L10 Sedatives, Antipsychotic and antidepressants
一、Review of Pharmacology of CNS Drugs
Central neurotransmitters
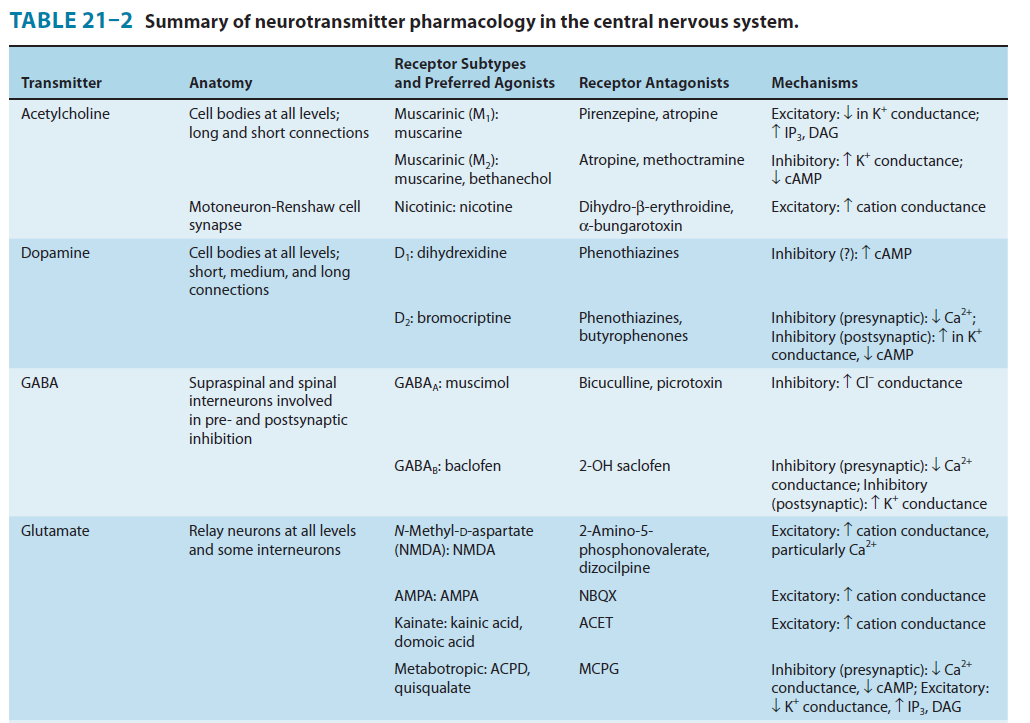
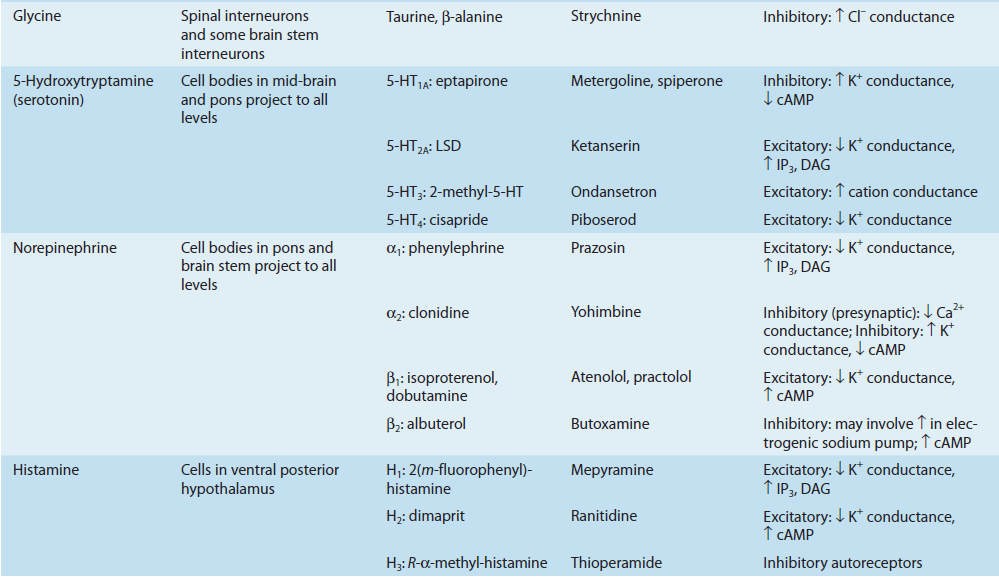
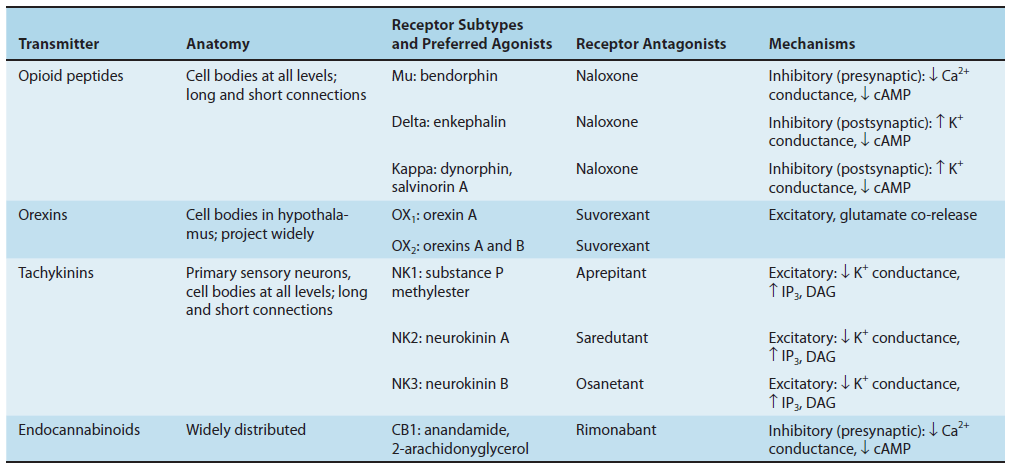
Amino acids: Glutamate Excitatory Neurotransmitter
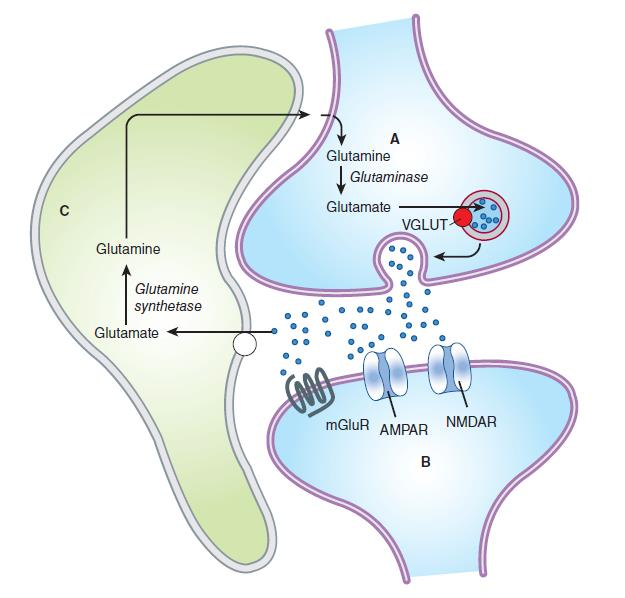
Glutamine is imported into the glutamatergic neuron (A) and converted into glutamate by glutaminase. The glutamate is then concentrated in vesicles by the vesicular glutamate transporter. Upon release into the synapse, glutamate can interact with AMPA and NMDA ionotropic receptor channels (AMPAR, NMDAR) in the postsynaptic density (PSD) and with metabotropic receptors (MGluR) on the postsynaptic cell (B). Synaptic transmission is terminated by active transport of the glutamate into a neighboring glial cell (C) by a glutamate transporter. It is synthesized into glutamine by glutamine synthetase and exported into the glutamatergic axon. (D) shows a model NMDA receptor channel complex consisting of a tetrameric protein that becomes permeable to Na+ and Ca2+ when it binds a glutamate molecule.
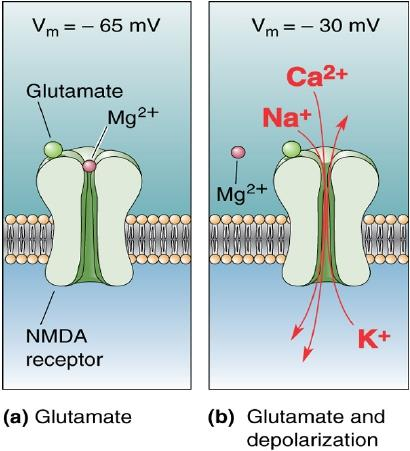
NMDA receptors are highly permeable to Ca2+ as well as to Na+ and K+. Due to the voltage-dependent block of the NMDA pore by extracellular Mg2+, there are two requirements for NMDA receptor channel opening: Glutamate must bind the receptor and the membrane must be depolarized to expel Mg2+. The rise in intracellular Ca2+ that accompanies channel opening can result in a longlasting enhancement in synaptic strength that is referred to as long-term potentiation (LTP). Which is generally accepted as an important cellular mechanism underlying learning and memory.
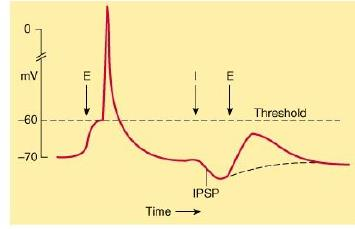
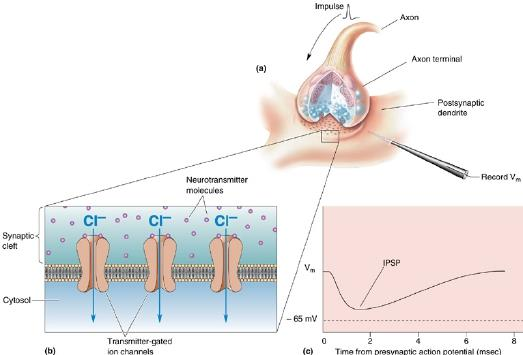
Amino acids: GABA and Glycine-Inhibitory Neurotransmitter
Neurotransmitter crosstalk
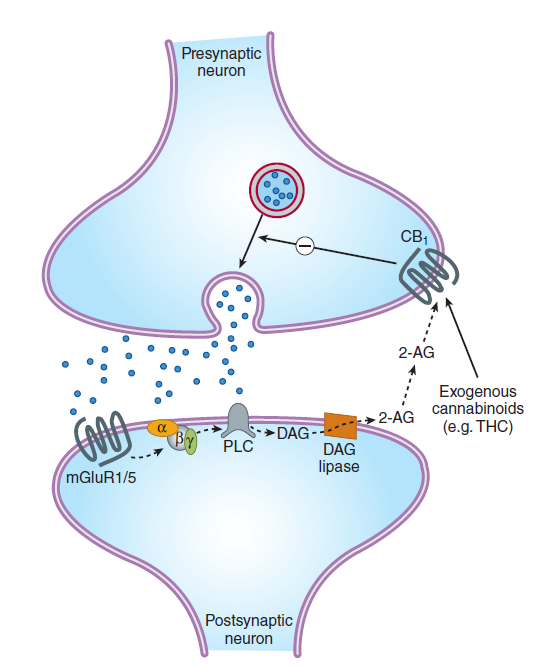
- norepinephrine: negative feedback (prevent over-release)
二、Sedative-Hypnotic Drugs
Introduction
Sedative(镇静剂) = quiets patient, gives a feeling of relaxation and rest
- Not necessarily accompanied by sleep
Hypnotic(安眠药) = produces sleep
镇静 -> 催眠 -> 麻醉
An effective sedative agent should reduce anxiety and exert a calming effect with little or no effect on motor or mental functions
A hypnotic drug should produce drowsiness and encourage the onset and maintenance of a state of sleep that as far as possible resembles the natural sleep state
Chemical Classification
Benzodiazepines: wildly used, not to lead general anesthesia, or death.
Barbiturates: the older sedative-hypnotics, general depression of central nervous system. With such drugs, an increase in dose above that needed for hypnosis may lead to a state of general anesthesia. At still higher doses, it may depress respiratory and vasomotor centers, leading to coma and death
Newer Hypnotics: Several drugs with novel chemical structures have been introduced more recently for use in sleep disorders.
1. Benzodiazepines
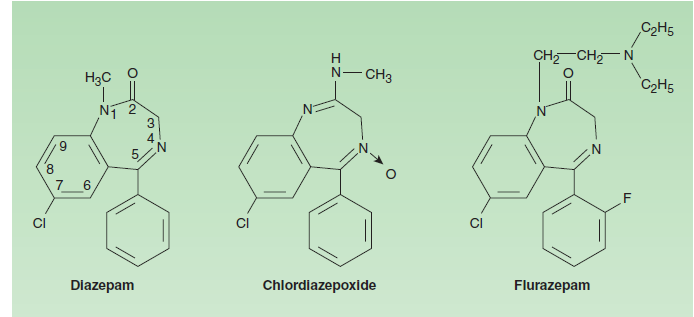
The benzodiazepines are widely used sedative-hypnotics. All of the structures are 1,4-benzodiazepines, and most contain a carboxamide group in the 7-membered heterocyclic ring structure. A substituent in the 7 position, such as a halogen or a nitro group, is required for sedative-hypnotic activity. The structures of triazolam and alprazolam include the addition of a triazole ring at the 1,2position.
2. Barbiturates
The chemical structures of some older and less commonly used sedative-hypnotics, including several barbiturates
3. Newer Hypnotics
Ramelteon
- Ramelteon, a novel hypnotic drug prescribed specifically for patients who have difficulty in falling asleep, is an agonist at MT1 and MT2 melatonin receptors located in the suprachiasmatic nuclei of the brain.
Buspirone
- Buspirone has selective anxiolytic effects, and relieves anxiety without causing marked sedative, hypnotic, or euphoric effects. Unlike benzodiazepines, the drug has no anticonvulsant or muscle relaxant properties. Buspirone does not interact directly with GABAergic systems. It may exert its anxiolytic effects by acting as a partial agonist at brain 5HT1A receptors, but it also has affinity for brain dopamine D2 receptors.
Pharmacodynamics
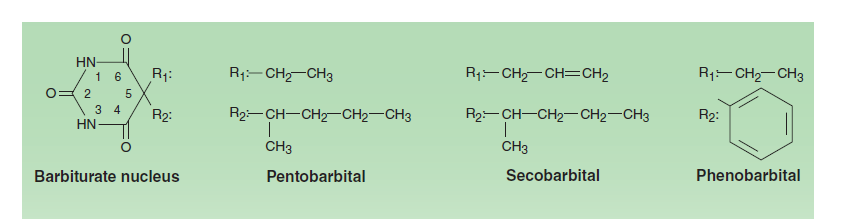
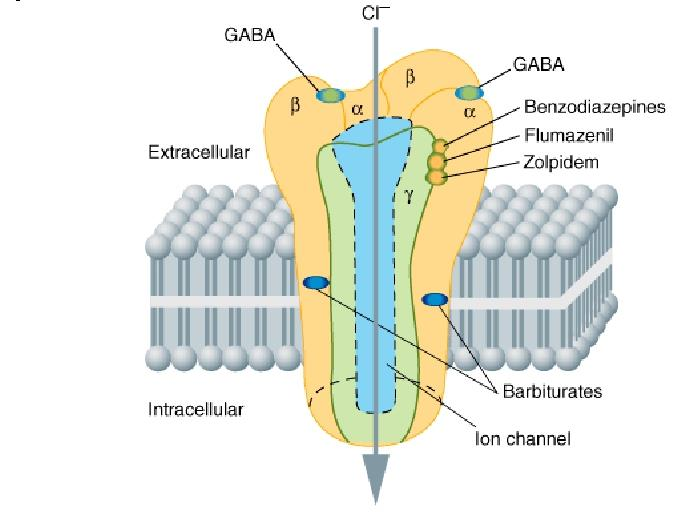
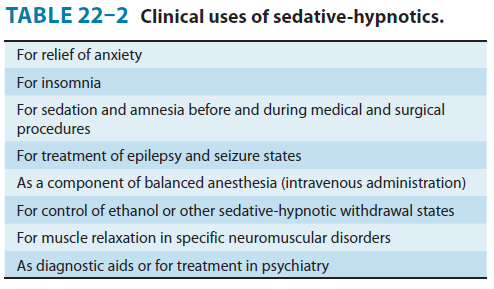
1. GABA receptor
2. Neuropharmacology
Benzodiazepines appear to increase the efficiency of GABAergic synaptic inhibition.
- Do not substitute for GABA
- Enhance GABA’s effects allosterically without directly
- Activating GABA
Areceptors or opening the associated chloride channels. - Increase the frequency of channel-opening events.
Barbiturates increase the duration of the GABA-gated chloride channel openings.
- Barbiturates also exert nonsynaptic
- Membrane effects in parallel with their effects on GABA and glutamate neurotransmission.
- Induce full surgical anesthesia and for their more pronounced central
- Depressant effects compared with benzodiazepines and the newer hypnotics.
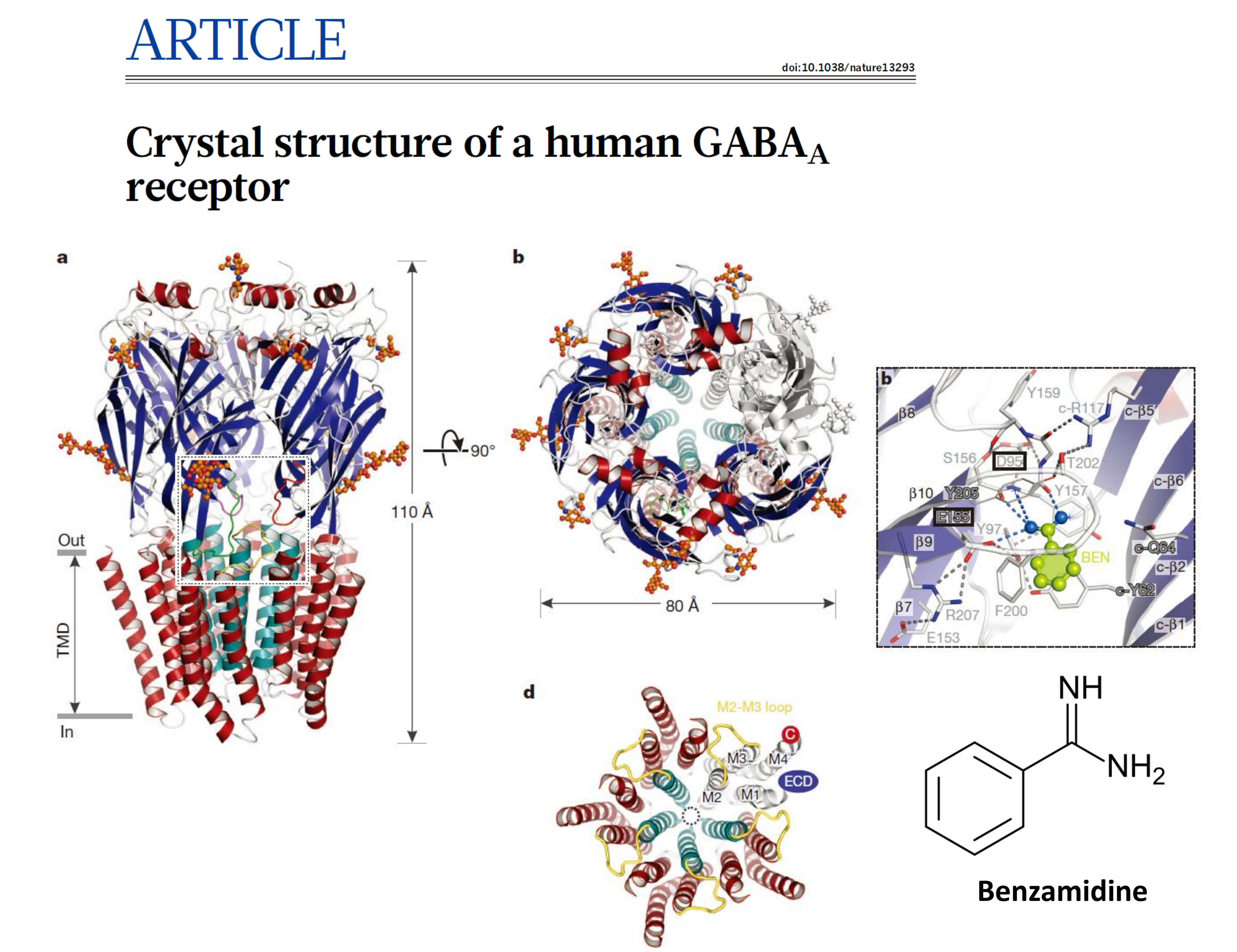
Basic Pharmacology of Sedative-Hypnotics
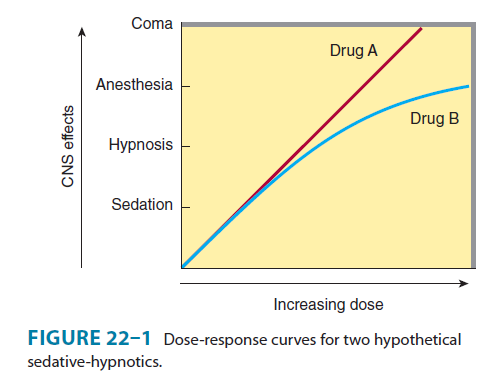
The linear slope for drug A is typical of many of the older sedative-hypnotics, including the barbiturates and alcohols. With such drugs, an increase in dose higher than that needed for hypnosis may lead to a state of general anesthesia. At still higher doses, these sedative-hypnotics may depress respiratory and vasomotor centers in the medulla, leading to coma and death. Deviations from a linear dose-response relationship, as shown for drug B, require proportionately greater dosage increments to achieve central nervous system depression more profound than hypnosis. This appears to be the case for benzodiazepines and for certain newer hypnotics that have a similar mechanism of action.
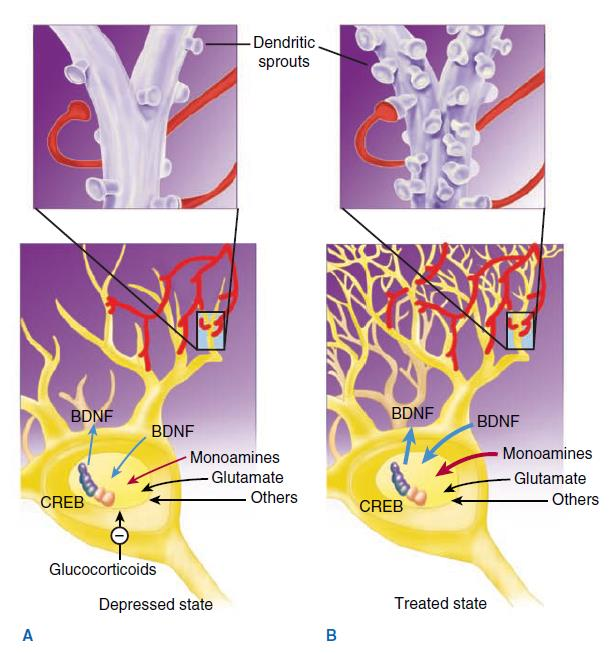
Clinical Pharmacology of Sedative-Hypnotics
1. Treatment of Anxiety States
Advantages of benzodiazepines for anxiety
- a rapid onset of action
- a relatively high therapeutic index, plus availability of flumazenil for treatment of overdose
- a low risk of drug interactions based on liver enzyme induction
- minimal effects on cardiovascular or autonomic functions.
Disadvantages of benzodiazepines
- Dependence
- Depression of central nervous system functions
- Amnestic effects
- To cause depression when administered with other drugs, including ethanol
2. Benzodiazepine Antagonists: Flumazenil
Flumazenil is one of several 1,4-benzodiazepine derivatives with a high affinity for the benzodiazepine binding site on the GABA-A receptor that act as competitive antagonists.
It blocks many of the actions of benzodiazepines, zolpidem, zaleplon, and eszopiclone, but does not antagonize the central nervous system effects of other sedative-hypnotics, ethanol, opioids, or general anesthetics.
- Flumazenil is approved for use in reversing the central nervous system depressant effects of benzodiazepine overdose and to hasten recovery following use of these drugs in anesthetic and diagnostic procedures.
三、Antidepressant agents
Introduction
Major depressive disorder (MDD) is characterized by depressed mood most of the time for at least 2 weeks and/or loss of interest or pleasure in most activities. In addition, depression is characterized by disturbances in sleep and appetite as well as deficits in cognition and energy. Thoughts of guilt, worthlessness, and suicide are common.
Major depression is commonly associated with a variety of medical conditions—from chronic pain to coronary artery disease. Coronary artery disease, diabetes, and stroke appear to be more common in depressed patients, and depression may considerably worsen the prognosis for patients with a variety of comorbid medical conditions
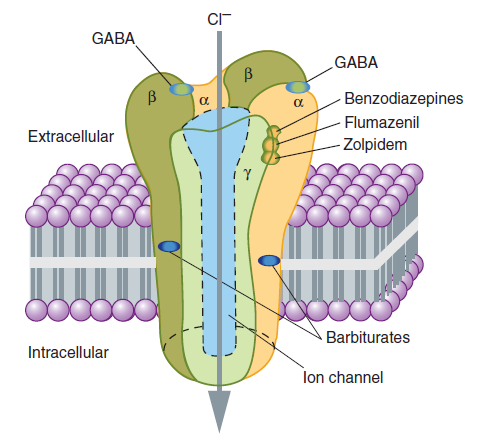
Neurotrophic Hypothesis
Decrease of brain‐derived neurotrophic factor (BDNF) in association with stress and pain
Loss of volume in structures such as the hippocampus in patients
BDNF into the midbrain, hippocampus, and lateral ventricles of rodents has an antidepressant‐like effect in animal models
All known classes of antidepressants are associated with an increase in BDNF levels in animal models with chronic administration
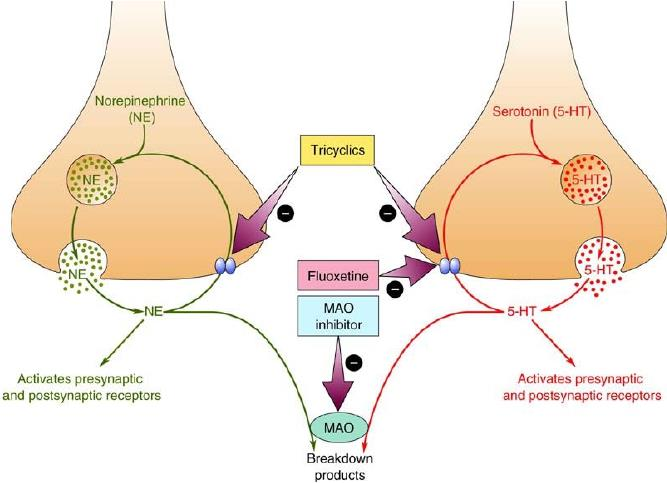
Monoamines and other neurotransmitters
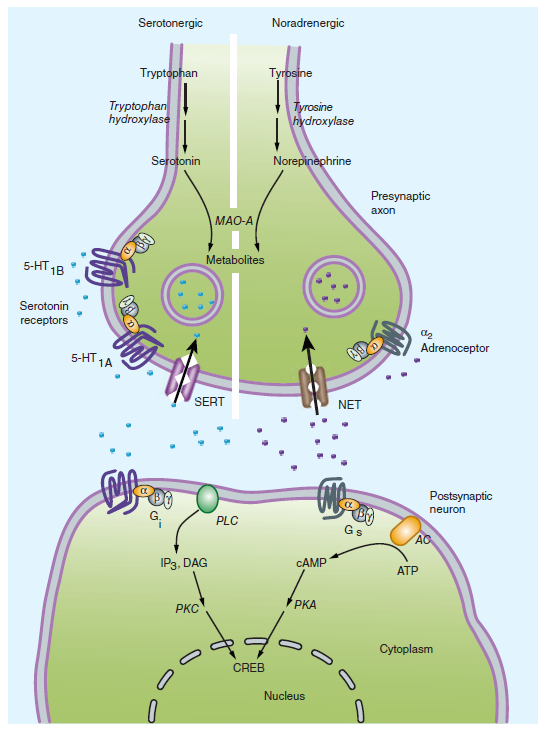
A deficiency in the amount or function of cortical and limbic serotonin (5‐HT), norepinephrine (NE), and dopamine (DA).
All classes of antidepressants appear to enhance the synaptic availability of 5‐HT, norepinephrine, or dopamine.
Neuroendocrine
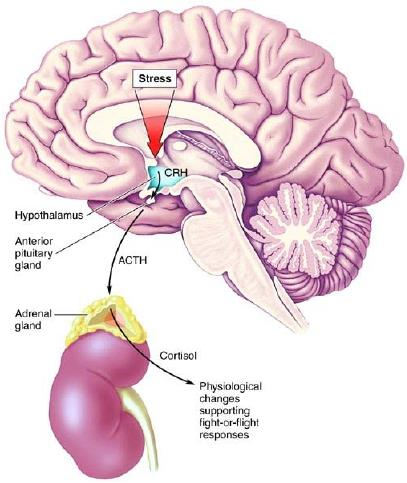
Abnormalities in the HPA axis in patients with MDD
MDD is associated with elevated cortisol levels
Both exogenous glucocorticoids and endogenous elevation of cortisol are associated with mood symptoms and cognitive deficits similar to those seen in MDD.
Types of Mood Disorders
- Depression
- Dysthymia—chronically depressed mood/2 other s/s and for at least 2 years
- Bipolar—depression alternating with mania
- Cyclothymia—mild type of bipolarity. S/S
- Must be present for 2 years.
Basic Pharmacology of Antidepressants
1. Selective Serotonin Reuptake Inhibitors (SSRIs)
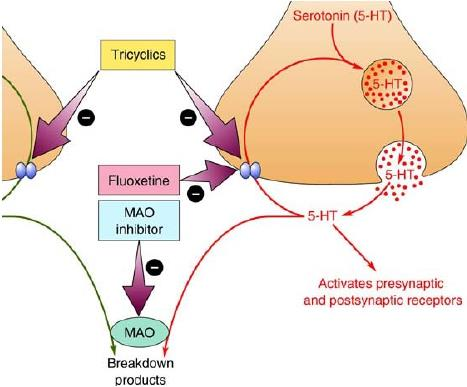
SSRIs are the most common antidepressants in clinical use
Major depression
- Panic disorder, generalized anxiety disorder (GAD), post‐traumatic stress disorder (PTSD), obsessive‐ compulsive disorder (OCD) and Pain disorders
2. Serotonin‐norepinephrine Reuptake Inhibitors
SNRIs: venlafaxine, and duloxetine
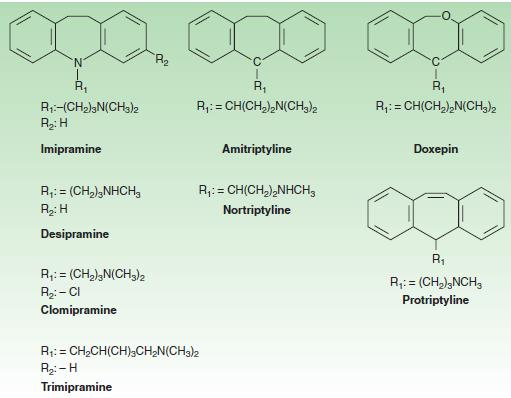
Tricyclic Antidepressants (TCAs)
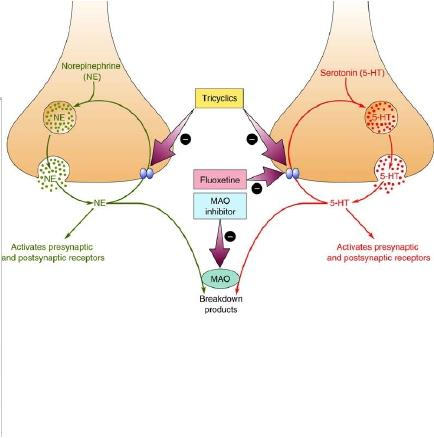
- Monoamine oxidase inhibitors: such as phenelzine and selegiline, are also nonspecific antidepressant
3. Tetracyclic and unicyclic antidepressants
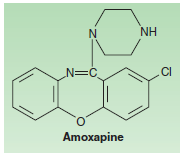
Functions similar to TCAs, at the present time, TCAs and Tetracyclic antidepressants are used primarily in depression that is unresponsive to more commonly used antidepressants such as the SSRIs or SNRIs.
Clinical Pharmacology of Antidepressants
1. Clinical Indications
Depression
- Recurrence in a lifetime (approximately 85%)
- Long‐term maintenance treatment if they have had two or more serious MDD episodes in the previous 5 years or three or more serious episodes in a lifetime.
Anxiety Disorders
- A number of SSRIs and SNRIs have been approved for all the major anxiety disorders, including PTSD, OCD, social anxiety disorder, GAD, and panic disorder.
Pain Disorders
- Medications that possess both norepinephrine and 5‐HT reuptake blocking properties are often useful in treating pain disorders. (TCAs and SNRIs)
Premenstrual Dysphoric Disorder:
- SSRIs, eg: Fluoxetine
Smoking Cessation:
- Bupropion, as effective as nicotine patches
Eating Disorders:
- Bupropion
- Antidepressants appear to be helpful in the treatment of bulimia but not anorexia.
2. Adverse Effects
Selective Serotonin Reuptake Inhibitors
- Gastrointestinal symptoms: Increased serotonergic activity in the gut is commonly associated with nausea, gastrointestinal upset, diarrhea
Serotonin‐Norepinephrine Reuptake Inhibitors and Tricyclic Antidepressants Gastrointestinal symptoms as SSRI
- Increased blood pressure and heart rate
- CNS activation: insomnia, anxiety, and agitation
5‐HT2 Antagonists
- Sedation and gastrointestinal disturbances
3. Overdose
The most common method used in suicide attempts, and antidepressants, especially the TCAs, are frequently involved
- Induction of lethal arrhythmias, including ventricular tachycardia and fibrillation. In addition, blood pressure changes and anticholinergic effects including altered mental status and seizures
Psychotic Symptoms
- Schizophrenia
- Bipolar disorder
- Psychotic depression
- Senile psychoses
- Drug-induced psychoses
Besides treating the above symptoms, antipsychotics are also able to improve mood and reduce anxiety and sleep disturbances
1. Psychosis
Psychosis may be acute or chronic.
- When acute—may be confusion or delirium. Can be precipitated by illness, drug effects or superimposed on chronic dementias.
Psychosis—severe mental disorder charac. By disordered thought processes, inappropriate emotional responses, bizarre behavior, agitation, aggressiveness, hostility, social withdrawal, deterioration in occupational and social functioning, hallucinations and paranoid delusions
Hallucinations—sensory perceptions of people or objects that are not present. Unable to distinguish between false perceptions and reality
In schizophrenia or bipolar disorder, usually auditory; in dementia usually are visual.
Delusions are false beliefs that persist in absence of reason or evidence. May believe others control their thoughts, feelings or seek to harm them
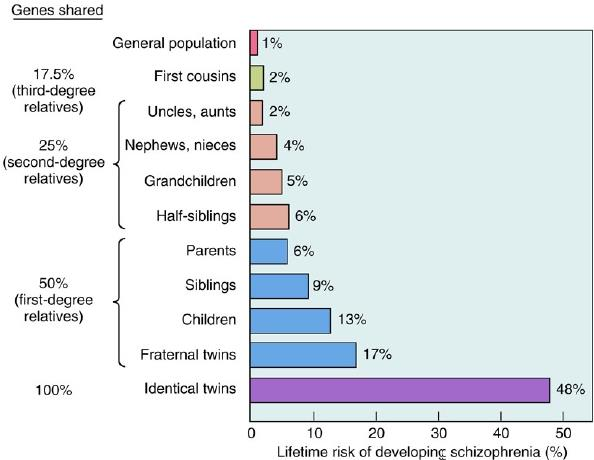
2. Schizophrenia
Consists of a variety of related disorders
Does have a genetic predisposition
Positive symptoms include CNS stimulation, agitation, behavioral disturbances, delusions, hallucinations, insomnia, and paranoia.
Negative symptoms include anhedonia, lack of motivation, blunted affect, poor hygiene, poor social skills and social withdrawal
Nature of Psychosis & Schizophrenia:
The Serotonin Hypothesis of Schizophrenia
5-HT2A-receptor:
- Indole hallucinogens such as LSD (lysergic acid diethylamide) is a serotonin (5-HT) agonists. The 5-HT2A-receptor stimulation was the basis for the hallucinatory effects of these agents.
Drugs to 5-HT2A-receptor:
- 5-HT2A-receptor blockade is a key factor in the mechanism of action of the main class of atypical antipsychotic drugs such as clozapine and quetiapine. These drugs block the constitutive activity of 5-HT2A receptor (inverse agonist). These receptors modulate the release of dopamine in the cortex, limbic region, and striatum. Stimulation of 5HT2A receptors leads to depolarization of glutamate neurons, but also stabilizes NMDA receptors on postsynaptic NMDA receptors.
5-HT2C-receptor:
- 5-HT2C-receptor stimulation provides a further means of modulating cortical and limbic dopaminergic activity.
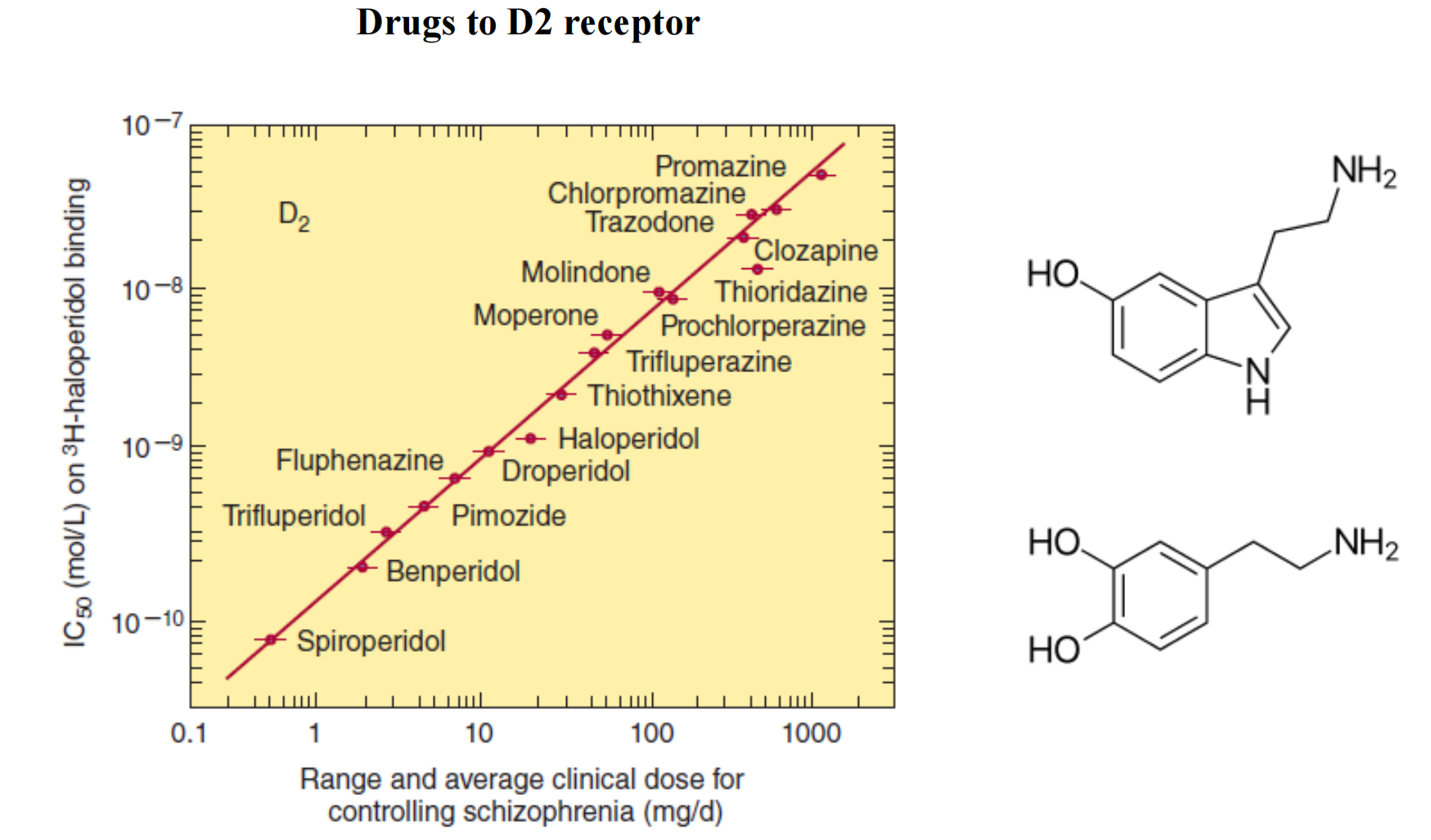
The Dopamine Hypothesis of Schizophrenia
Evidence: excessive limbic dopaminergic activity plays a role in psychosis:
- Many antipsychotic drugs strongly block postsynaptic D2 receptors in the central nervous system, especially in the mesolimbic and striatal-frontal system; this includes partial dopamine agonists, such as aripiprazole and bifeprunox
- Drugs that increase dopaminergic activity, such as levodopa, amphetamines, and bromocriptine and apomorphine, either aggravate schizophrenia psychosis or produce psychosis de novo in some patients.
- Dopamine-receptor density has been found postmortem to be increased in the brains of schizophrenics who have not been treated with antipsychotic drugs.
- Some postmortem schizophrenic subjects have increased dopamine levels and D2-receptor density in the nucleus accumbens, caudate, and putamen.
- Imaging studies have shown increased amphetamine-induced striatal dopamine release, increased baseline occupancy of striatal D2 receptors by extracellular dopamine.
(1) Dopamine
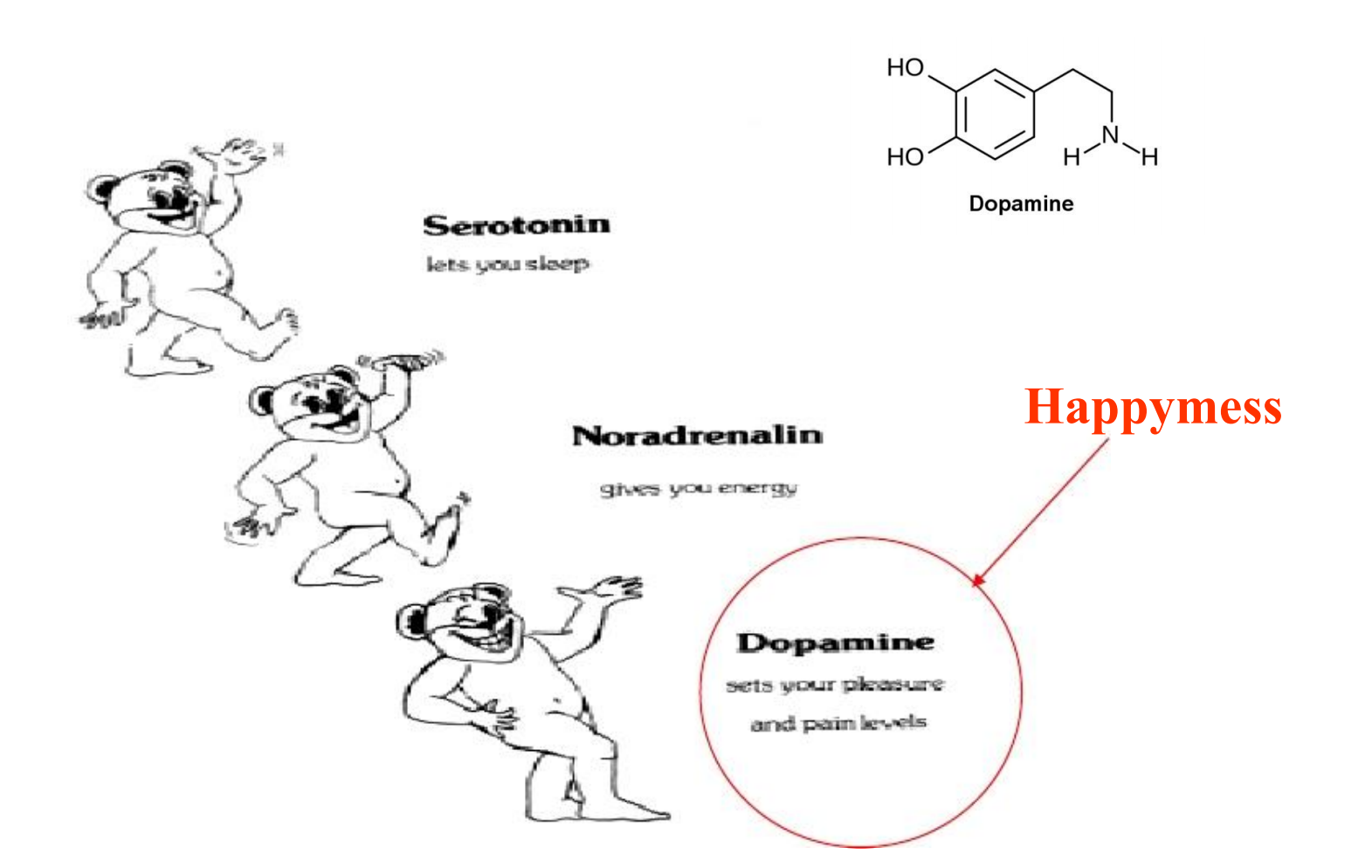
(2) Dopamine in brain
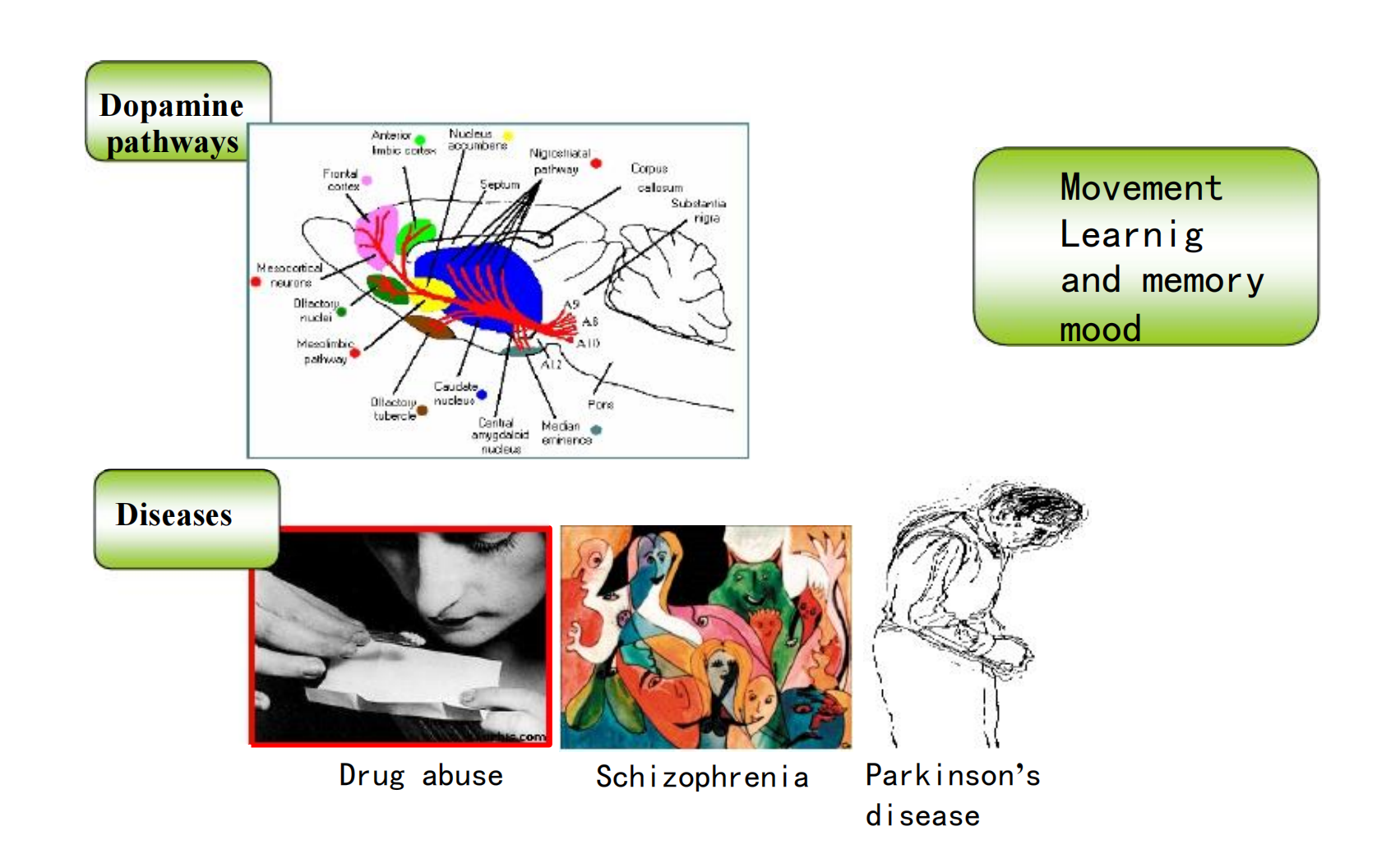
(3) The Dopamine Hypothesis of Schizophrenia
Rethinking:
- Several of the atypical antipsychotic drugs have much less effect on D2 receptors and yet are effective in schizophrenia.
The atypical antipsychotic drugs share the property of weak D2-receptor antagonism and more potent 5-HT2A-receptor blockade.
(4) Dopamine receptor and their effects
(5) Dopamine system
The antipsychotic action is now thought to be produced (at least in part) by their ability to block dopamine in the mesolimbic and mesocortical systems, which are involved in cognitive control, motivation, and emotional response
Antipsychotic Drugs
Categorized as “typical”, “first-generation” or “conventional”== phenothiazines
“Atypical” or “second-generation”==newer nonphenothiazines
Typicals include phenothiazine and haloperidol, developed in the 1950s, but have parkinson-like side effects
Antipsychotic agents:
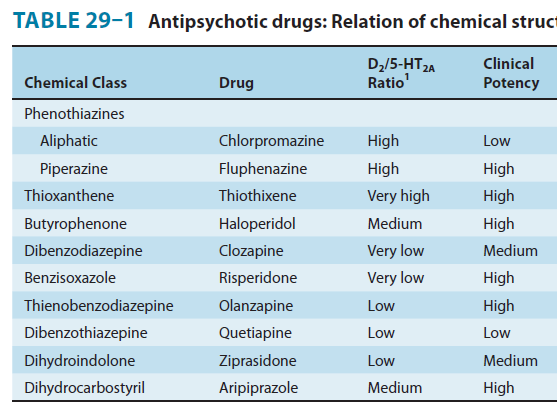
1. Differences among antipsychotic drugs
A summary of the relative receptor-binding affinities of several key agents :
- Chlorpromazine: α1 = 5-HT2A > D2 > D1
- Haloperidol: D2 > α1 > D4 > 5-HT2A > D1 > H1
- Clozapine: D4 = α1 > 5-HT2A > D2 = D1
- Olanzapine: 5-HT2A > H1 > D4 > D2 > α1 > D1
- Aripiprazole: D2 = 5-HT2A > D4 > α1 = H1 >> D1
Thus, most of the atypical and some typical antipsychotic agents are at least as potent in inhibiting 5-HT2 receptors as they are in inhibiting D2 receptors
2. Psychological effects
Nonpsychotic persons also experience impaired performance as judged by a number of psychomotor and psychometric tests. Psychotic individuals, however, may actually show improvement in their performance as the psychosis is alleviated
3. Clinical Pharmacology
Indications-Psychiatric indications
Schizophrenia: benzodiazepine
Psychotic Bipolar Disorder : benzodiazepine + lithium
psychotic depression, and treatment resistant depression.
- Olanzapine + Fluoxetine
Schizoaffective Disorders, which share characteristics of both schizophrenia and affective disorders. The manic phase in bipolar affective disorder often requires treatment with antipsychotic agents
Others: Tourette’s syndrome, Alzheimer’s disease, psychotic depression
4. Lithium and others
Nature of bipolar disorder
Manic phase: excitement, hyperactivity, impulsivity, disinhibition, aggression, diminished need for sleep, psychotic symptoms in some (but not all) patients, and cognitive impairment.
Depressive phase: depressed mood, diurnal variation, sleep disturbance, anxiety, and sometimes, psychotic symptoms. Mixed manic and depressive symptoms are also seen. Patients with bipolar disorder are at high risk for suicide
Bipolar disorder, once known as manic-depressive illness, is a psychotic disorder distinct from schizophrenia.
Lithium was the first agent shown to be useful in the treatment of the manic phase of bipolar disorder. Lithium continues to be used for acute-phase illness as well as for prevention of recurrent manic and depressive episodes.
Others:
- Carbamazepine and valproic acid for the treatment of acute mania and for prevention of its recurrence
- Lamotrigine is approved for prevention of recurrence. Gabapentin
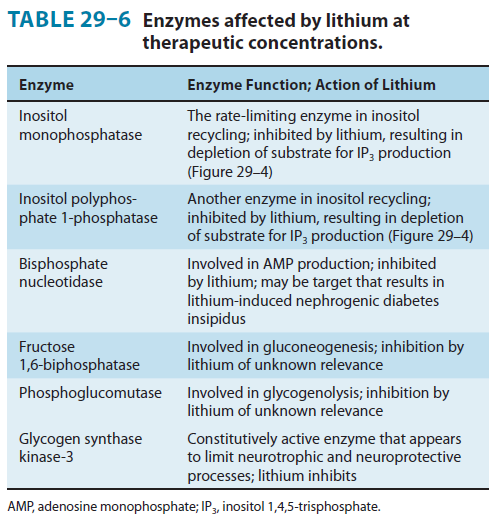
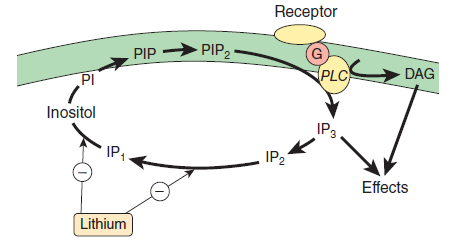
Phamacodynamics
Clinical Pharmacology of Lithium
Applications
- Bipolar Affective Disorder
- Other Applications
- Recurrent endogenous depression with a cyclic pattern
- Schizoaffective disorder
Other drugs for bipolar disorder
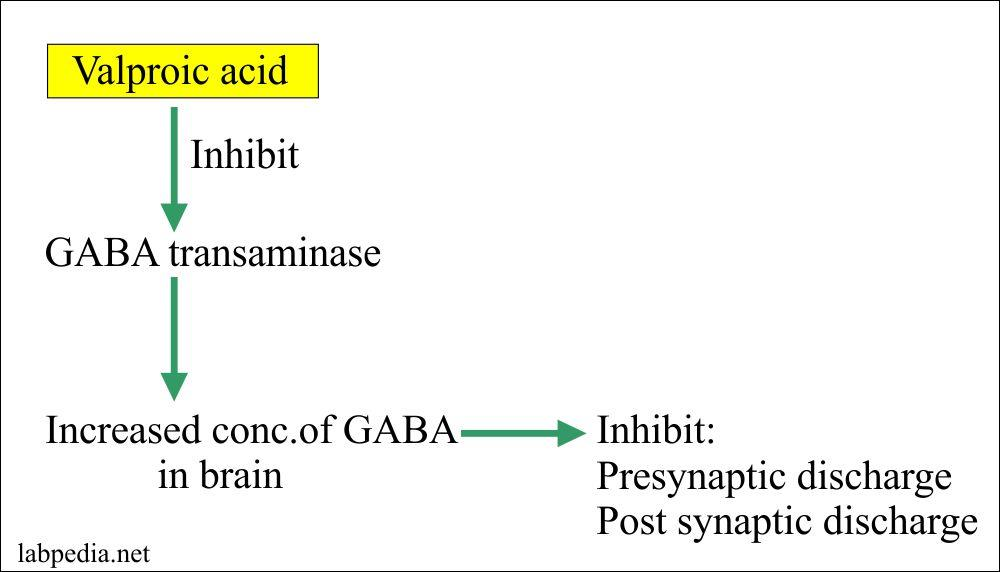
(1) Valproic Acid 丙戊酸
Valproic acid (valproate), an antiepileptic, shows efficacy equivalent to that of lithium during the early weeks of treatment. It is significant that valproic acid has been effective in some patients who have failed to respond to lithium.
四、Drug Selection
Atypicals are drugs of choice as they:
- May be more effective
- Produce milder adverse effects
- Patients display greater compliance in taking them
- Drawbacks include: glucose intolerance, weight gain