
- The main candidate molecules that fulfill criteria for being an incretin are Glucagon-like peptide-1 (GLP-1)
- GLP-1 is rapidly inactivated by the enzyme dipeptidyl peptidase-4 (DPP-4).
(1) Glucagon-like peptide (GLP) analogs
- GLP agonists bind to a membrane GLP receptor.
- As a consequence of this, insulin release from the pancreatic beta cells is increased.
Exenatide (also Exendin-4, marketed as Byetta) is the first GLP agonist approved for the treatment of type 2 diabetes
It is an injectable medication. (liraglutide)
These agents may also cause a decrease in gastric motility, responsible for the common side effect of nausea, and is probably the mechanism by which weight loss occurs
(2) DPP-4 inhibitors
Sitagliptin
- an inhibitor of dipeptidyl peptidase-4 (DPP4), the enzyme that degrades incretin and other GLP-l-like molecules.
- increase blood concentration of the incretin GLP-1
- This drug appears likely to be approved for use in type 2 diabetes.
(3) Amylin analogues
Amylin agonist analogues slow gastric emptying and suppress glucagon.
pramlintide is a clinically available amylin analogue.
Like insulin, it is administered by subcutaneous injection.
The most frequent and severe adverse effect of pramlintide is nausea, which occurs mostly at the beginning of treatment and gradually reduces.
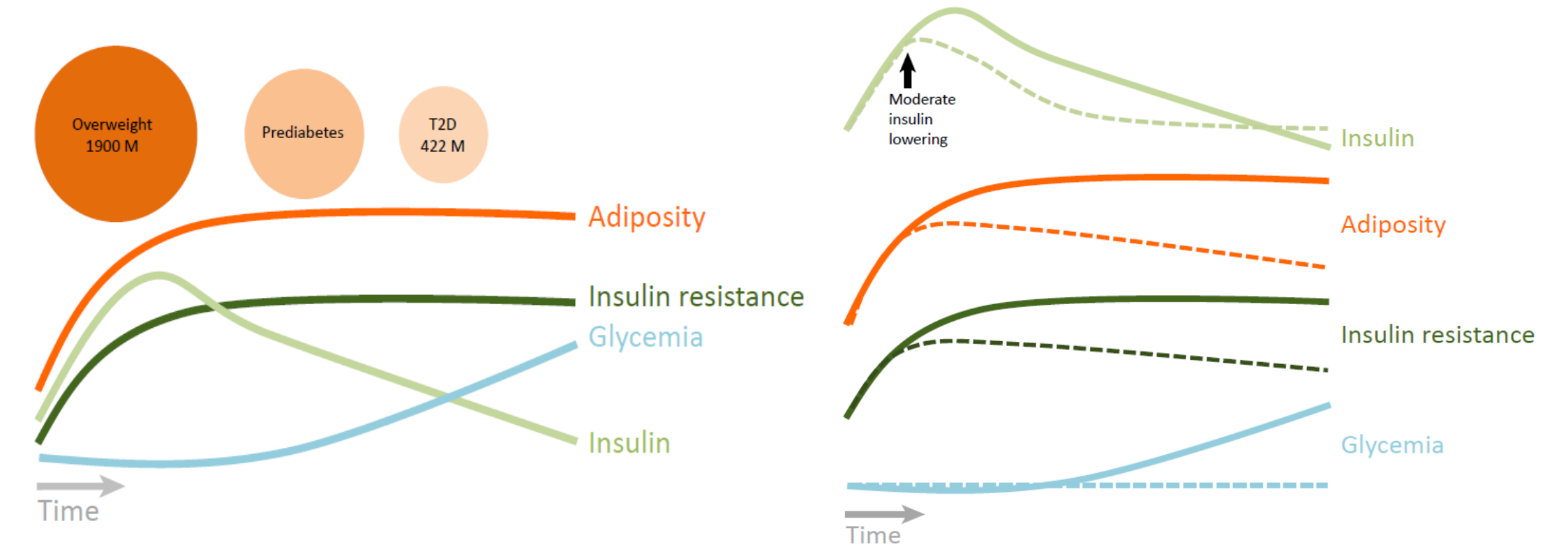
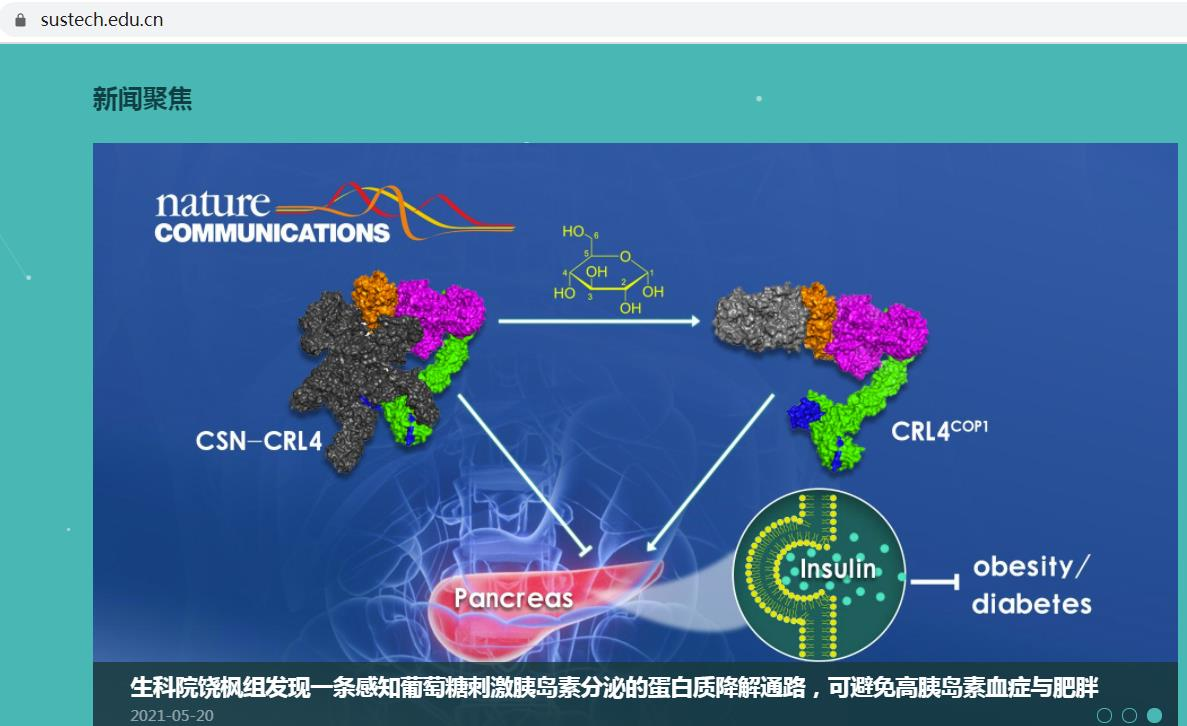
Emerging concept: mild suppression of hyperinsulinemia in treatment obesity and insulin resistance