L7 Antihypertensive drugs including Vasodilators and anti-diuretics
一、The definition of Hypertension
Hypertension: an elevation of arterial blood pressure above an arbitrarily defined normal value
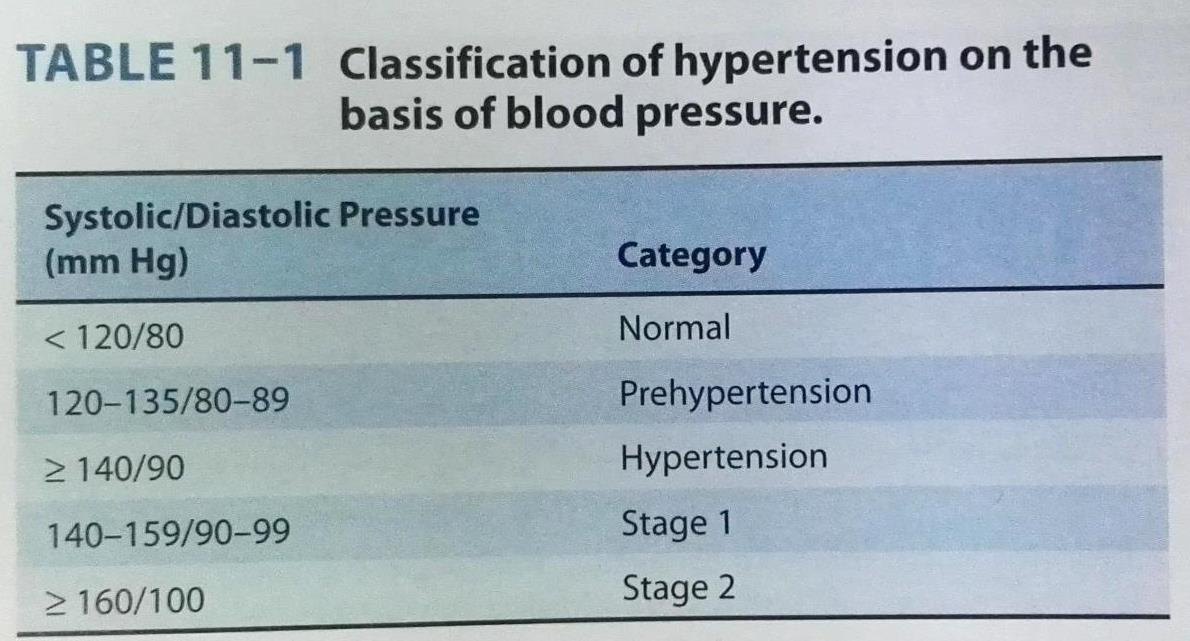
- Risks of damage to kidney, heart and brain are directly related to the extent of blood pressure elevation
General info of hypertension (HTN)
Nearly 90% people will develop HTN
- Causes are not clear for primary HTN
- Diagnosed by Bp measurement, rather than symptoms at the early stage
- Many complications:
- renal failure 肾功能衰竭
- heart failure
- coronary disease 冠状动脉疾病
- Stroke (blood vessel rupture in the brain)
- CV diseases are pressure related
- From 115/75 mmHg, each 20/10 mmHg doubles risk
The cause of Hypertension
Essential or primary hypertension: patients with no specifc cause of hypertension can be found, account for 85-90% of patients
Secondary hypertension: with known cause,could be due to many reasons such as renal artery constriction(肾动脉收缩), coarctation of the aorta(主动脉缩窄), etc.
BP = CO x PVR, Cardiac Output (CO) is mostly normal, whereas peripheral vascular resistance (PVR), the resistance to flow of blood through arterioles, is usually increased in hypertension
Normal regulation of BP
BP = CO x PVR
CO : myocardial contractility & basic filling pressure
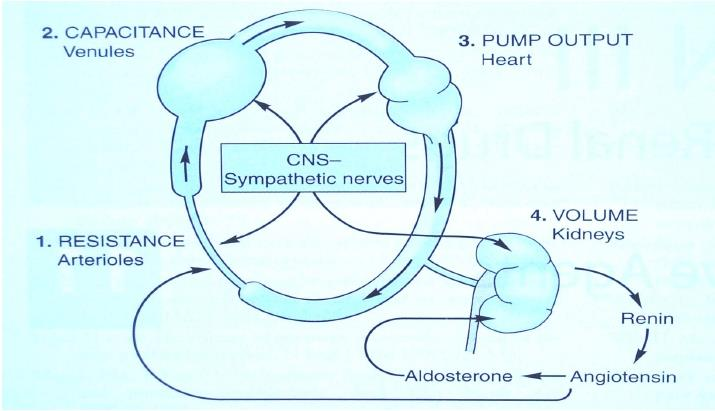
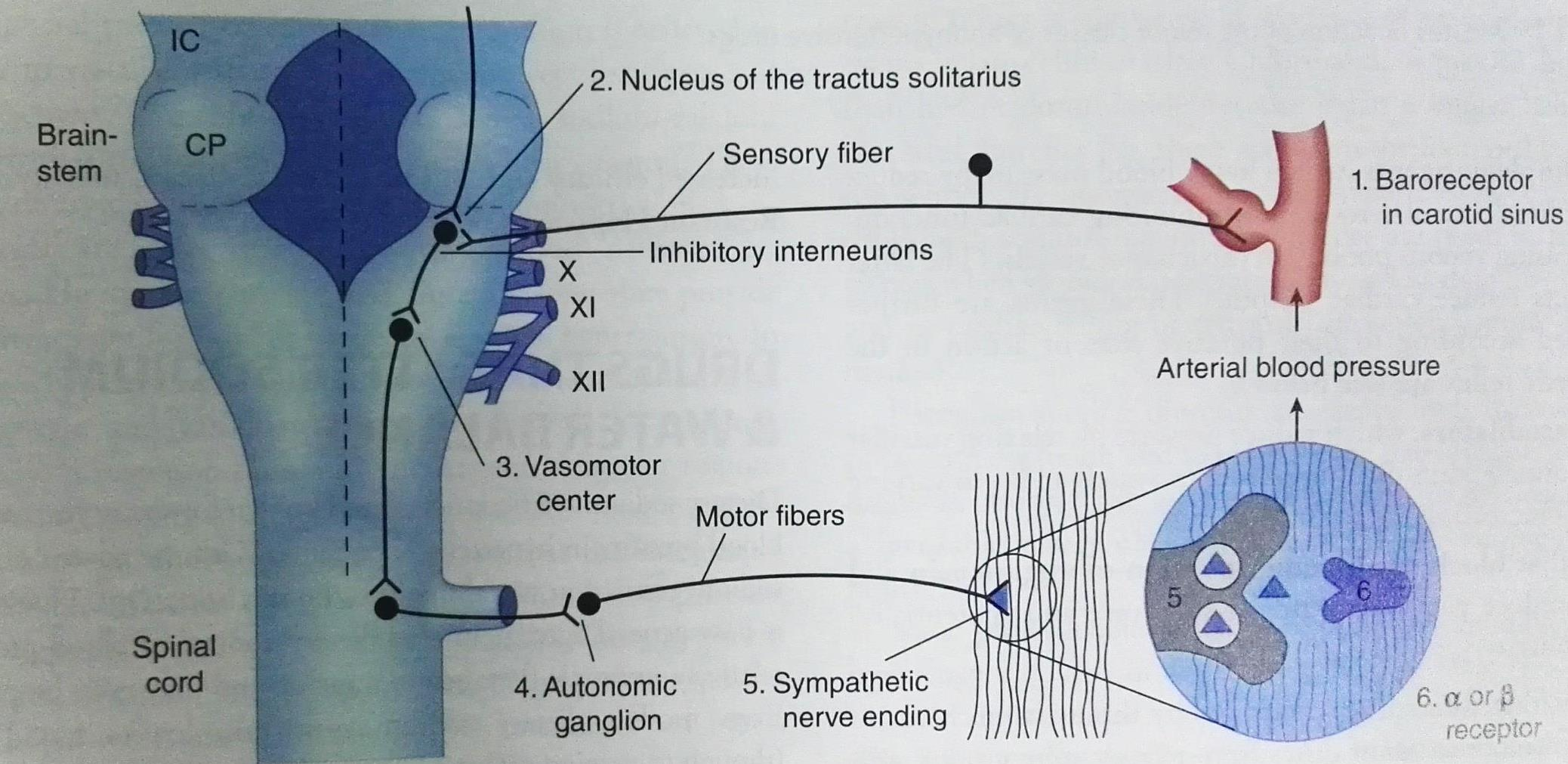
- Hypertensive patients: the baroreceptors and the renal blood volume-pressure control system are set at a higher level of blood pressure
1. Baroreceptor reflex
CNS sympathetic nerves
- Resistance vessels
- Capacitance vessels
- Cardiac output
- Basic filling pressure via kidney
- Renin angiotensin aldosterone system
- Baroreceptor reflex arc

Local released vasoactive substances
Vasodilator
- NE
- Nitric Oxide
- Endothelial - NOS
vasoconstrictive factors
- Angiotensin
- Prostaglandins
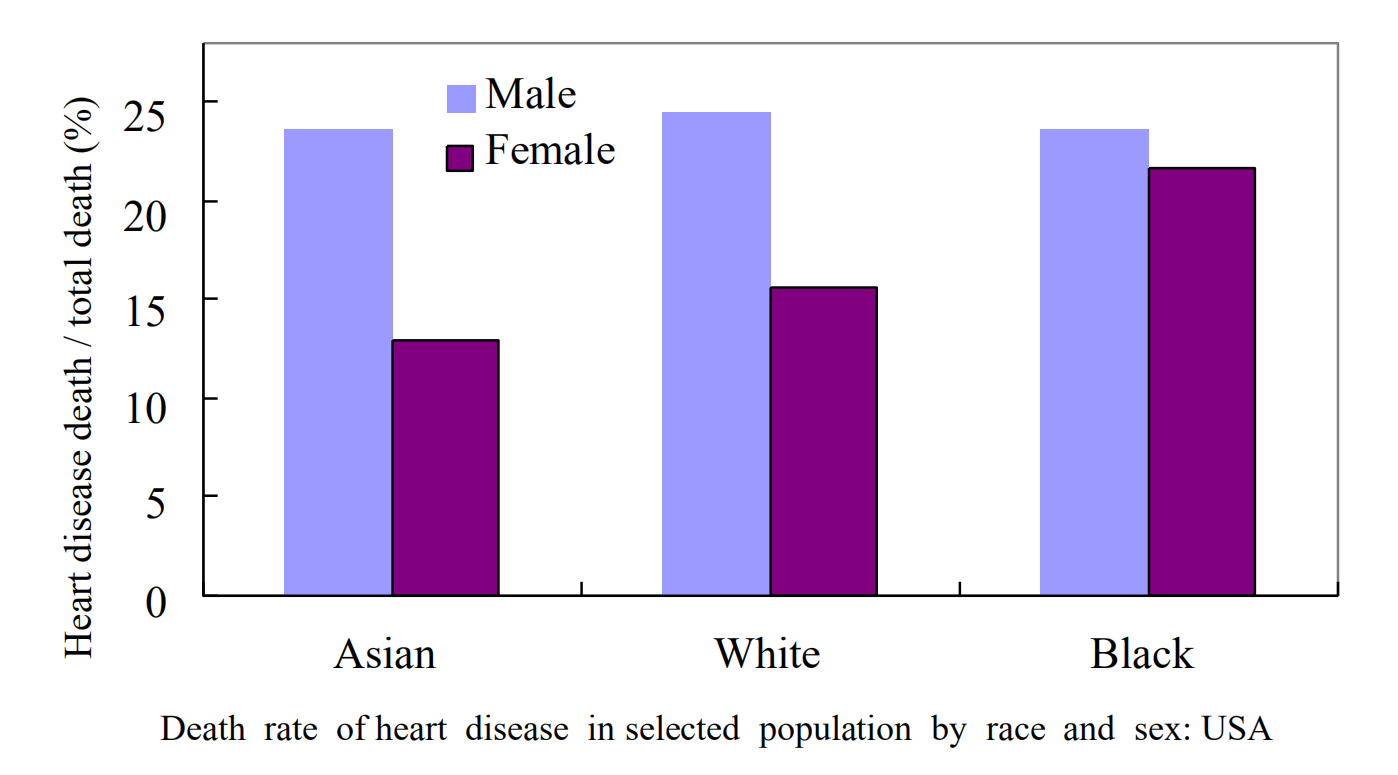
2. Differences
Gender and Ethic difference
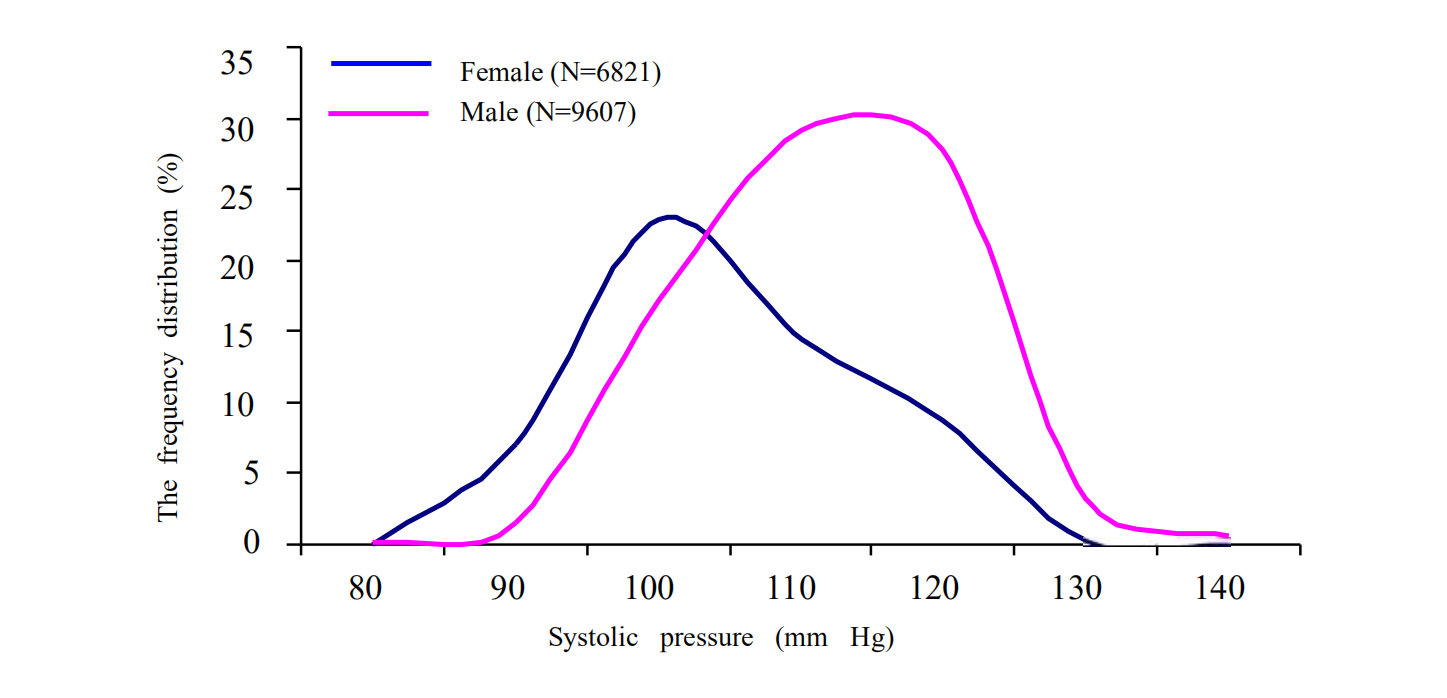
- The frequency distribution of the systolic pressure of 16429 undergraduates
Food: Particularly the salt intake
Physical exercise
Conscious control: Yuga
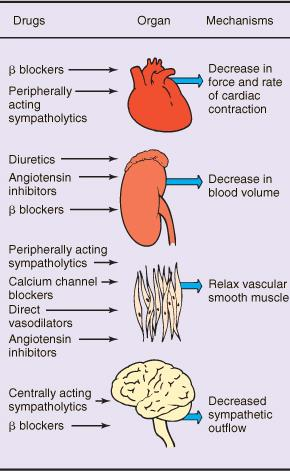
二、Antihypertensive drugs
Major sites of antihypertensive drugs
brain-heart-vessels-kidney
- Diuretics: Drugs that alter sodium and water balance (kidney)
- Alter sympathetic NS:
- Centrally acting sympathoplegic drugs
- Ganglion‐blocking agents
- Adrenergic neuron‐blocking agents
- Adrenoceptor antagonists: beta & alpha blockers
- Vasodilators (Blood vessel)
- Act on angiotensin system (kidney):
- ACEI & receptor blockers
- Calcium channel blockers
- calcium will cause constriction
Drugs alter sympathetic NS
1. Drugs
- methyldopa 甲基多巴
- Clonidine 可乐定
- Guanethidine 胍乙啶
- Reserpine 利血平
- Propranolol(心得安) and other beta antagonist
useful in polytherapy in moderate to severe HTN
2. Different Side Effects
CNS: sedation, depression, nightmares
ganglia: inhibition parasympathetic system as well
sympathetic end (NE release): ejection (-), postural hypotension
block postsynaptic receptors: more selective effects
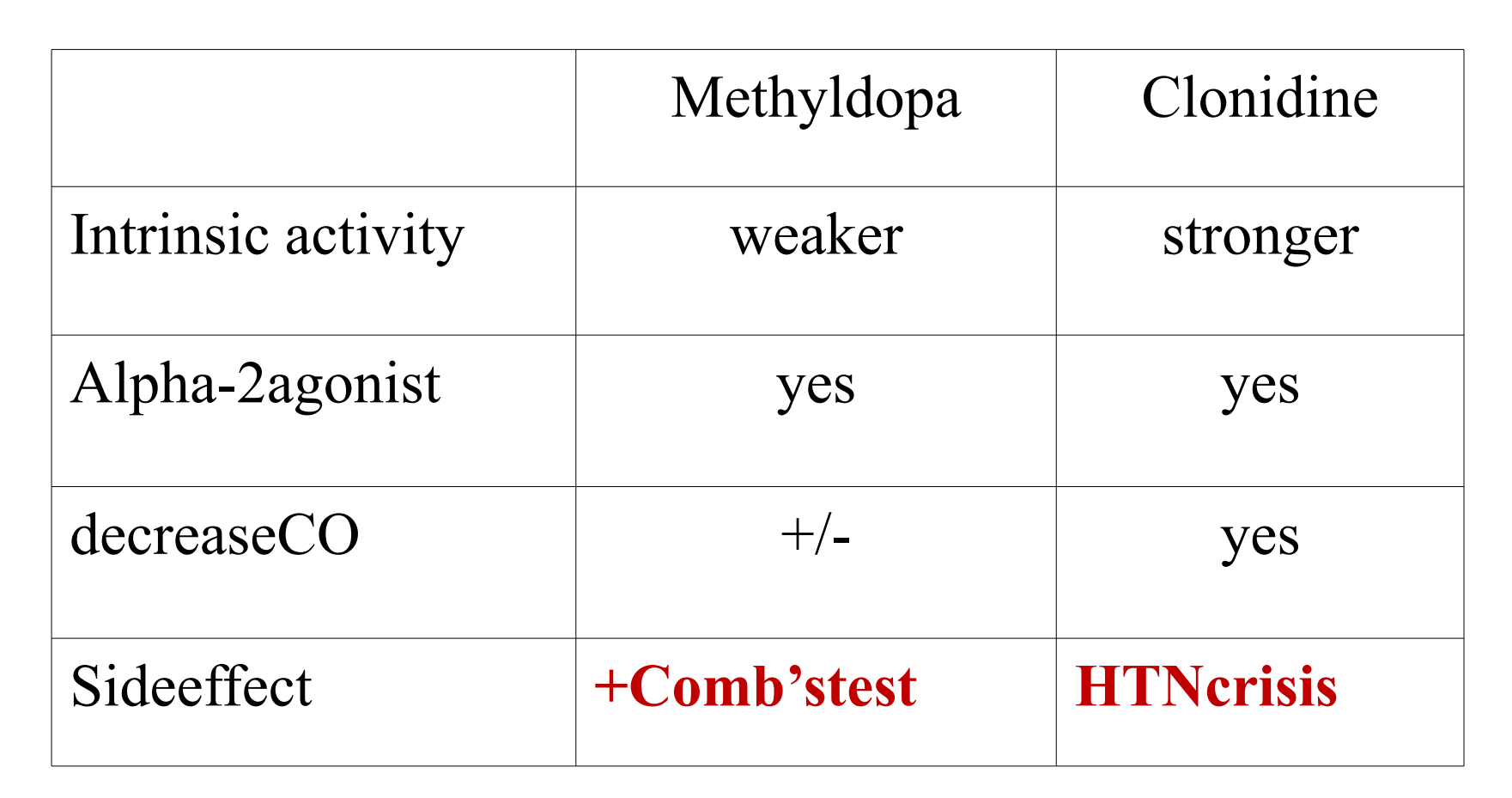
3. methyldopa
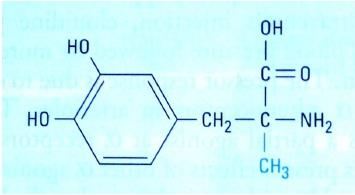
- structure just like dopamine
Enters CNS via Aromatic amino acid transport
Converts into alpha-methyldopamine & alpha-methylNE
Partial alpha agonist: initial ↑BP by stimulating vascular receptor, & then ↓ BP by stimulating CNS alpha-2 receptors
↓BP mainly by reducing PVR
4. Clonidine
Specificity towards the presynaptic α2 receptors in the vasomotor center in the brainstem. This binding has a sympatholytic effect, suppresses release of norepinephrine, ATP, renin
↓BP by ↓cardiac output and ↓PVR ( maintaining renal blood supply)
Major sites of antihypertensive drugs
Ganglion‐blocking agents: historically, 1st generation of antihypertensive drugs (trimethaphan);
Competitively block Nicotinic Cholinoceptors on postganglionic Neurons in both sympathetic and parasympathetic ganglia., or they may directly block the nicotinic acetylcholine channel.
Most such drugs are no longer available clinically because of intolerable toxicities related to their primary action.
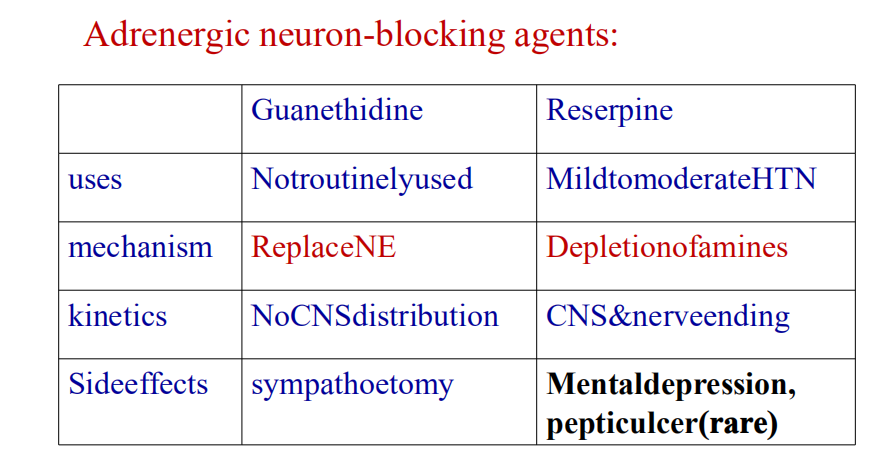
1. Adrenergic neuron-blocking agents
Guanethidine
- replace NE, gradual depletion of NE store in the nerve ending
Reserpine
- Block monoamine transporter VMAT, inhibits NE uptake into synaptic vesicles
- uptake ≠ reuptake
Antihypertensive effects
- short term: ↓CO, ↓ capacitance vessels;
- long term: ↓ PVR sedation,
Adrenoceptor antagonists (1): the prototype
Propranolol: Nonselective beta-blocker, preventing reflex tachycardia, reduce mortality in heart failure
- Effects: ↓CO, CNS inhibition, ↓renin production
Side effects: related to beta blockage at heart, bronchi, vessels, pancreas; should not be discontinued abruptly
Adrenoceptor antagonists (2): good for asthma
Metoprolol(美托洛尔): relatively selective beta-1-blocker, 50-100-fold less potent than propranolol in blocking beta-2 receptor (expressed on metabolic organs)
Indications: HTN with asthma, diabetes, or peripheral vascular diseases
Adrenoceptor antagonists (6): Esmolol 艾司洛尔
Short T1/2
- Property: beta-1-selective, and short T1/2 (9-10 min)
- Indications: lowring BP in operation, postoperation, & HTN emergencies
Question: why is this short effective drug advantageous in dealing with HTN during operation ?
- A drug with short duration of action can be discontinued quickly, less danger for heart failure
Adrenoceptor antagonists (7): alpha-1-specific blockers
Prazosin (T1/2: 4h)
- Mechanisms: block alpha-1; & allow alpha-2 (-) feedback
- Prazosin 哌唑嗪
- Decrease BP mainly via dilating vessels
- More effective when combined with beta blockers or diuretics
Vasodilators 血管舒张剂
Oral: outpatient
Parental: HTN emergencies
Calcium channel blockers: for both
Work best in combination with other drugs to oppose the compensatory CV responses
Oral vasodilators: Hydralazine vs minoxidil Mechanistic target still unknown
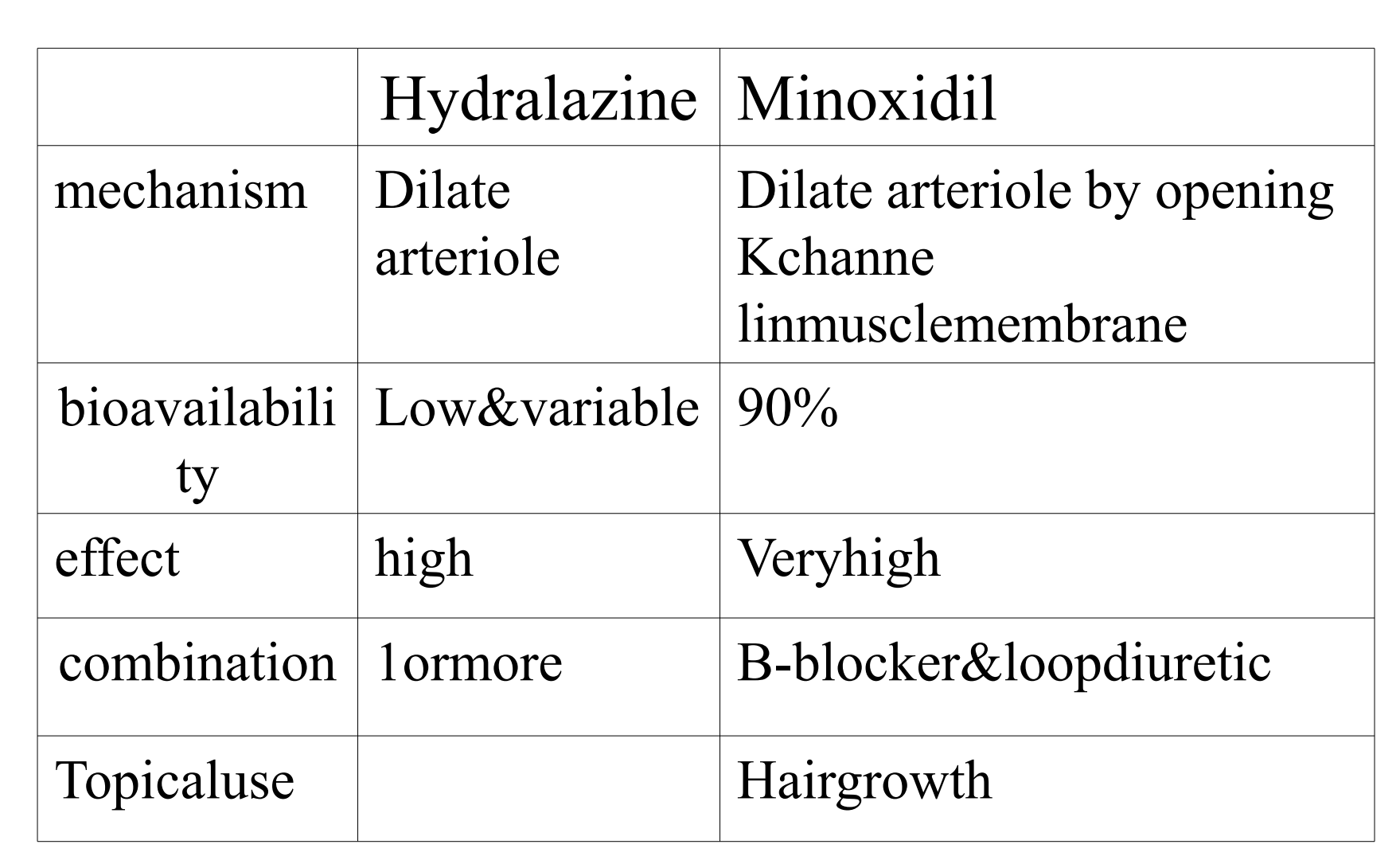
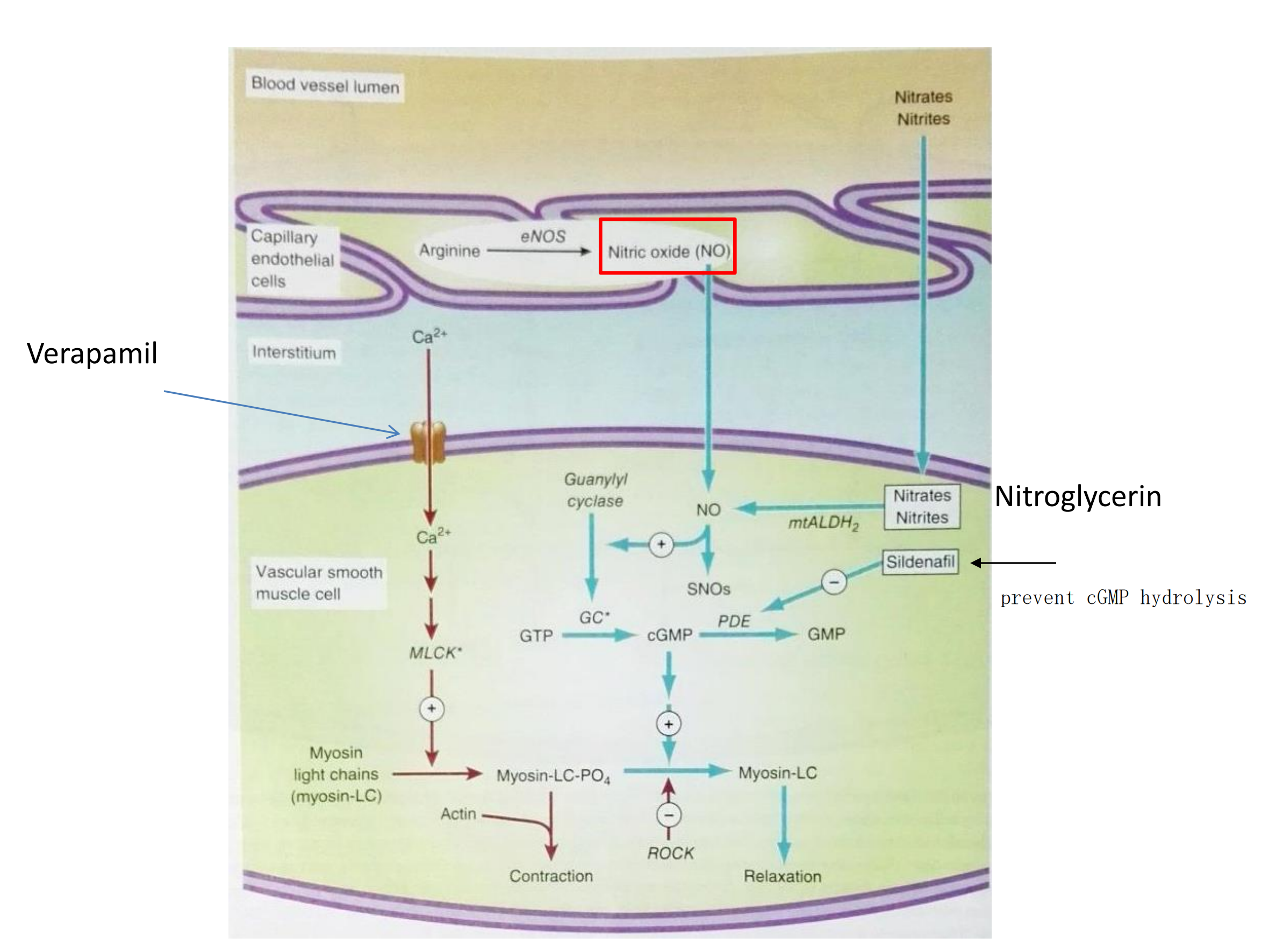
- Nitroprusside(硝普钠): Dilates arterial & venous vessels through increased cGMP
- Increased CO in HTN with heart failure
- Effects disappeared within 10 minutes, light sensitive
- Diazoxide(氯甲苯噻嗪): Dilates arterial vessels, K+ channel opener (calcium channel close)
- Occasionally used to treat HTN emergencies
- Side effects: extensive hypotension
- Tips: Diazoxide and Thiozoxide are structurally similar, the former causes salt & water retention, while the latter has been used as diuretics.
- hypotention is very lethal, so there are not hypotension patients
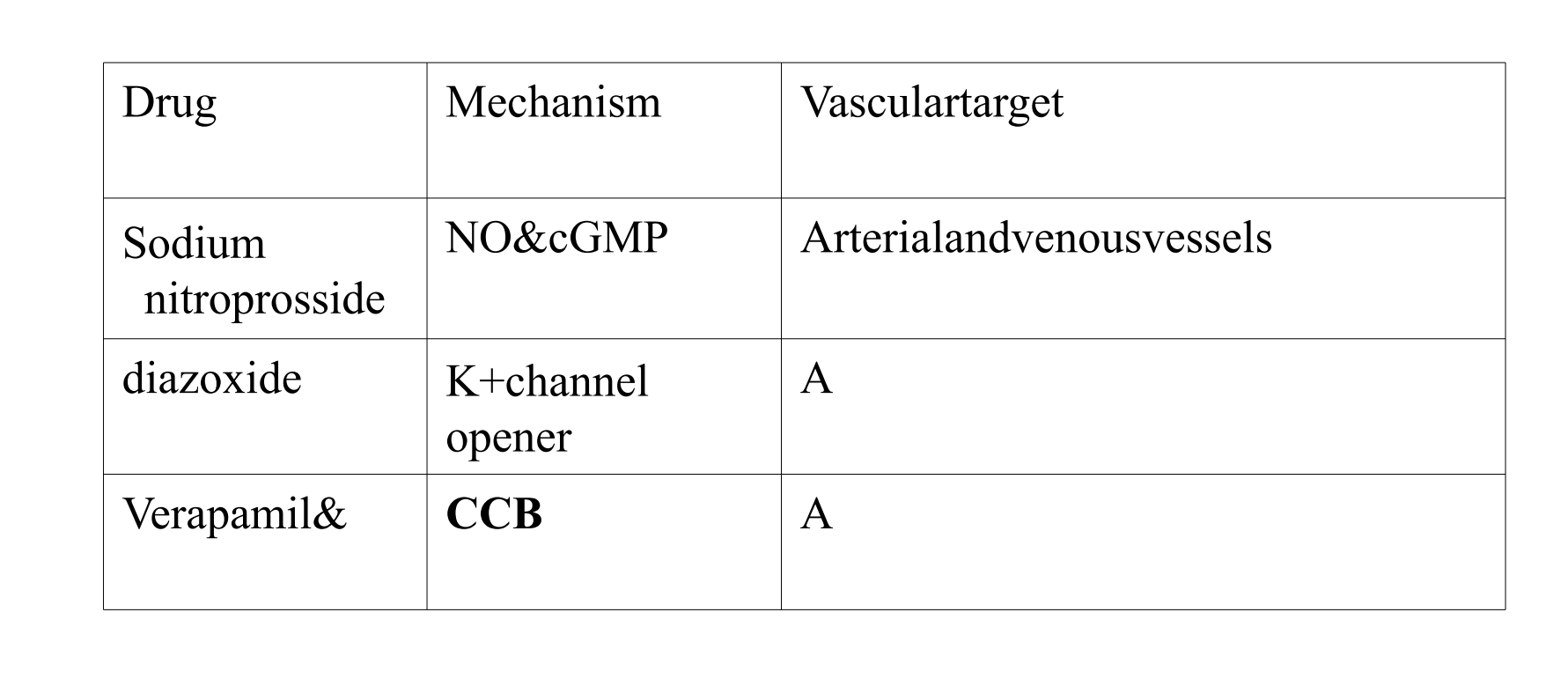
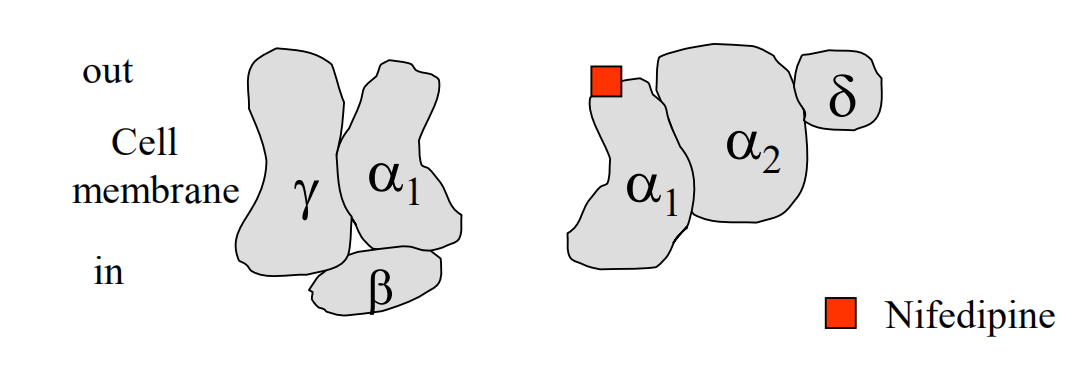
CCBs (Calcium channel blockers) – Mechanisms of Action
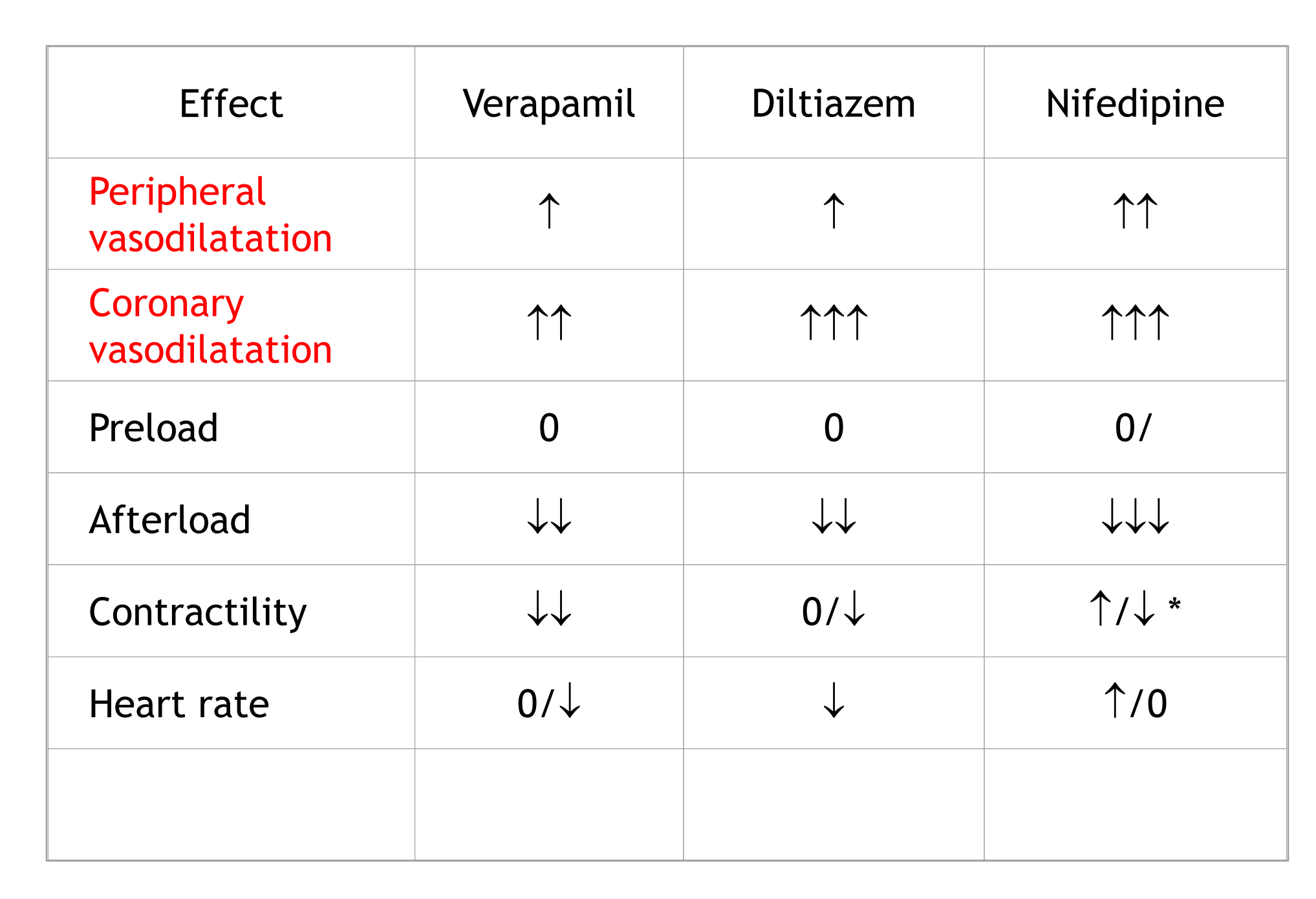
Increase the time that Ca2+ channels are closed
Relaxation of the arterial smooth muscle but not much effect on venous smooth muscle
Significant reduction in afterload (blood coming out of heart), but not preload (blood goes into heart).
The α1C subunit of the L-type Ca2+ channel is the pore-forming subunit
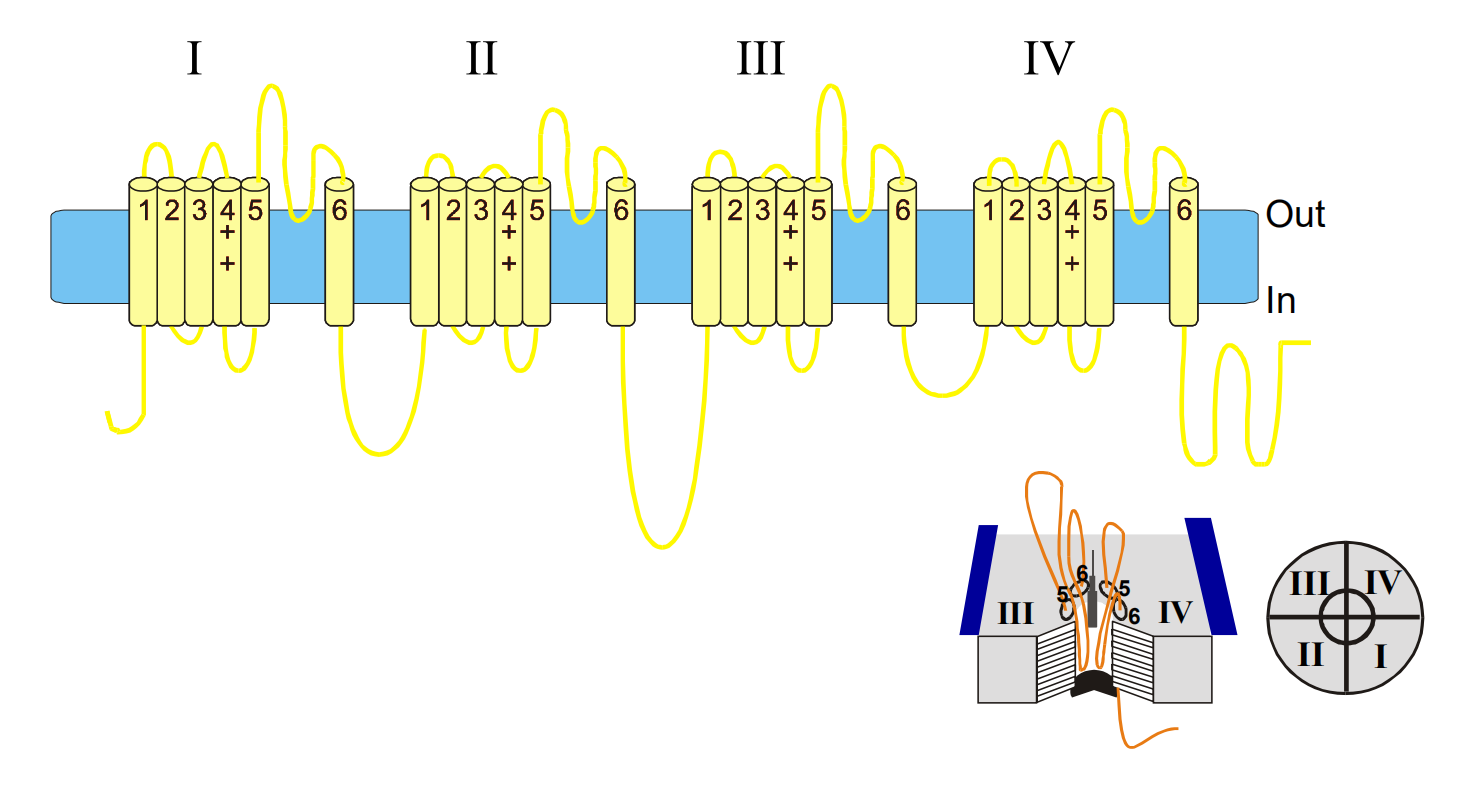
The expression and function of the α1C subunit is modulated by other smaller subunits
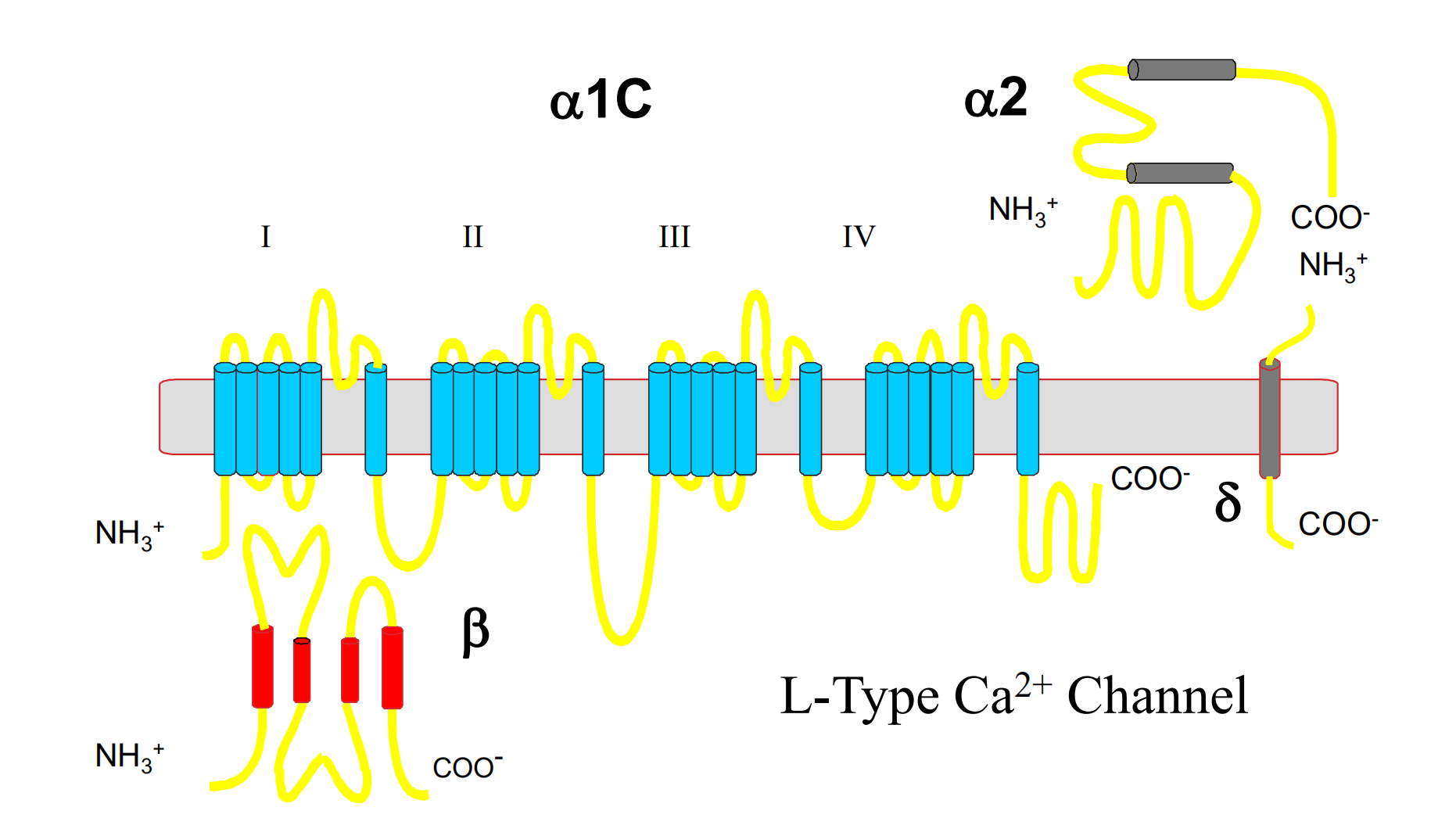
The different binding sites of CCBs result in differing pharmacological effects
Use-dependent binding (targets cardiac cells):
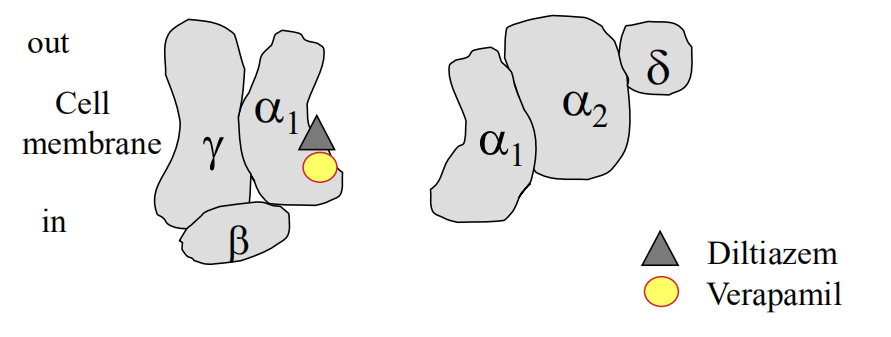
Voltage-dependent binding (targets smooth muscle):
Hemodynamic Effects of CCBs
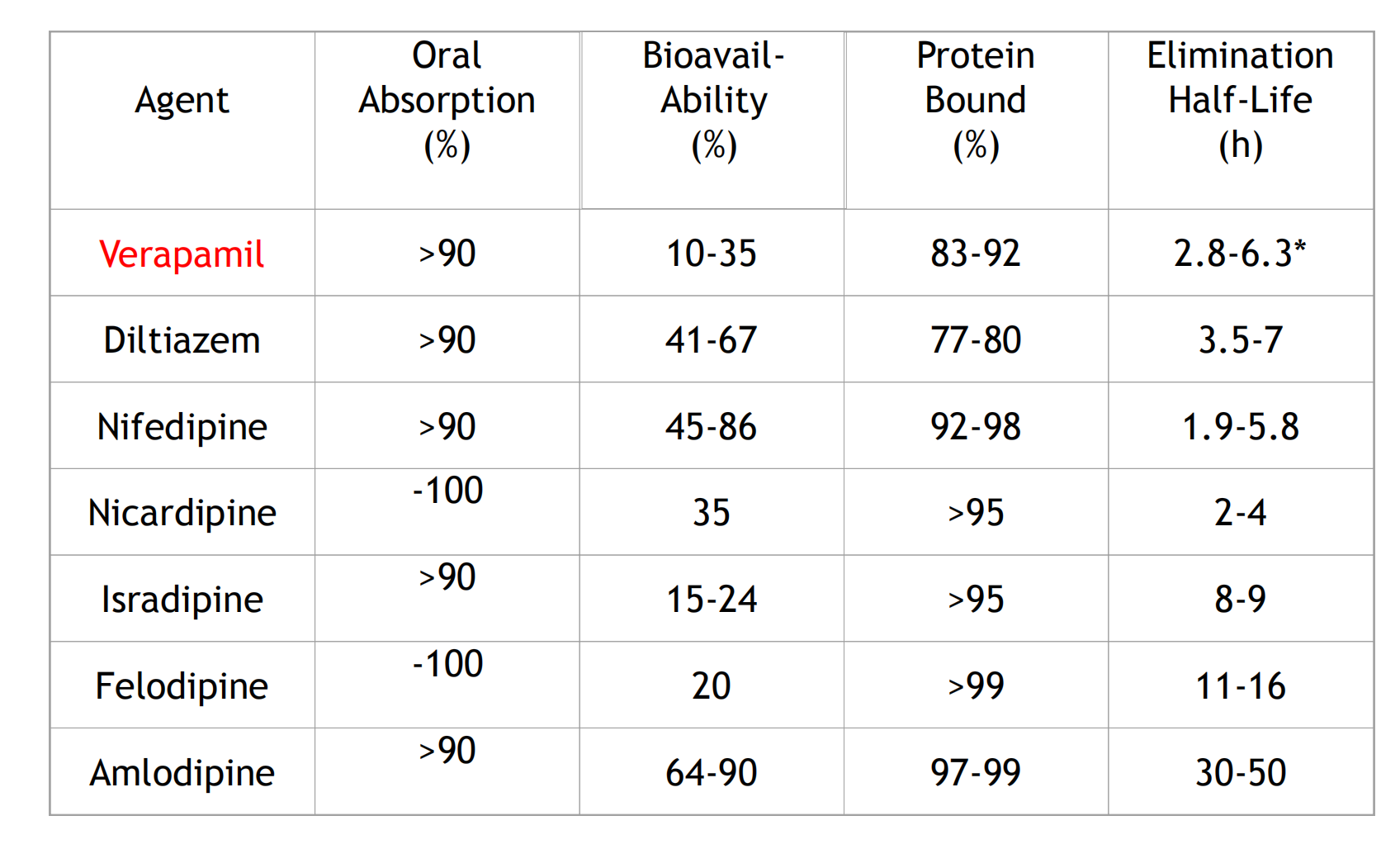
CCBs: Pharmacokinetics
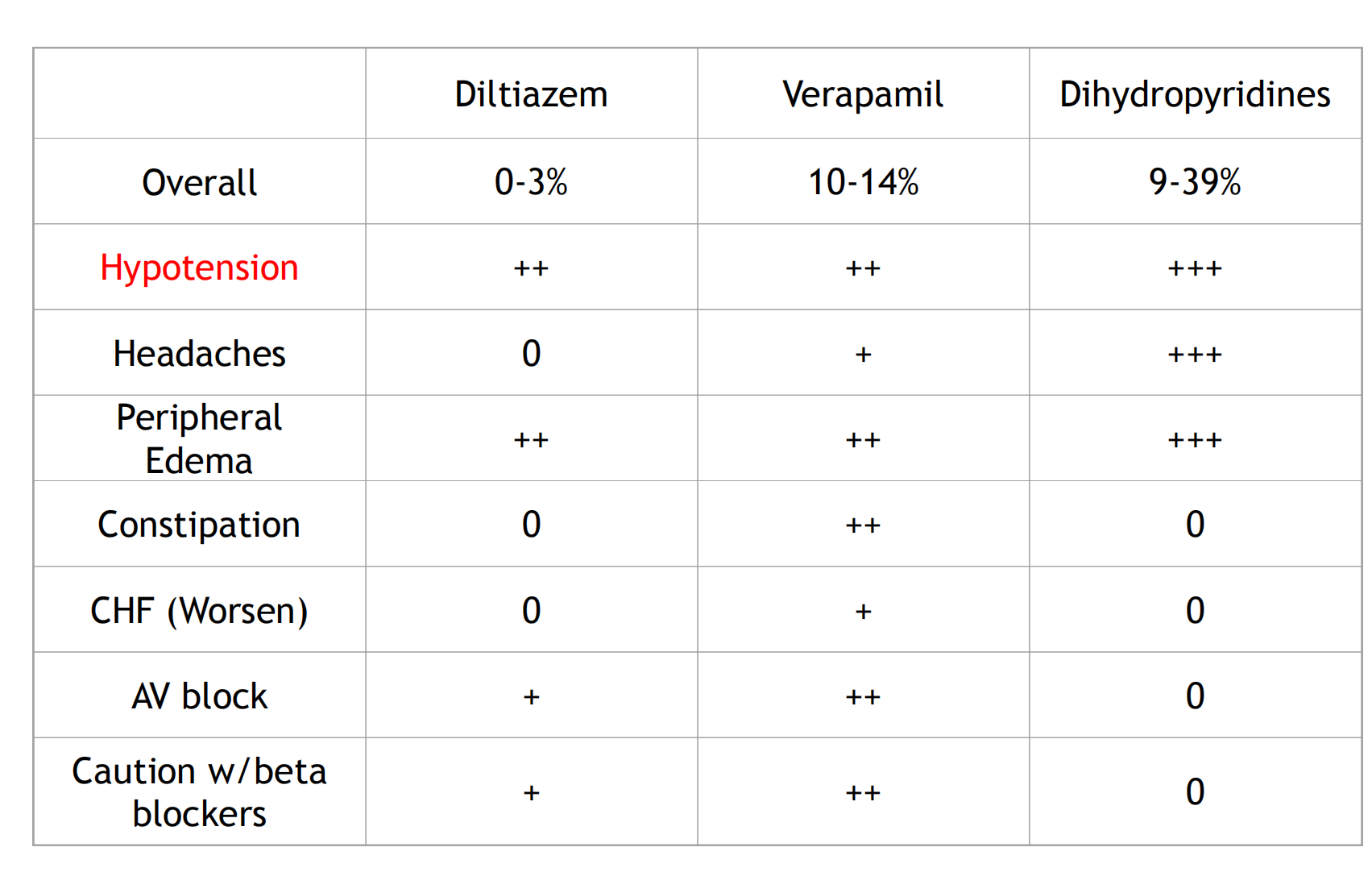
Comparative Adverse Effects
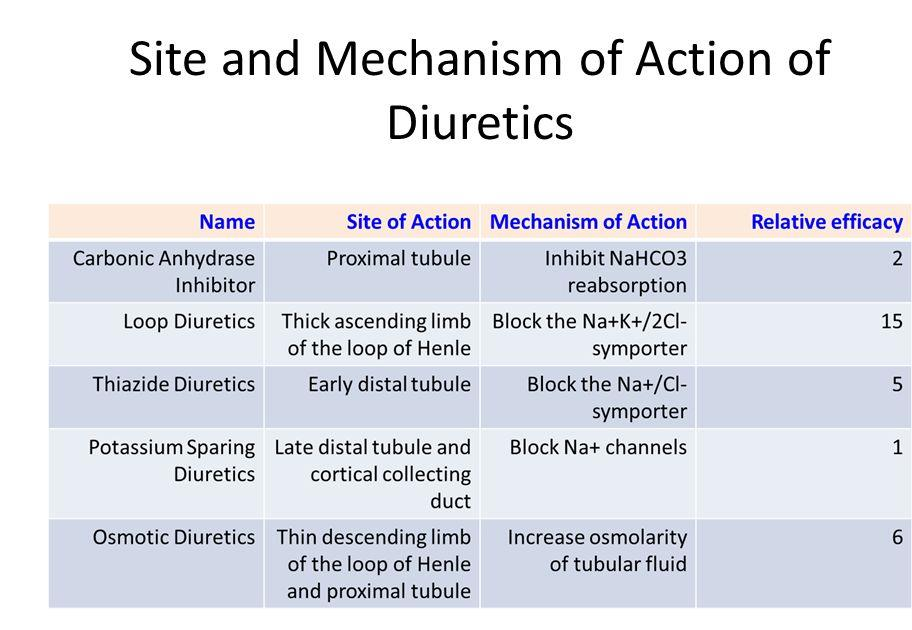
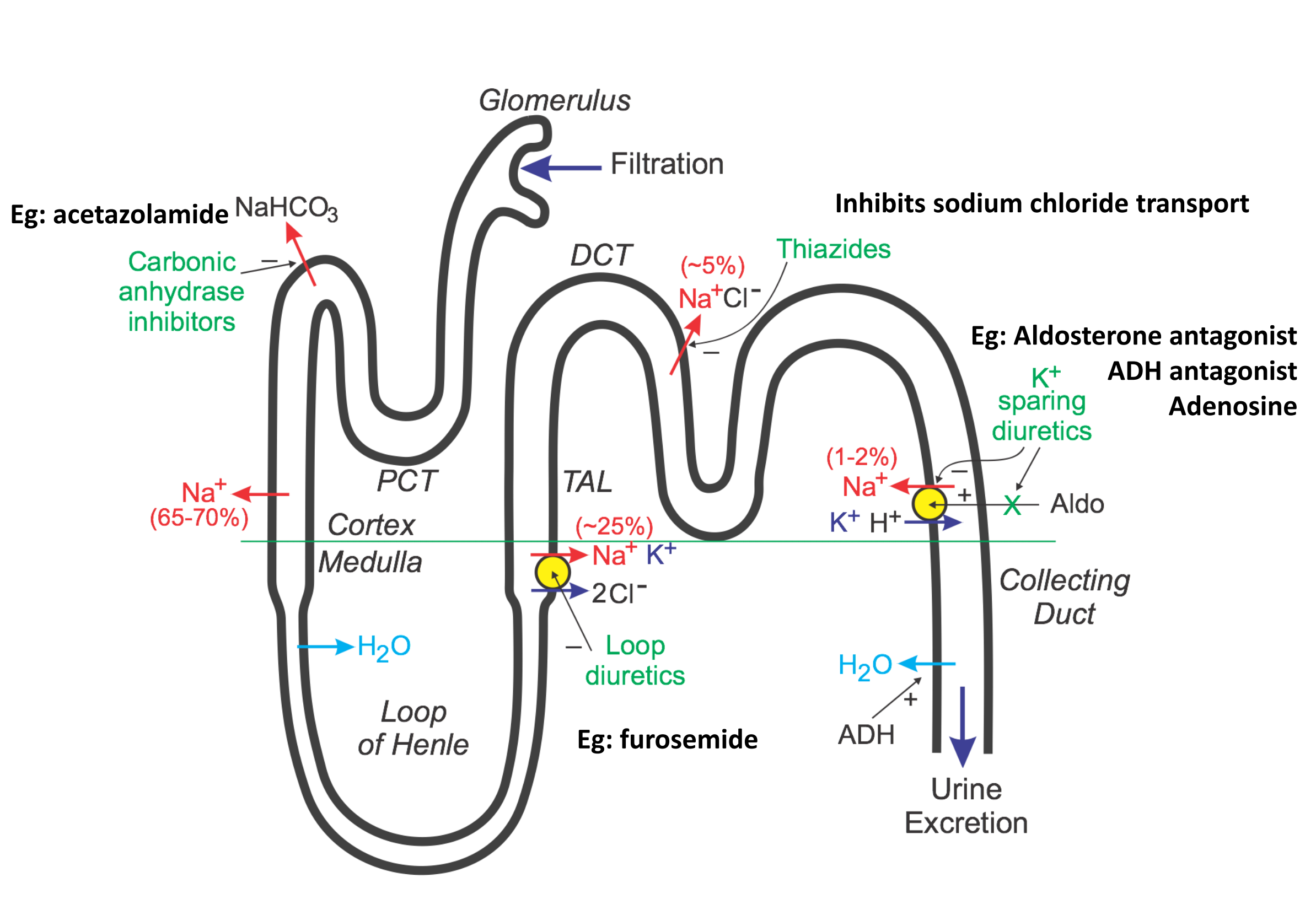
Diuretic agents
Diuretics: for mild or moderate essential HTN,
- can lower10-15 mmHg;
- natriuretic
- direct vasodilatory effect decrease body volume
Dietary sodium restriction is better for prevention
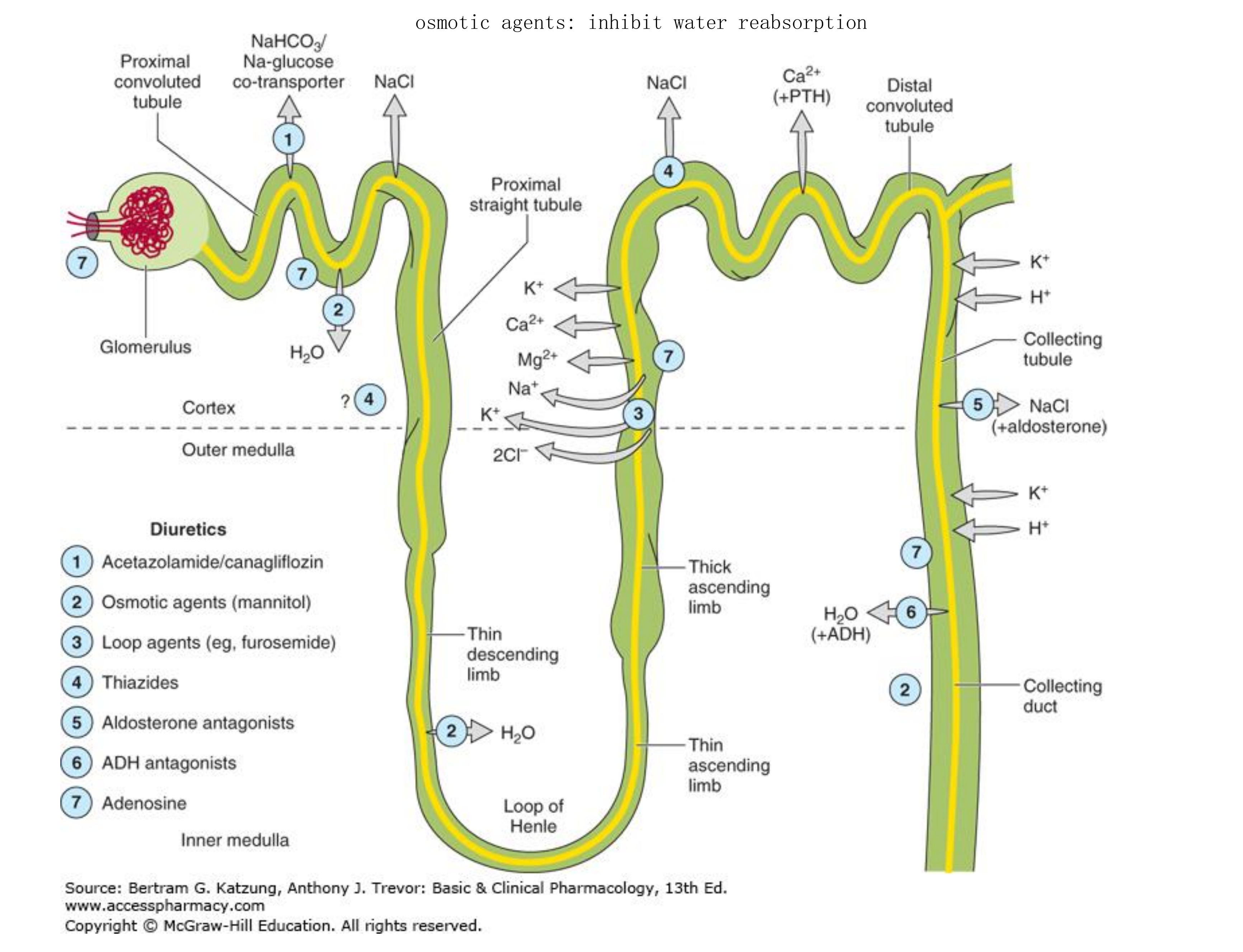
- osmotic agents: inhibit water reabsorptions
1. basic pharmacology of diuretic agents (1)
Carbonic anhydrase inhibitor
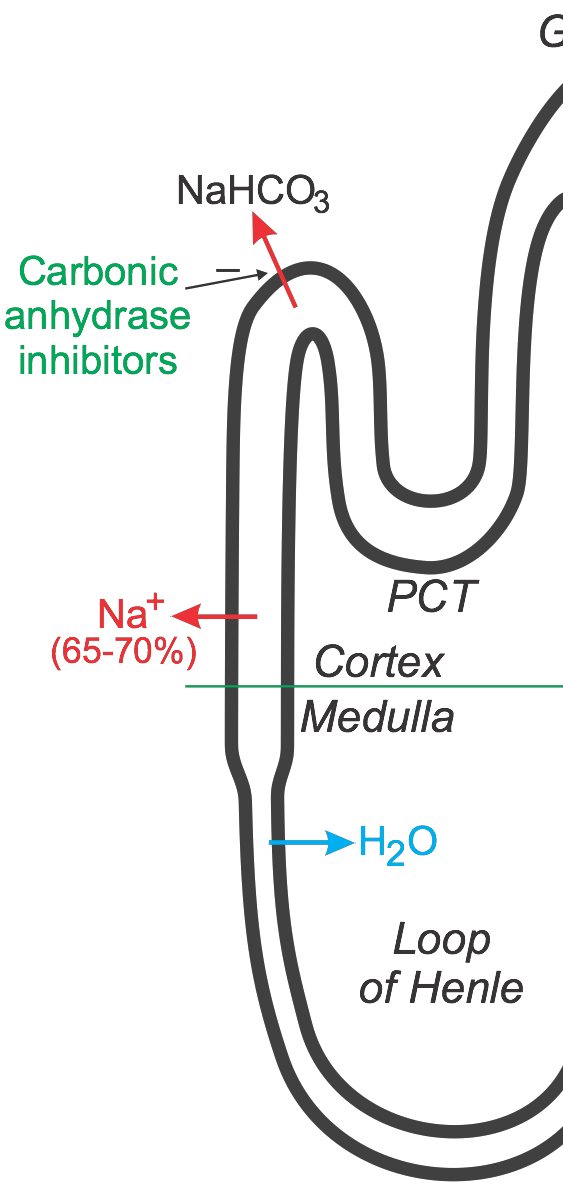
Discovery history
- sulfonamide(磺胺): alkaline diuresis & hyperchloremic
metabolic acidosis
- Mechanism: ↑ NaHCO3 in urine
Major clinical indications
- glaucoma(青光眼): no systematic side effects
- urinary alkalinization(尿碱化): ↑excretion of weak acids
- acute mountain sickness(极性高原病)
Drugs available: Acetazolamide(乙酰脞胺)
2. loop diuretic (2)
Furosemide (呋喃苯胺酸)
Mechanism: ↓ NKCC2(sodium-(potassium)-chloride cotransporter 2 ),
- then↓ NaCl reabsortion at think ascending limb
Specified clinical indications (2)
- hyperkalemia (toxicity: hypokelemia)
- acute renal failure
- anion overdose
Thiazides (3)
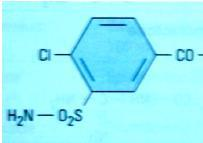
Identified during synthesize more carbonic anhydrase inhibitors
Chemistry
- Share an unsubstituted sulfonamide group
Mechanism: ↓ NaCl reabsorption by ↓Na+/Cl‐ transporter
Major clinical indications: a frequently used subgroup
Drugs available:
- table 15-5: thiazide & sulfonamide
Potassium-sparing diuretics (4)
Chemistry
- Spironolactone, aldosterone antagonist;
- Eplerennone is a spironolactone analog but with higher selectivity
- Amiloride & triameterene: inhibitor of Na+ influx
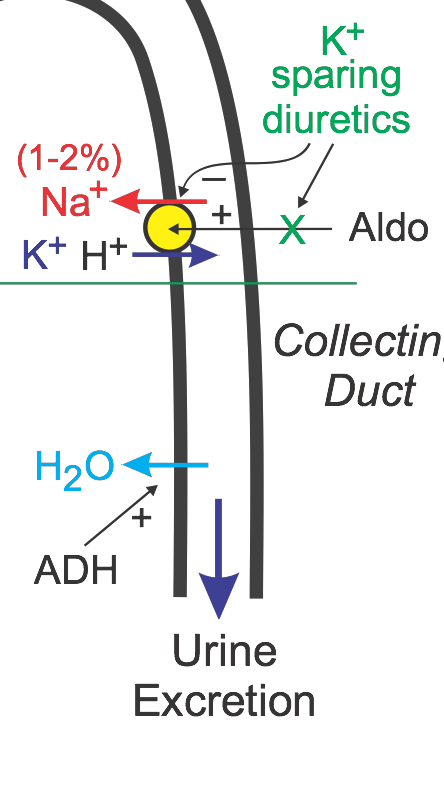
Applications:
- Primary or secondary hyperaldosteronism;
- Combined used with other diuretics
Agents altering water excretion (5a)
Osmotic diuretics: mannitol(甘露醇)
- Be filtered by the glomerulus, but not reabsorbed
Applications:
- ↑urine volume
- ↓intracranial & intraocular pressure
Antidiuretic hormone agonists
- Vasopressin and desmopressin: for central diabetes, insipidus(尿崩症)
Antidiuretic hormone antagonists
- Conivaptan, lithium, demeclocycline
- For primary or secondary ADH(抗利尿激素) elevation
3. Clinical pharmacology of Diuretic agents
Common reason:↓peripheral or pulmonary edema
- Hear failure: for pts CO maintained with high filling pressure
- Kidney disease: loop diuretics are often the best (furosemide)
- Hepatic cirrhosis: hypoalbuminemia, high aldosterone
- loop diuretics + aldosterone antagonist
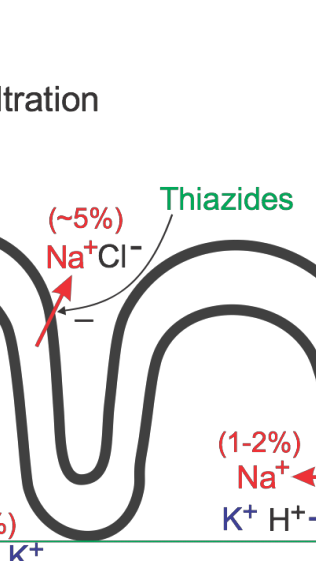
Major sites of antihypertensive drugs
Compensatory response to vasodilators
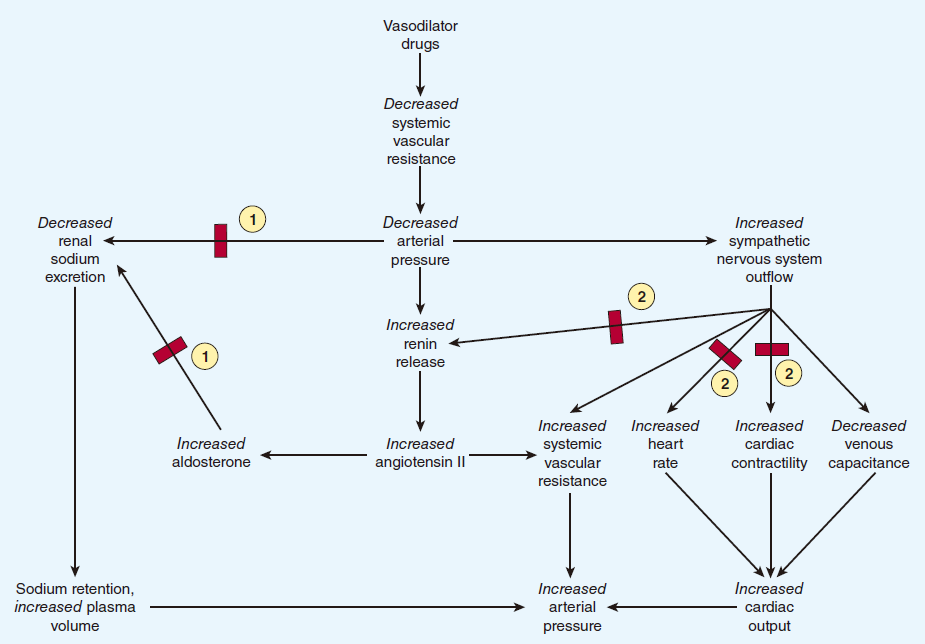
Due to compensation, combination therapy with beta-Blocker and diutretics are desired
- Combination treatment means another class of blood pressure medication is added to the first drug to increase effectiveness.
- Combination treatment for hypertension is individualized. It gives the best possible control of blood pressure with the fewest side effects.
- When used in a drug combination, the diuretic has fewer side effects. It also boosts the blood-pressure-lowering effect of the other medication.
- Sometimes, a beta-blocker is combined with an alpha-blocker. This may be useful for men who have hypertension and an enlarged prostate. The alpha-blocker may help both problems at the same time.
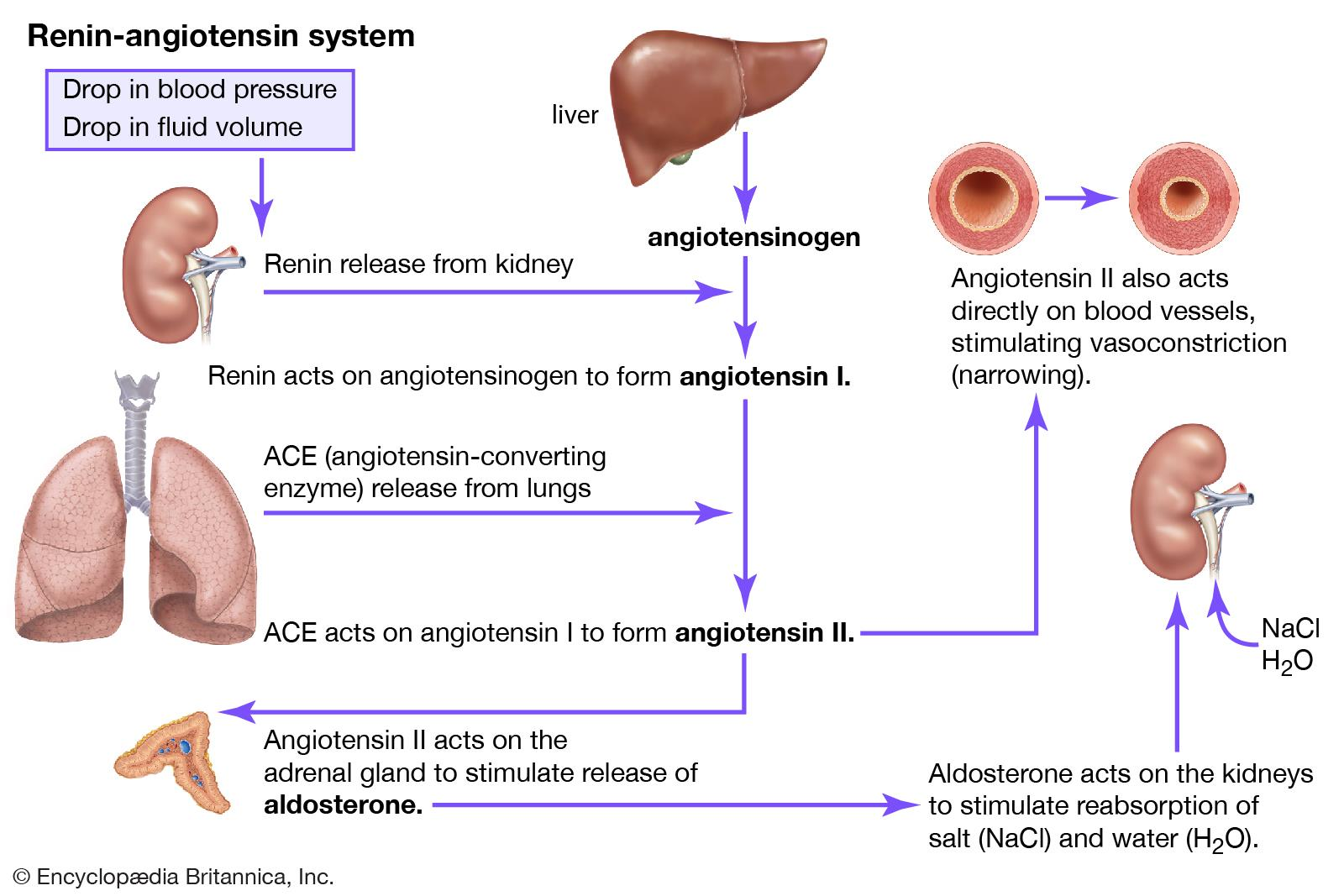
1. Site of action for Inhibitors of angiotensin
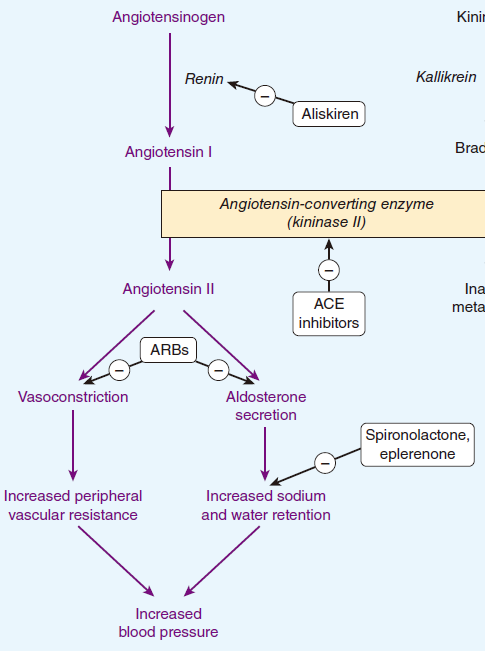
2. Inhibitors of angiotensin
Two major types:
ACEI: Captopril, …..pril
- ↓Angiotensin II, aldosterone
- More effective in Angiotensin I augumented heart damage
Ang II receptor blockers: Losartan, …..sartan
- blocking AT1 receptor
- the baroreceptor: to prevent the hypotension
When to start medication
- Diagnosis of essential HTN: excluding secondary HTN
- Initial step: non‐pharmacologic
- Sodium restriction
- Weight reduction
- Low saturated fat and total fat
- Physical exercise
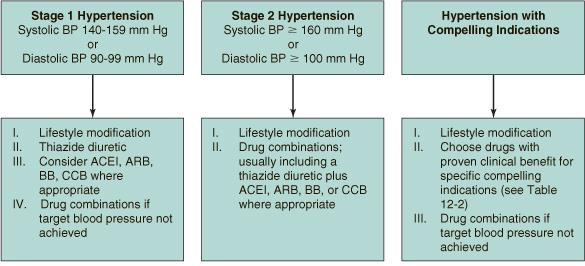
How to treat HTN
- 1 drug first, most of the pts requires 2 or more drugs
- Concomitant disease
- Chronic kidney disease: ACEI
- Angina: beta blocker, CCB
- Heart failure: diuretics, beta blocker, ACEI, AT1 blocker