L8 Agents used in Heart Failure and Cardiac Arrhythmias
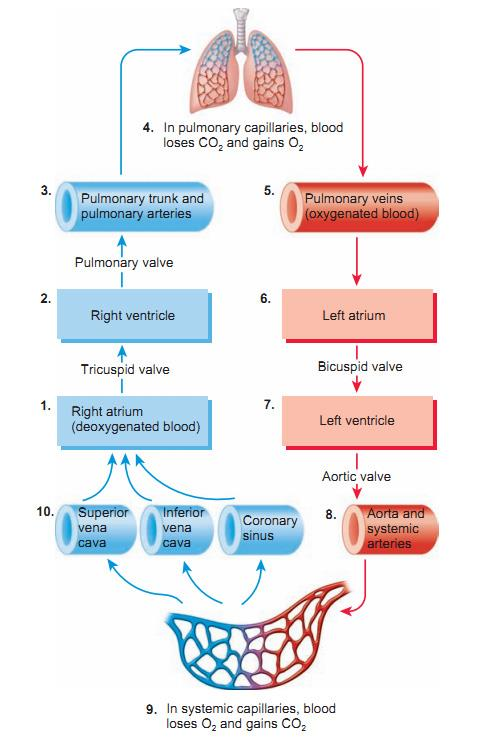
一、Heart Failure
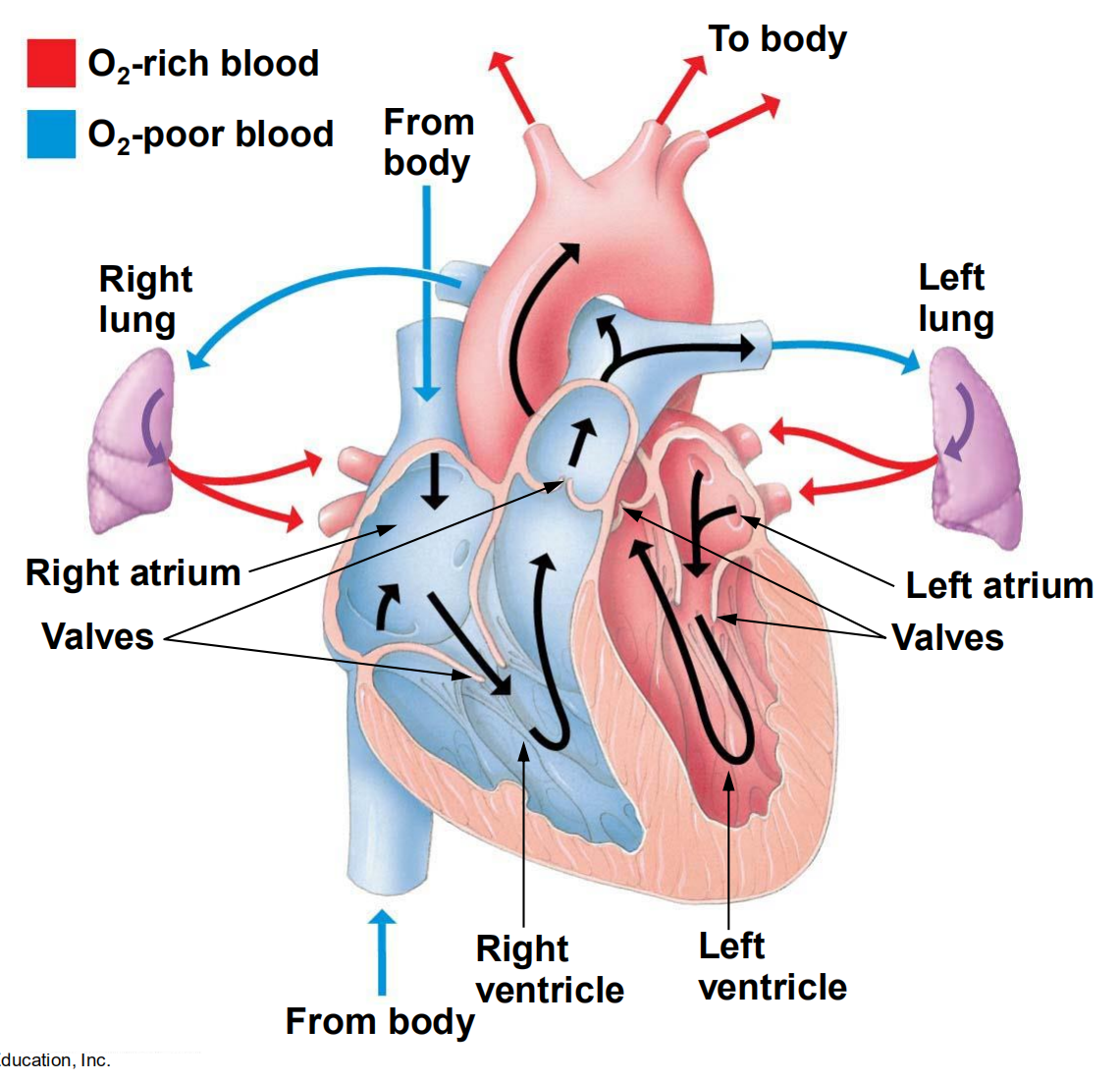
Results from any structural or functional abnormality that impairs the ability of the ventricle to eject blood (Systolic Heart Failure) or to fill with blood (Diastolic Heart Failure)
Systolic failure: reduced mechanical pumping action (contractility)and reduced ejection fraction: failure in excitation-contraction coupling
Diastolic failure: stiffening and loss of adequate relaxation results in reduced filling and cardiac output
Final common pathway for many cardiovascular diseases whose natural history results in symptomatic or asymptomatic left ventricular dysfunction (less blood coming out of heart)
Cardinal manifestations of heart failure include dyspnea (呼吸困难) , fatigue and pulmonary edema
Risk of death is 5-10% annually in patients with mild symptoms and increases to as high as 30-40% annually in patients with advanced disease
Overview of congestive heart failure
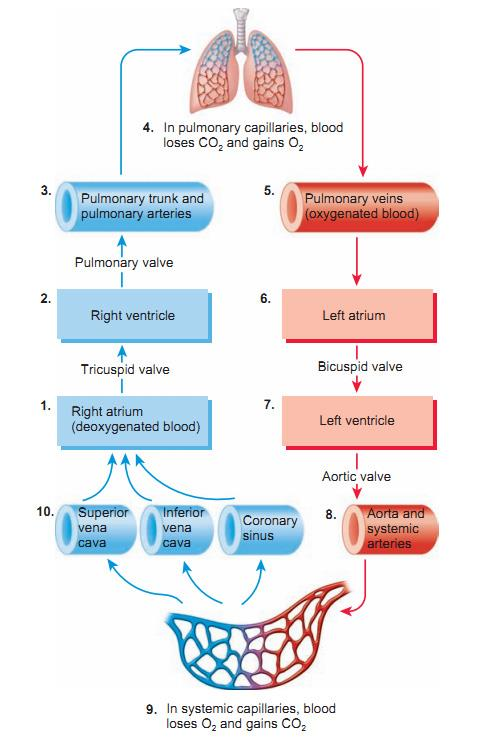
Congestive heart failure (CHF) is a condition in which the heart is unable to pump sufficient blood to meet the needs of body.
CHF can be caused by increased workload imposed on the heart.
CHF is accompanied by abnormal increases in blood volume and interstitial fluid; the heart, veins, and capillaries are therefore generally dilated with blood.
symptoms include pulmonary congestion with left heart failure, and peripheral edema with right heart failure.
Underlying causes of CHF include arteriosclerotic heart disease, hypertensive heart disease, valvular heart disease(心瓣膜病), dilated cardiomyopathy(扩张性心肌病), and congenital heart disease(先天性心脏病)
The Vicious Cycle of Heart Failure
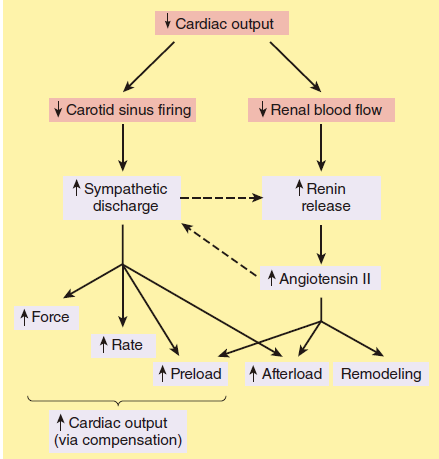
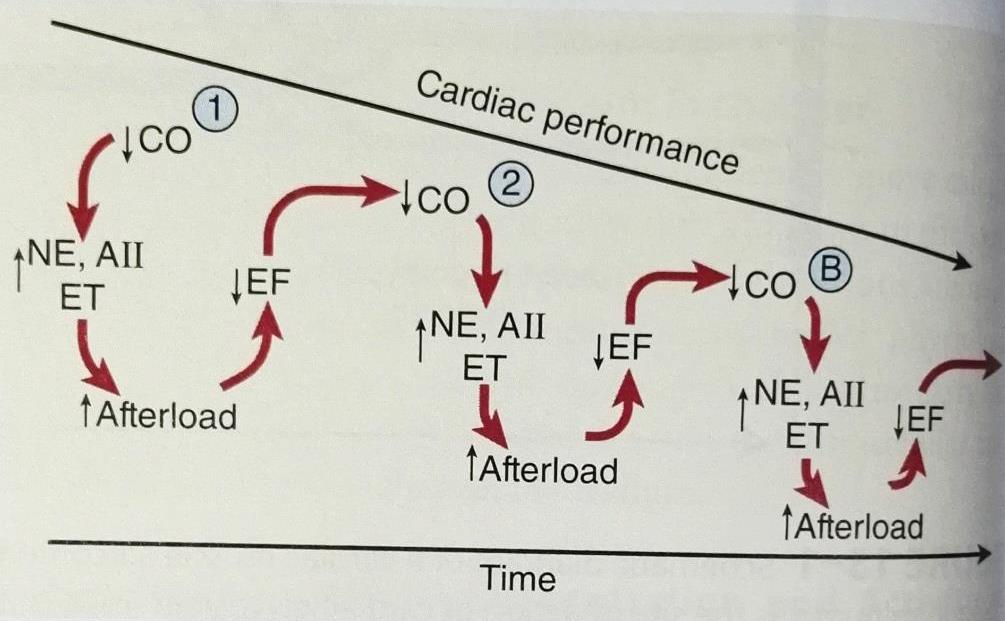
- NE: Norepinephrine;
- AII: Angiotensisn II
- ET: Endothelin;
- Therefore, targeting the SNS and RAS,together with vasodilators, will help to treat HF
Compensatory changes in heart failure
Activation of Sympathetic Nerve System
Activation of Renin-Angiotensin System
Increased heart rate
Release of Aldosterone Hormone (vaso-constriction)
Release of atrial natriuretic peptide 心钠素
Chamber enlargement 心室腔扩大
Myocardial hypertrophy 心室肥厚
二、Cardiac Contractility
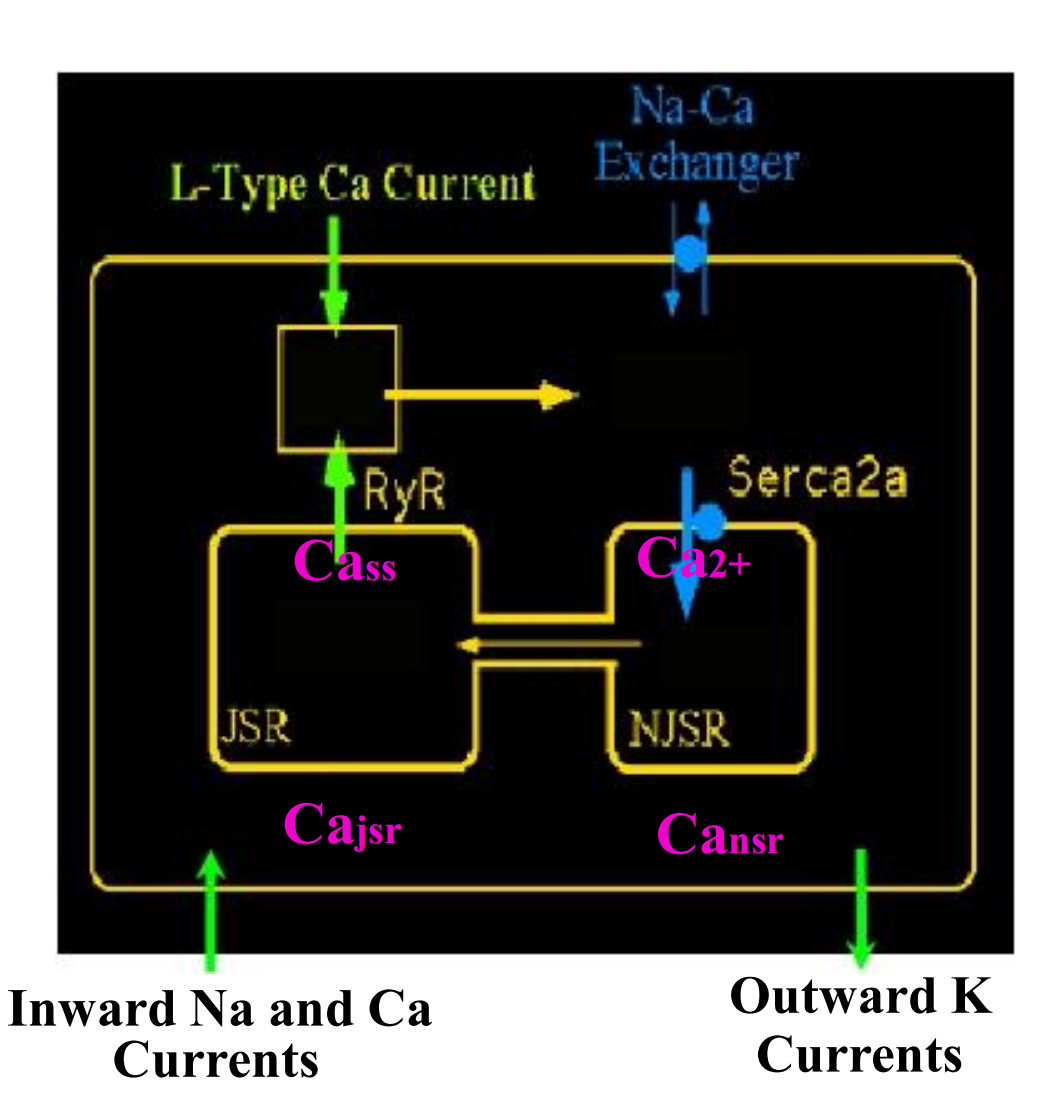
Control of normal cardiac contractility
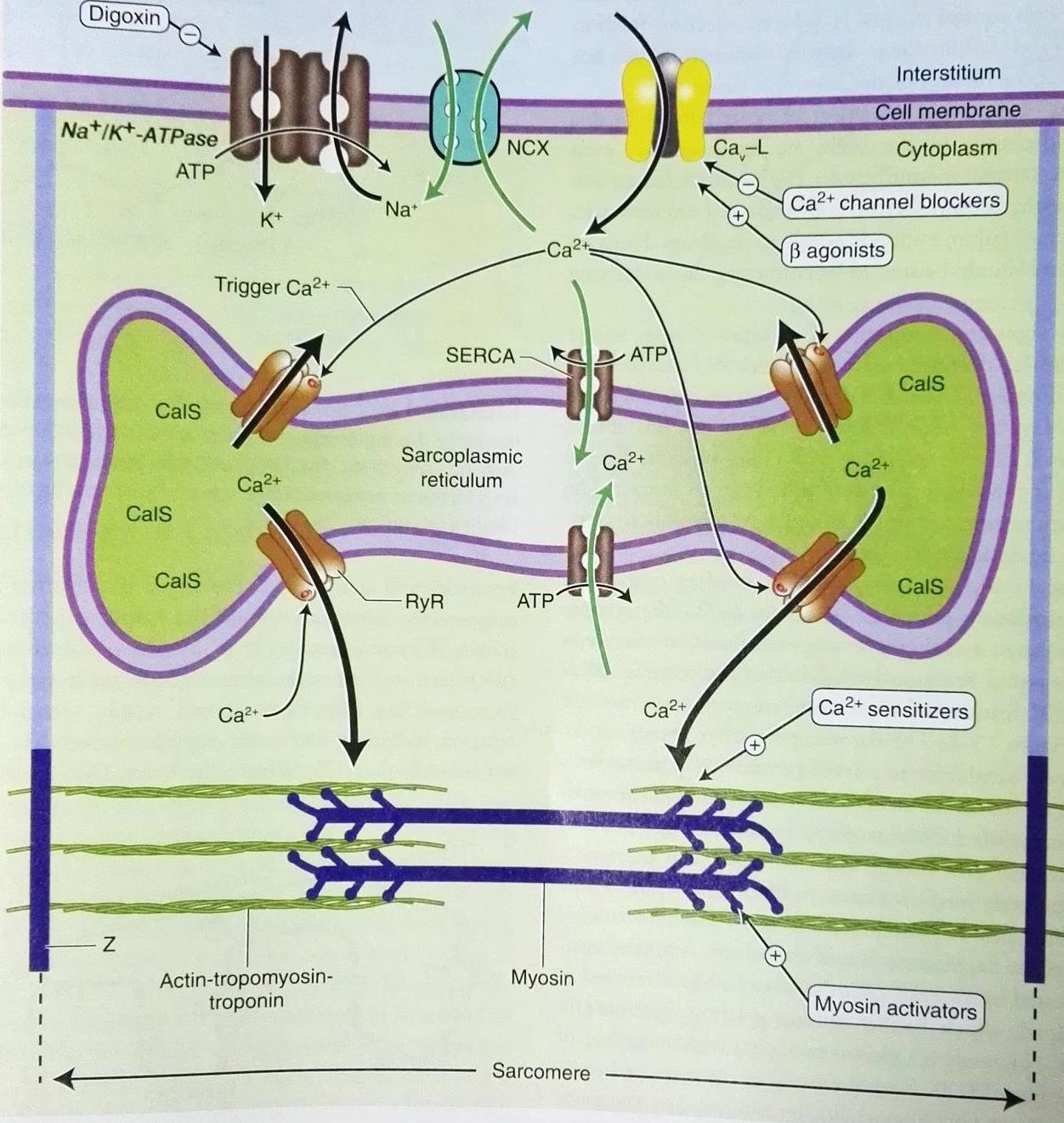
- Sensitivity of contractile proteins to calcium
- Amount of calcium released from SR
- Amount of calcium stored in SR
- Amount of trigger calcium entering cell
- Activity of sodium-calcium antiporter 6.Activity of Na+/K+-ATPase
Strategy of treatment of CHF
The therapeutic goal for CHF is to increase cardiac output
- Inotropic agents that increase the strength of contraction of cardiac muscle
- PDEI (phosphodiesterase inhibitors) agents that increase cAMP to induce systoles and vasodilatation
- Calcium sensitizers extracellular fluid volume
- β adrenergic agonist
- β adrenergic antagonist
- Vasodilators: Calcium channel blocker
- Decreasing RAS activity: ACEI and AT1 antagonist
- Diuretic agents
Treatment of congestive heart failure
1. Positive inotropic drugs
- Cardiac glycosides
- β-adrenergic agonists (New dopamine receptor agonist)
- phosphodiesterase inhibitors
- Calcium sensitizers
Cardiac glycosides/强心苷类
An inotrope is an agent that alters the force or energy of muscular contractions. Negatively inotropic agents weaken the force of muscular contractions. Positively inotropic agents increase the strength of muscular contraction
- prevent calcium efflux
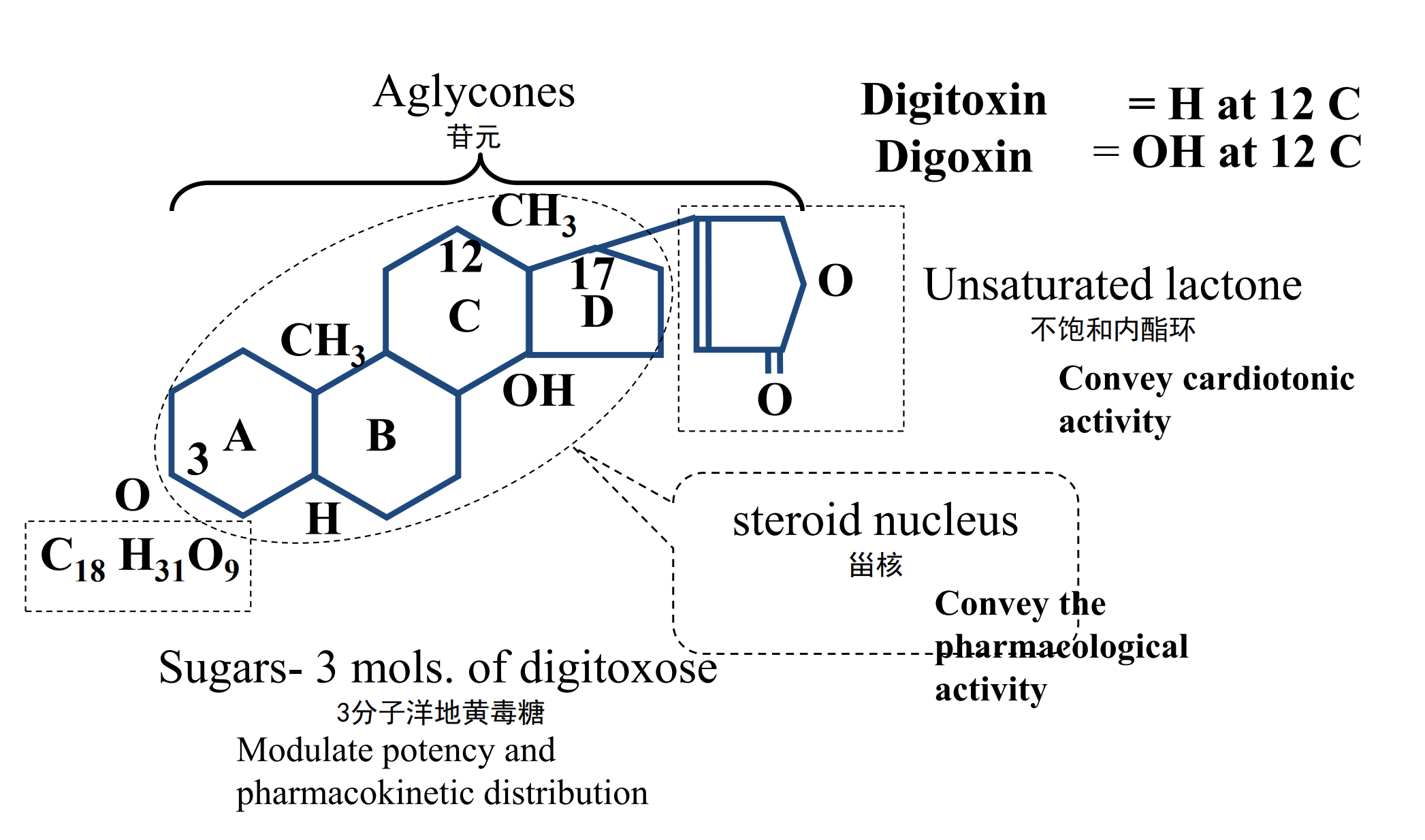
- The Unsaturated lactone(不饱和内酯环)Convey cardiotonic activity
- The steroid nucleus(甾核)Convey the pharmacological activity
- The Sugars- 3 mols. of digitoxose (3分子洋地黄毒糖) Modulate potency and pharmacokinetic distribution
(1) Machanism of cardiac glycoside on positive inotropic action
- Inhibiting Na+-K+-ATPase in therapeutic dose:
- Increasing of calcium inward and induce the releasing of calcium from sarcoplasmic reticulum
(2) Pharmacologic action
Action of cardiac glycosides on the heart
- Positive inotropic action:Increasing contractility of cardiac muscle in heart failure.
- characteristic:
- myocardiac quick contraction↓
- rate of force ↑
- time to peak tension ↓
- myocardiac quick contraction↓
- Effect of positive inotropic act
- cardiac output is increased
- compensatory sympathetic tone is reduced
- cardiac preload and afterload is decreased
- heart rate is reduced
- myocardiac fiber tone and oxygen consumption is decreased
- characteristic:
- Negative chronotropic (heart-rate change) action
- Continuous effect of positive inotropic action → increased cardiac output, heart rate is decreased (due to dereased sympathetic tone)
- Chronotropic drugs may change the heart rate and rhythm by affecting the electrical conduction system of the heart and the nerves that influence it, such as by changing the rhythm produced by the sinoatrial node. Positive chronotropes increase heart rate; negative chronotropes decrease heart rate.
- The CO is determined by heart rate and muscle contraction strength
(3) Clinical uses
Cardiac glycosides are given for CHF
- ,
- Best :go with atrial fibrillation
- Better:hypertension congenital heart disease
Some kinds of arrhythmias (abnormal heart rate)
- Atrial fibrillation
- Atrial flutter
- Supraventricular Tachycardia
β-Adrenoceptor agonists
They are used intravenously in CHF emergencies
Example of β-Adrenoceptor agonists :
Dobutamine (多巴酚丁胺)
- Exciting β1 Adrenoceptor → positive inotropic action →the volume of output↑
- Exciting β2 Adrenoceptor→dilate the vascular → afterload↓
have benefits within short time
Phosphodiesterase-Ⅲ inhibitors
Inodilator / inodilating drugs
- Inhibiting the activity of PDE Ⅲ → cAMP↑→ causes an increase in myocardial contractility and vasodilatation →total peripheral resistance ↓ →cardiac output ↑
Examples:
- Armirinone(氨力农): Inhibits the excess product of NO, TNF and affects the neurohormone, anti-the forming of thrombus
- milrinone(米力农): stronger 20 time
- vesnarinone(维司力农): myocardial contract element’s
the sensitivity to calcium ↑
Calcium sensitizers
Pimobendan 匹莫苯:
- Inhibit PDE Ⅲ ; increase TnC’s sensitivity to calcium
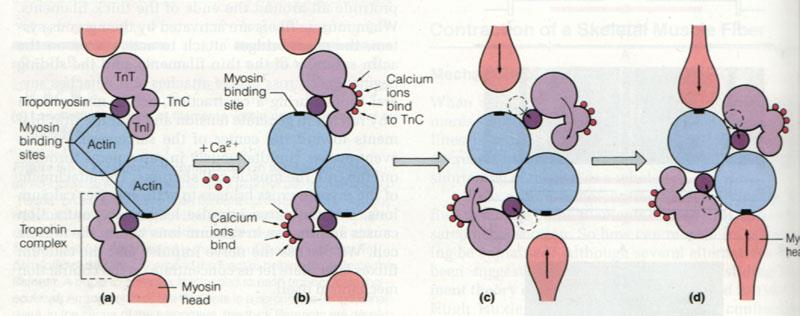
Tn troponin—肌钙蛋白;myosin-肌球蛋白;tropomyosin-原 ;Actin 肌动蛋白
2. Diuretics
Diuretics inhibit sodium and water retention, →reduce the volume of blood, →venous pressure and the thus cardiac preload are reduced↓, increasing the efficiency of the heart as a pump→ cardiac output ↑, so reduce oedema due to heart failure
Heart failure
- Low-grade : Thiazides hydrochlorothiazide 氢氯噻嗪
- Higher-grade : Acute left heart failure
- loop diuretics — furosemide 呋塞米(速尿)
- Spironolacton 螺内酯
- (anti-aldosterone ,keep potassium and diuretics)
3. Vasodilators
- Calcium channel blocker
- Nitryl-vasodilators
- Hydralazine
Angiotensin-converting-enzyme inhibitor (ACEI )
Example: Captopril Enalapril
Methanism of anti-CHF:
- Humour: Inhibit ACE→angiotensin Ⅱ and aldosterone levels↓, reduce sodium retention, increase bradykinin levels , ANP、 NO、PGI2↑, reduce the release of NA ET and renew the expression of βreceptor
- This therefore causes vasodilatation (include coronary artery) →reduction in peripheral resistance→ increase the cardiac output, Increase the blood flow of kidney so Improve the function of kidney
- Prevent the remodel of the heart
vesodilation → reduce preload
AT1 antiagonists
Losartan (氯沙坦)
- The function just like ACEⅠ
Clinical utilize:
- CHF (Congestive heart failure)
- Protection of kidneys
Calcium-channel blockers
Amlodipine 氨氯地平
- Blood Vessel Targeting
- Dilate artery
- Dilate the coronary
- Alleviate the LV Wall Tension
Others –Vasodilators: for phrephoiral
for heart failure patients, the pre and afterload should be both low by using drugs low afterload: prevent CO to decrease
mechanism: Finally Decrease the oxygen demand of the heart
- Dilatation of the veins→ decreases preload
- Dilatation of the artery→ decreases afterloads
Examples:
- Nitrate esters: nitroglycerin , nitroprusside sodium 硝普纳
- Hydralazine 肼屈嗪 direct dilate the vascular
- Prazosin 哌唑嗪 ɑ-receptor blocker
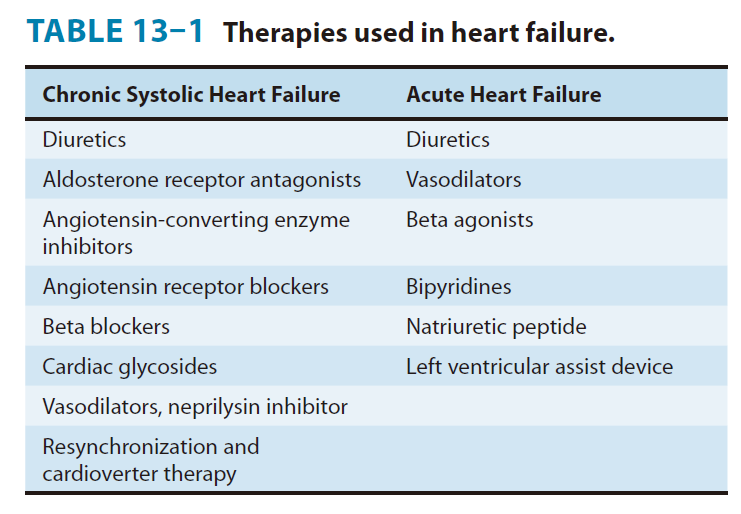
4. RAAS inhibitors
antiotensin converting enzyme inhibitor and AT1 antagonist
Combine drugs to treat heart failure to increase CO and induce vessel dilation at the same time, to prevent entering into the vicious cycle
The same as combining drugs to treat HTN: inducing vessel dilation while decreasing CO
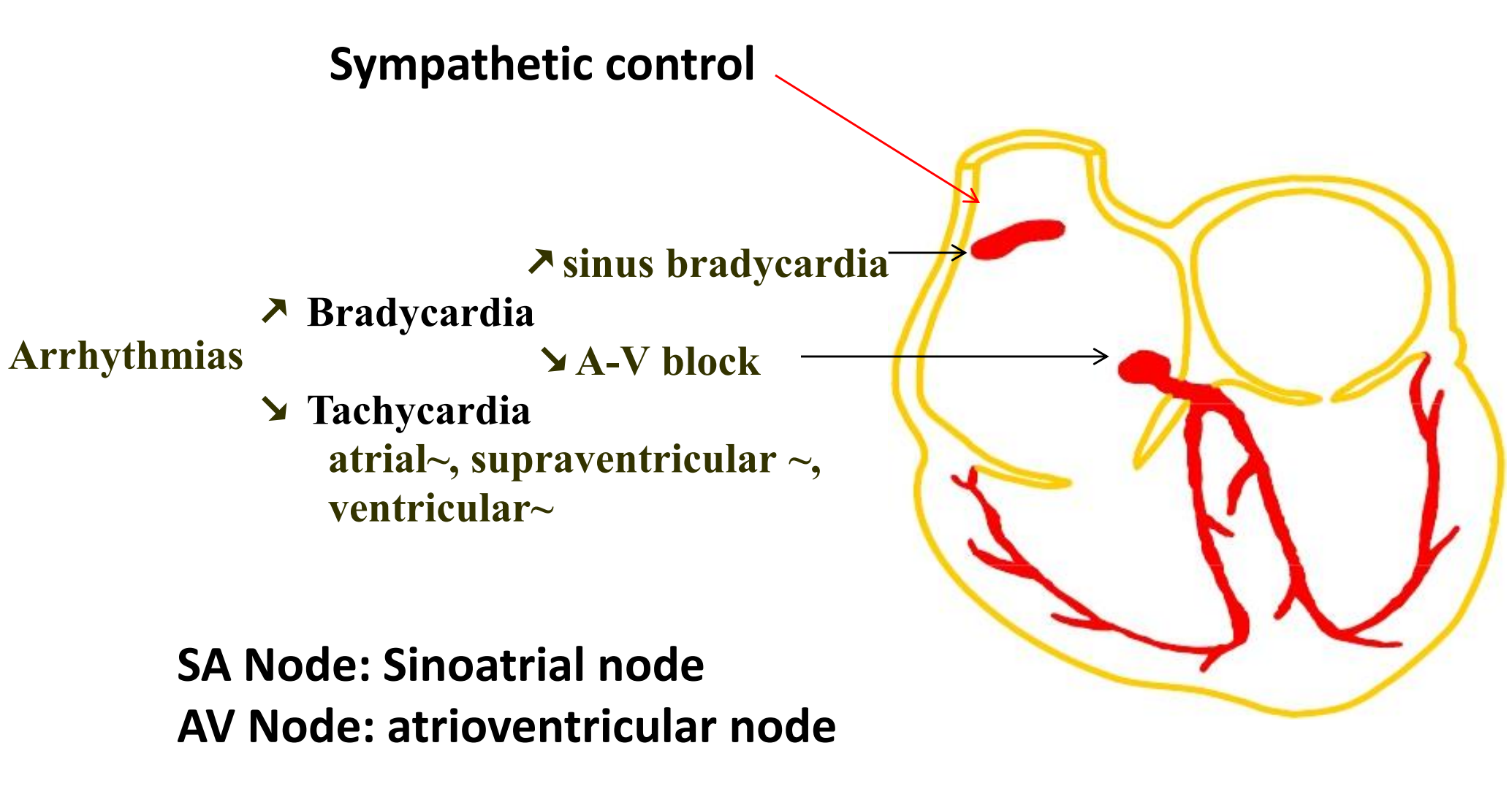
三、Agents used in Cardiac Arrhythmias
Definition of arrhythmia: irregular heart beat
Arrhythmias and disrhythmias are the same thing. Cardiac arrhythmia is an abnormality of the heart rhythm
- Bradycardia – heart rate slow (<60 beats/min) 心动过缓
- Tachycardia – heart rate fast (>100 beats/min) 心动过速
Arrhythmias is common
- 50% of anesthetized patients
- 80% of myocardial infarction patients
Can cause diziness, loss of consciousness, or death
Categories of arrhythmias
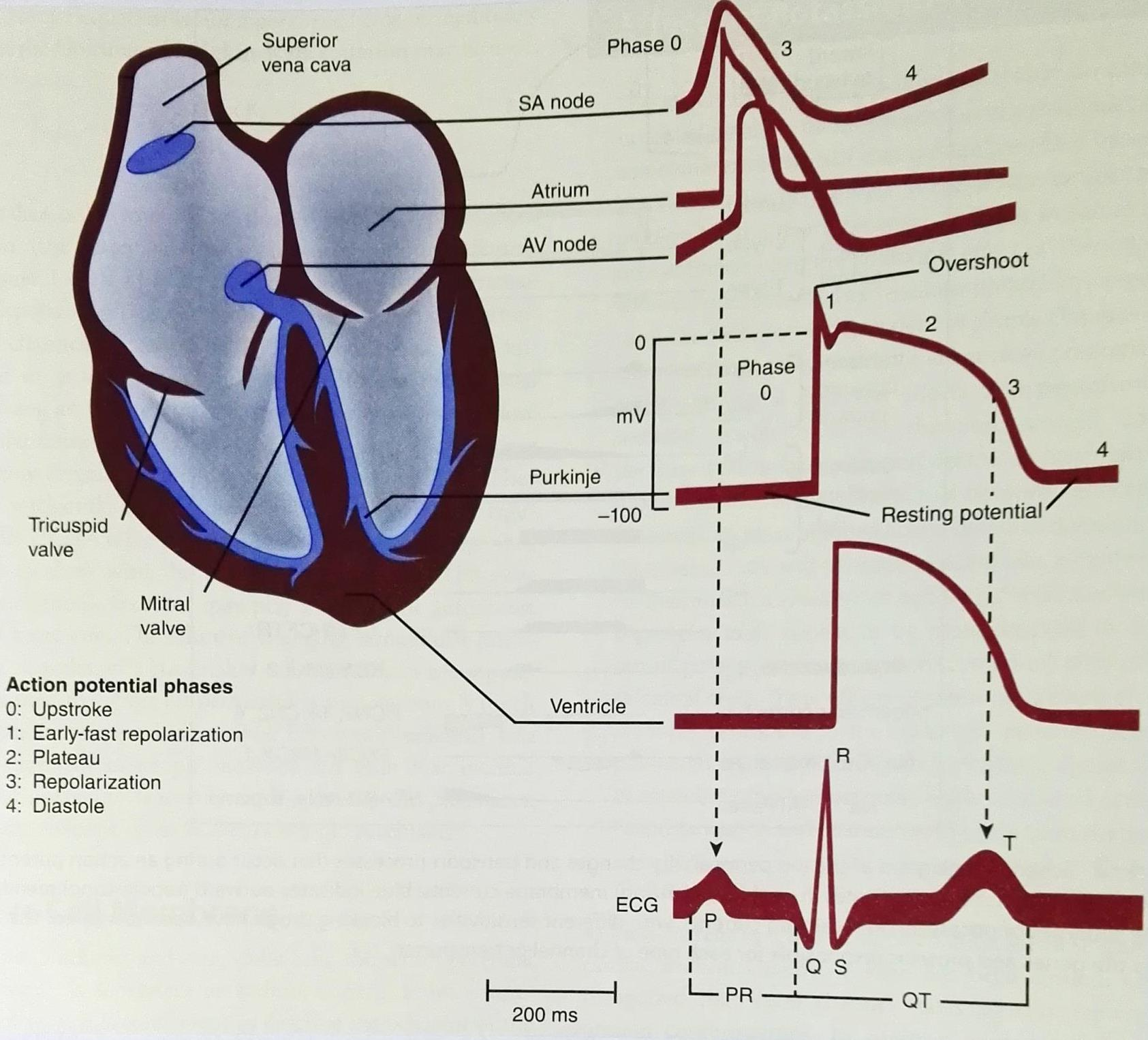
ECG
ECG is the body surface manifestion of the depolarization and repolarization waves of the heart
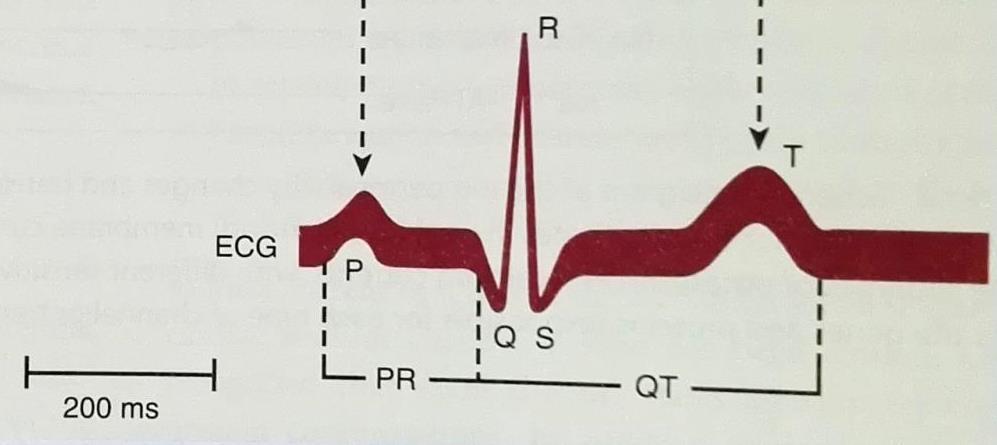
P: Atrial depolarization (Site of origin of the electrical impulse)
QRS: ventricle depolarization
T: ventricle repolarization
PR interval: a measure of conduction time from atrium to ventricle
QRS: the time required for all of the ventricular cells to be activated (the intraventricular conduction time)
QT: the duration of the ventricular action potential
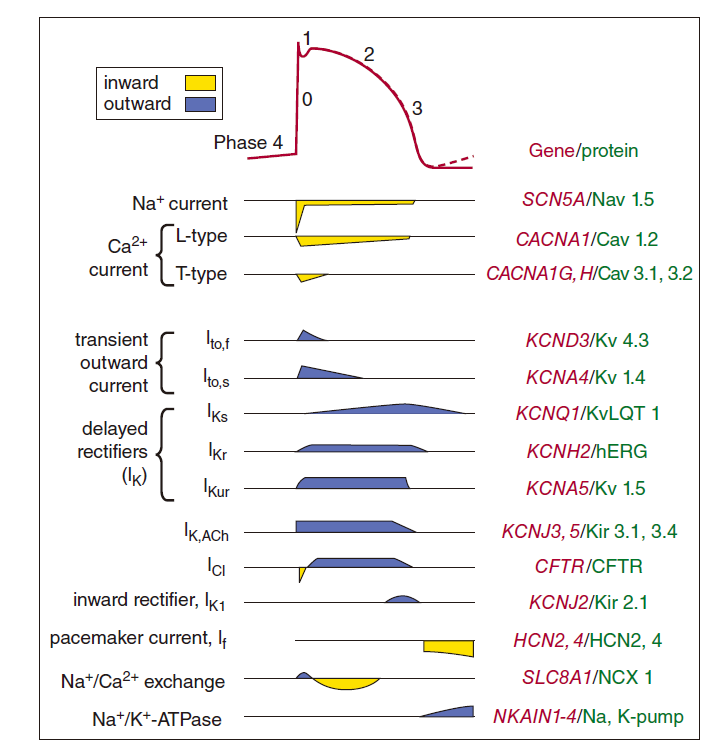
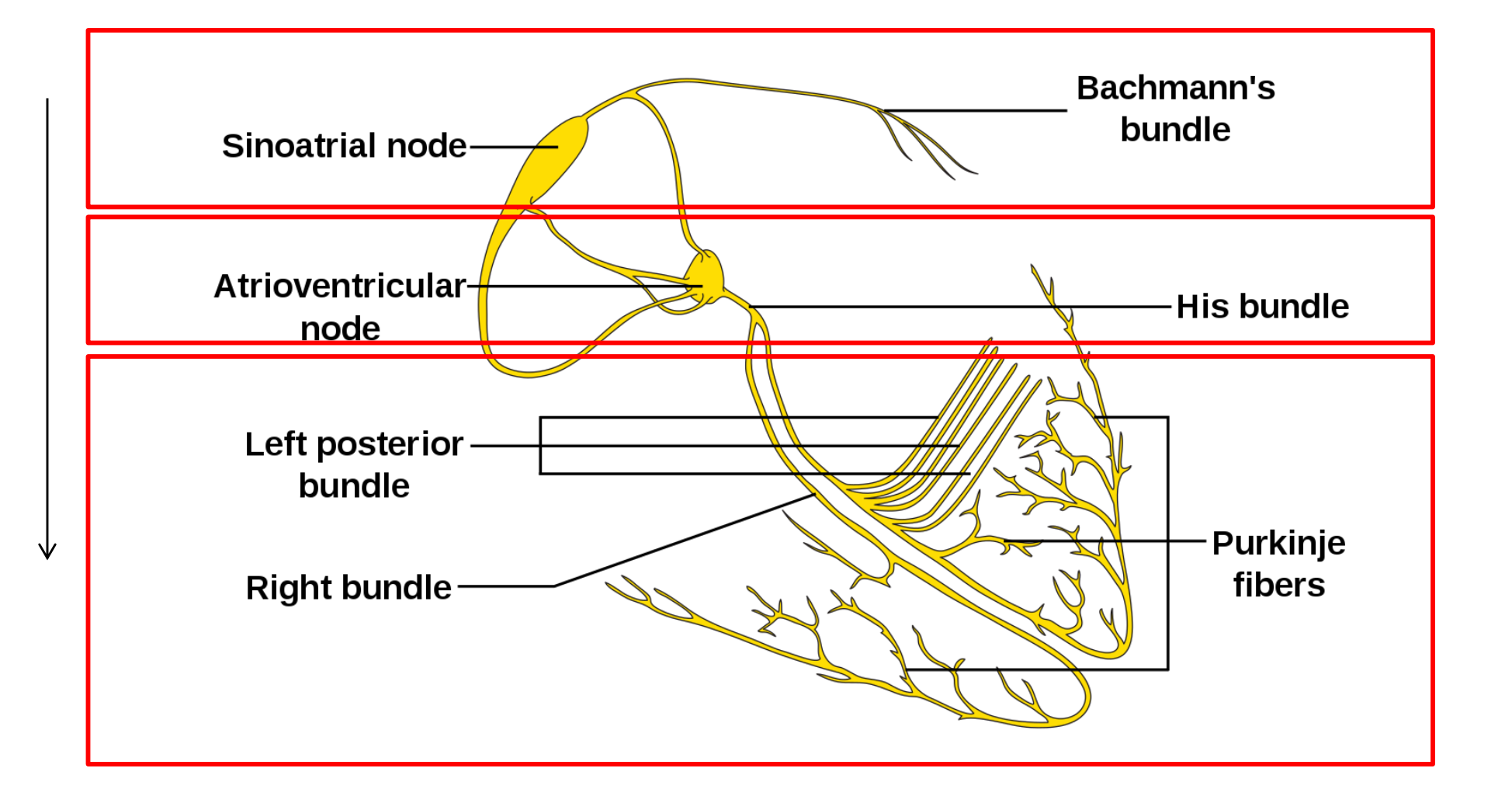
1. Cardiac Electrophysiology
To understand the action and classification of the antiarrhythmic drugs, it is first necessary to understand the ionic movements that underlie the cardiac membrane potential
The voltage change of the membrane potential is associated with the changes of ions across membrane, ie Na+, K+, and Ca2+
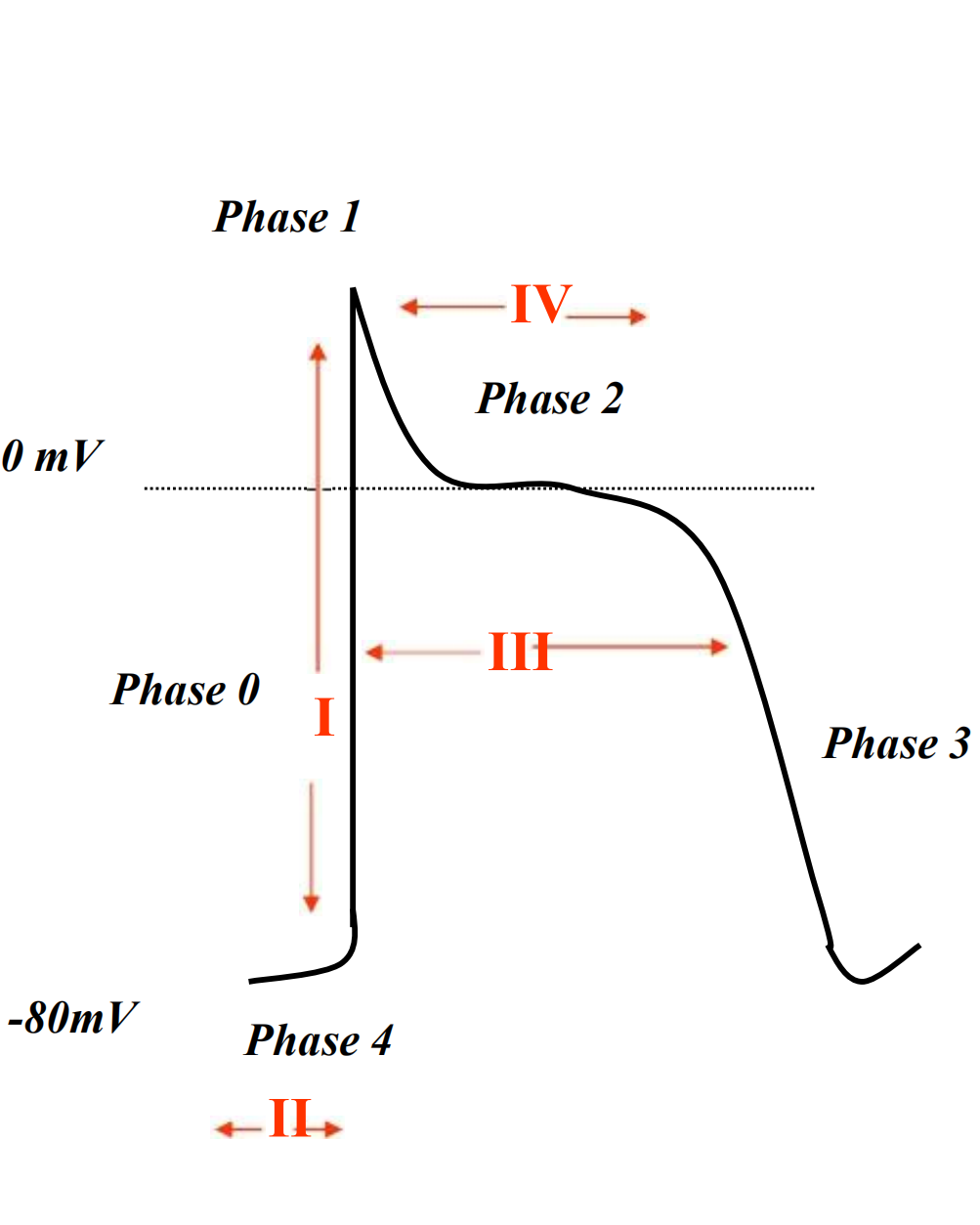
2. Phases of action potential of cardiac cells
A typical AP of ventricular muscle cell can be divided into 5 phases
Phase 0: rapid depolarisation – inflow of Na+
Phase 1:partial repolarization – inward Na+ of K+
Phase 2: plateau – slow inward calcium current
Phase 3:rapid repolarisation – calcium current inactivates, K+ outflow
Phase 4:pacemaker potential/diastole
- Na+ outflow and K+ inflow by Na-KATPase
- Autorhythmic cell : Na+ inflow to reach threshold potential