L26 Cancer cell biology
一、Cancer as a microevolutionary process
Two types of evolution
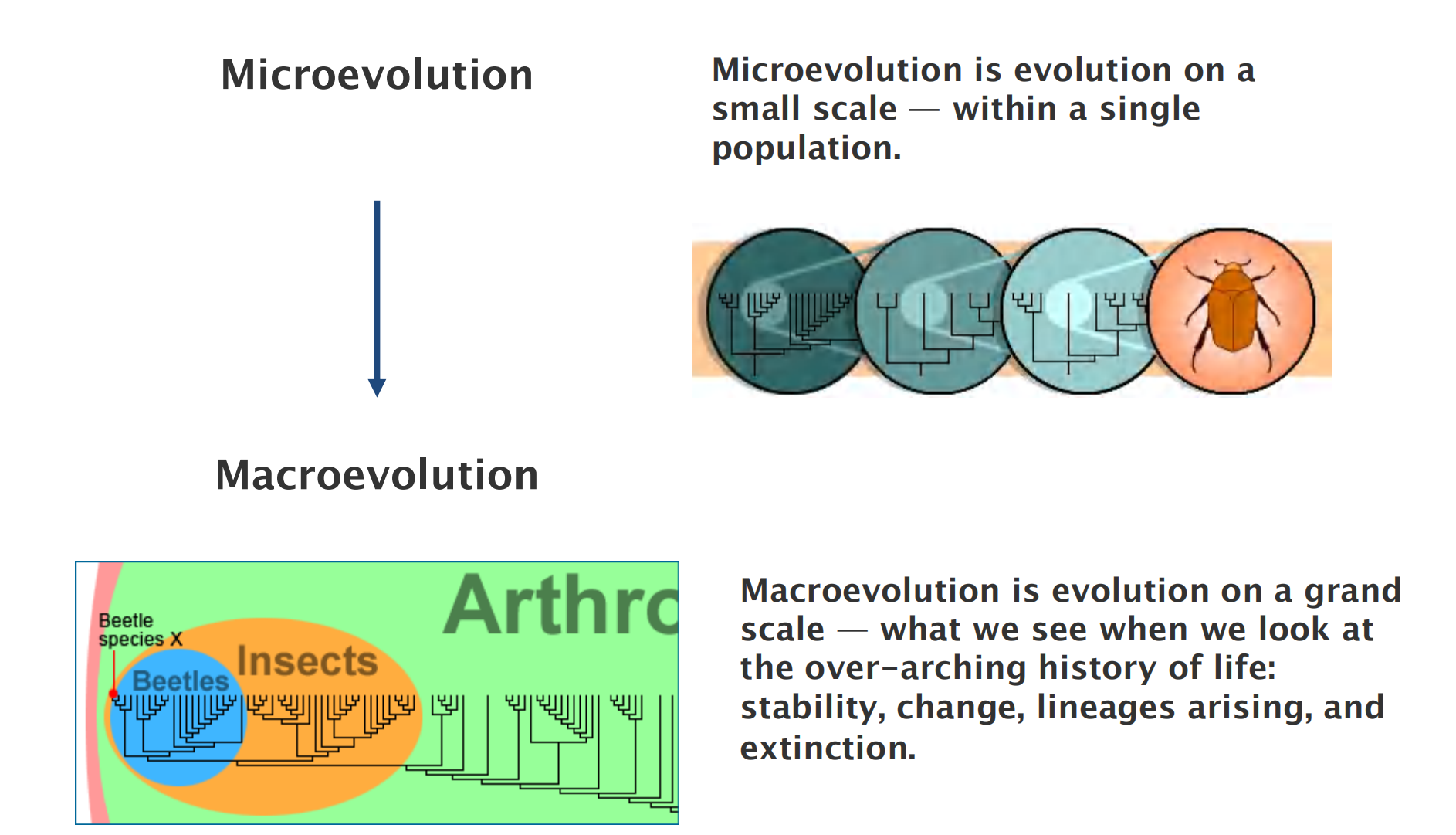
Microevolution
- Microevolution is evolution on a small scale — within a single population.
Macroevolution
- Macroevolution is evolution on a grand scale — what we see when we look at the over-arching history of life: stability, change, lineages arising, and extinction.
microevolutionary
1. Definition
Why is cancer called cancer?
- The Greek physician Hippocrates (460-370 BC), the “Father of Medicine” used the terms carcinos and carcinoma, which n Greek means a crab, to describe non-ulcer forming and ulcer-forming tumors.
- It was named after the crab because the finger-like spreading projections from a cancer called to mind the shape of a crab.
- Later, Roman physician, Celsus (28-50 BC) translated the Greek term into cancer, the Latin word for crab.
- It was Galen (130-200 AD), another Roman physician, who used the term oncos (Greek for swelling) to describe tumors.
- Oncos is the root word for oncology or study of cancers
What is cancer?
- The term cancer specifically refers to a new growth, that
- has the ability to invade surrounding tissues
- might metastasize (spread to distant other organs)
- eventually may lead to death (if untreated)
What is a tumor?
- “Tumor” is a commonly used, but non-specific, term for neoplasm, the abnormal new growth of cells.
- The word “tumor” simply refers to a mass.
- This is a general term that can refer to benign (generally harmless) or malignant (cancerous) growths.
The nature of cancer
Cancer: it is a disease in which an individual mutant clone of cells begins by prospering at the expense of its neighbors
An abnormal cell that grows (increases in mass) and proliferates (divides) out of control will give rise to a tumor, or neoplasm—literally, a new growth.
- As long as the neoplastic cells have not yet become invasive, however, the tumor is said to be benign
- A tumor is considered a true cancer if it is malignant; that is, when its cells have acquired the ability to invade surrounding tissue.
Invasiveness is an essential characteristic of cancer cells. It allows them to break loose, enter blood or lymphatic vessels, and form secondary tumors called metastases at other sites in the body
Cancer Cells Bypass Normal Proliferation Controls and Colonize Other Tissues
Carcinomas(癌) are cancers arising from epithelial cells, and they are by far the most common cancers in humans.
Sarcomas(肉瘤,恶性毒瘤) arise from connective tissue or muscle cells.
- cancer cells can contain an unusually large amount of heterochromatin
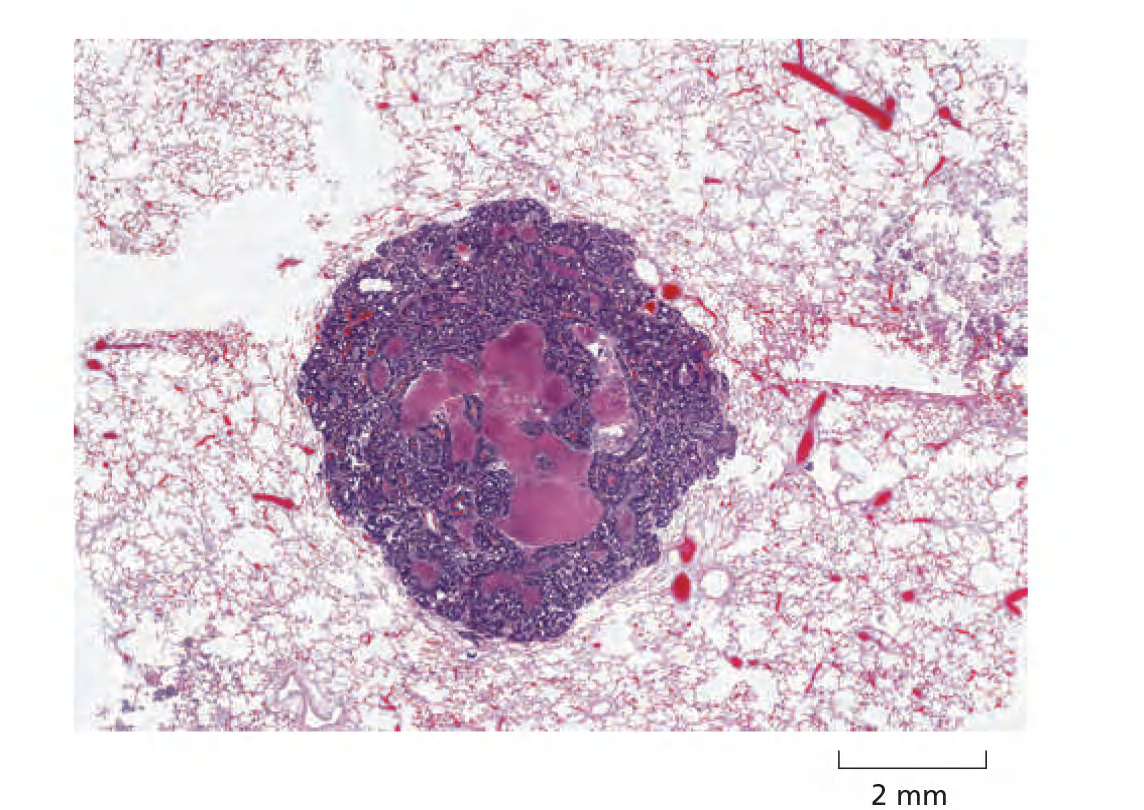
Cancer cells spread and grow and destroy the surrounding tissue → metastasis

Primary tumor versus metastasis
- Primary tumor is the initial tumor, the starting point of the cancer growth
- Metastasis is a new settlement of tumor forming cells, which are derived from another, primary tumor. Also referred to as secondary tumor
1. Morphological changes of cancerous cells
They are abnormal in their shape, their motility, their responses to growth factors in the culture medium, and, most characteristically, in the way they react to contact with the substratum and with one another
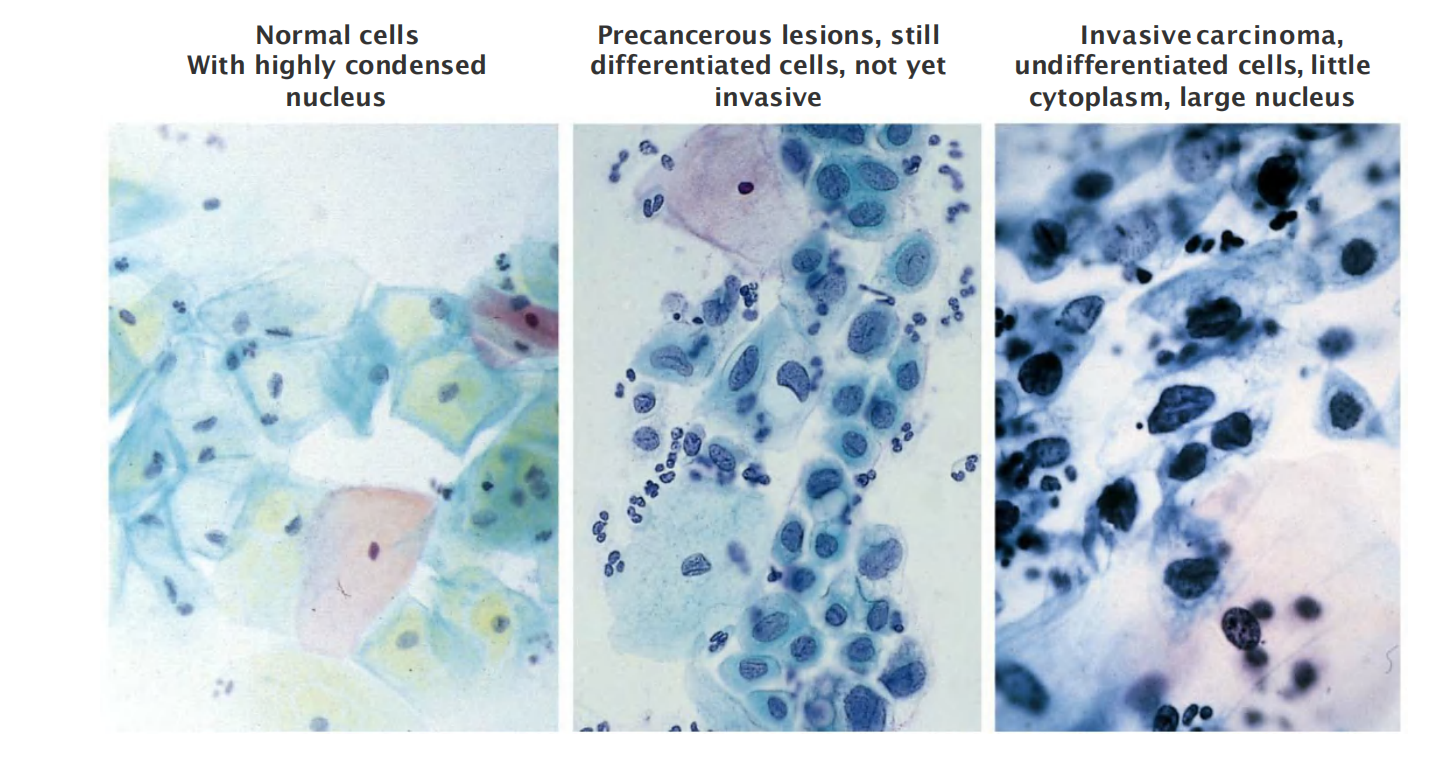
- 左图:Normal cells With highly condensed nucleus
- 中图:Precancerous lesions, still differentiated cells, not yet invasive
- 右图:Invasive carcinoma, undifferentiated cells, little cytoplasm, large nucleus
2. Monoclonal origin/clonal descendance of cancer
How to proof monoclonal origin of cancer?
- Molecular analysis of chromosomes reveals the clonal descendance(克隆血统) of the cancer cells.
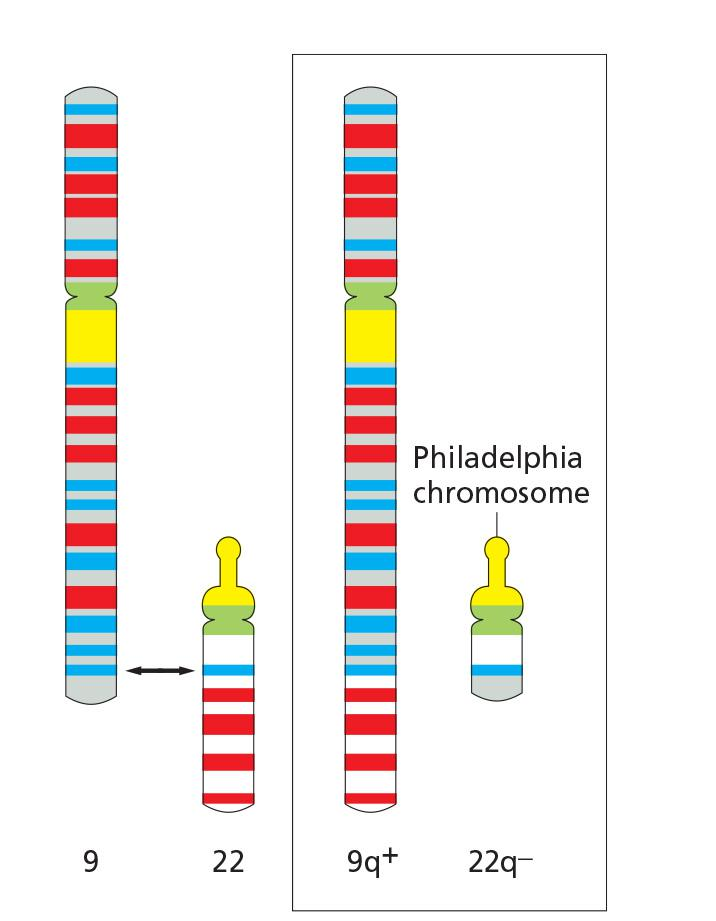
- Example: Chronic myelogenous leukemia (CML,慢性粒细胞性白血病)
- In CML, all cancer cells have generally the same translocation of the chromosome between the long arms of chromosomes 9 & 22 (Philadelphia chromosome)
- However, the break & rejoin differs a few 100-100 bases between patients, indicating an individual event in each case
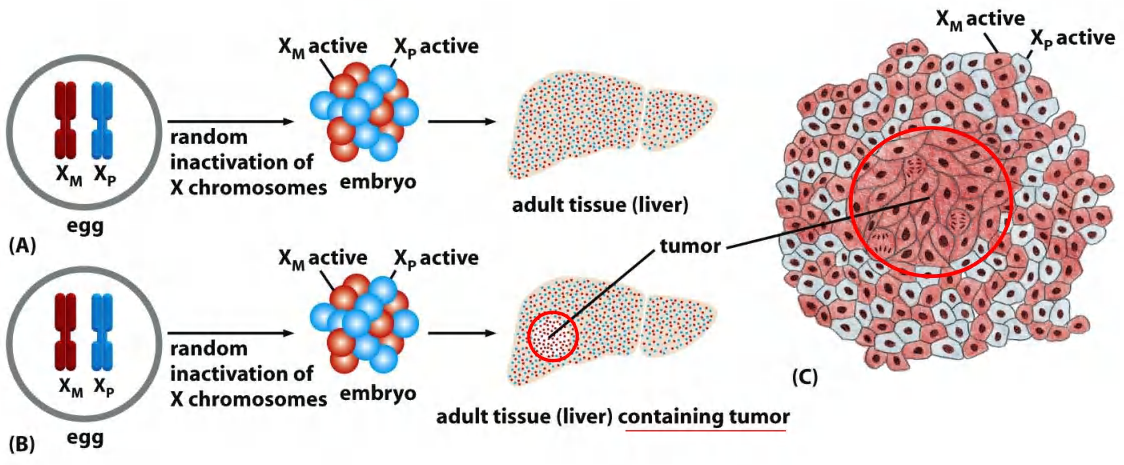
- Proof of monoclonal origin of cancer by X-inactivation mosaic analyses within tumor tissue
3. Cancer develops gradually from increasing aberrant cells
Darwinian evolution and clonal succession
- A single mutation is not enough to change a normal cell into a cancer cell
- Initiation of cancer is usually driven by multiple mutations
- Development of a tumor by repeated rounds of mutations
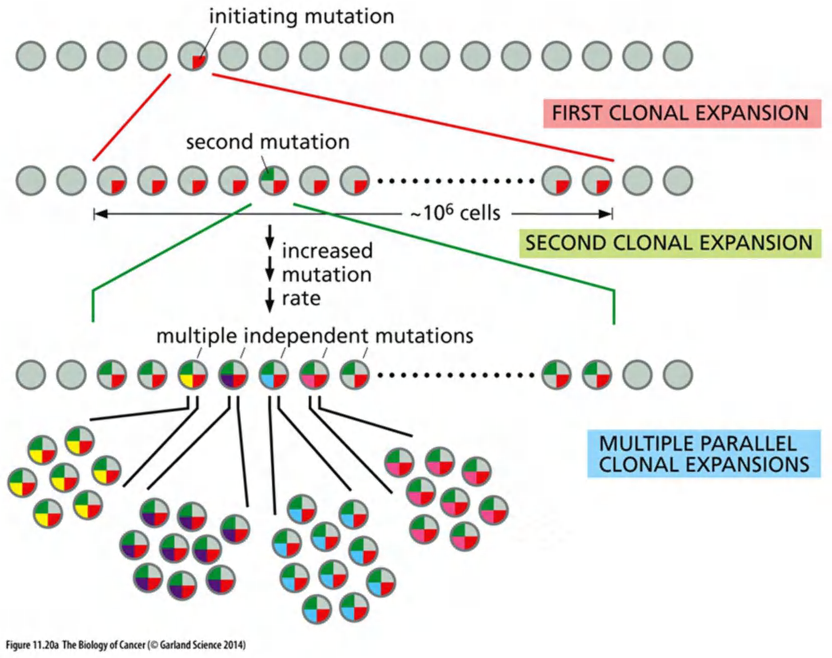
1. Clonal evolution
Development of a tumor by repeated rounds of mutations:
- each mutation either enhances cell proliferation or decreases cell death
- the progeny(后代) of such cells become the dominant clone in the tumor
- each step enhances the chance to proceed to the next step by increasing the numbers of cells that are at risk
- the final step: Invasion through the basement membrane - the initial step in metastasis
In reality, there are more than the three steps shown here, and a combination of genetic and epigenetic changes are involved
Epigenetic changes provide another important way to permanently inactivate a tumor suppressor gene
Most commonly, the gene may become packaged into heterochromatin and/or the C nucleotides in CG sequences in its promoter may become methylated in a heritable manner
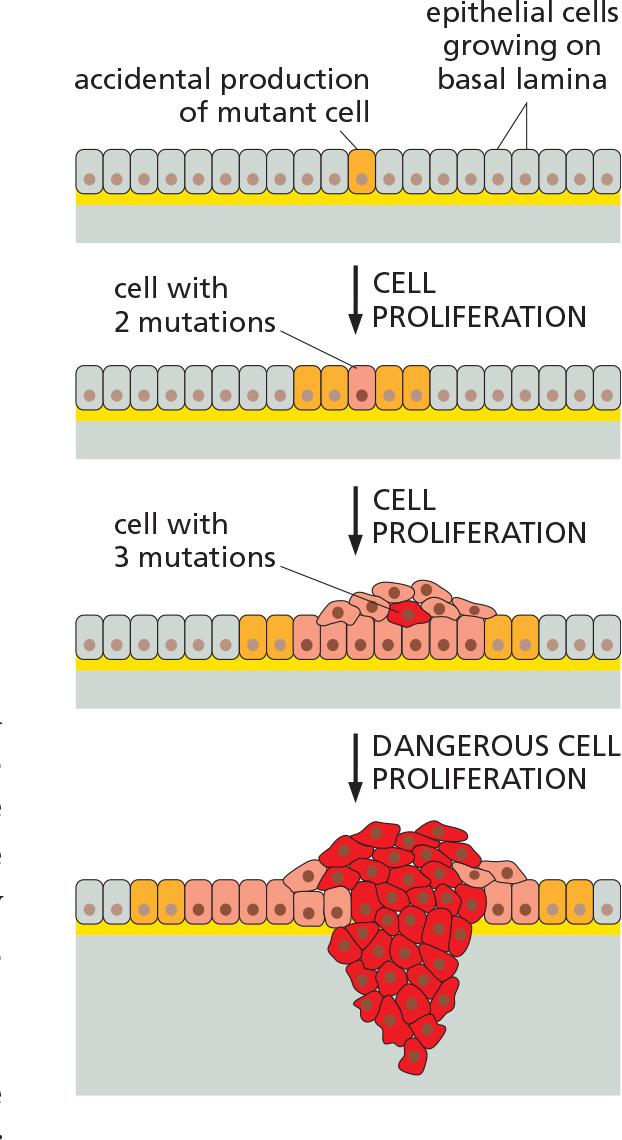
2. Cancers progress as a series of subclones
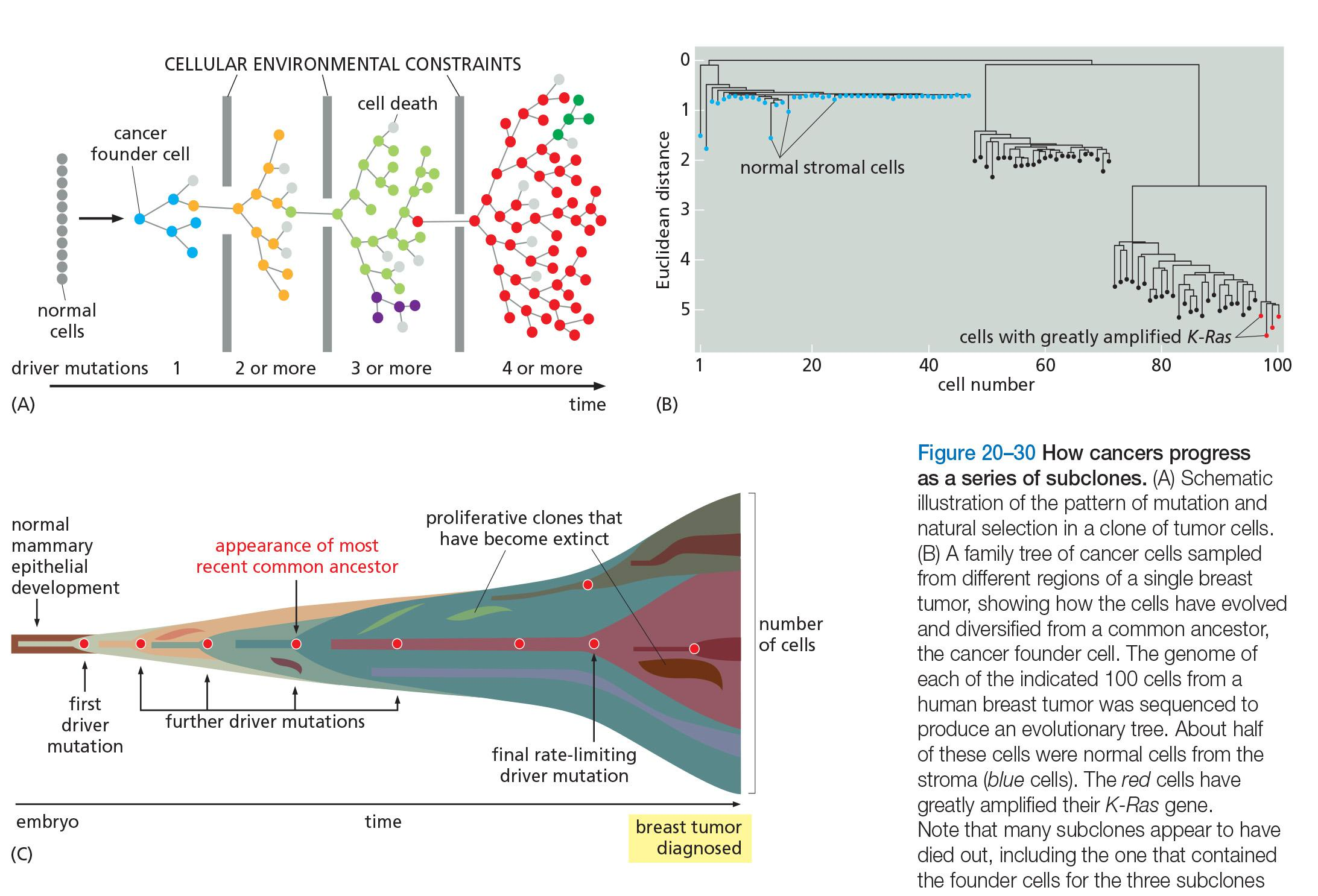
3. Genome instability of cancer cells
Human Cancer Cells Are Genetically Unstable
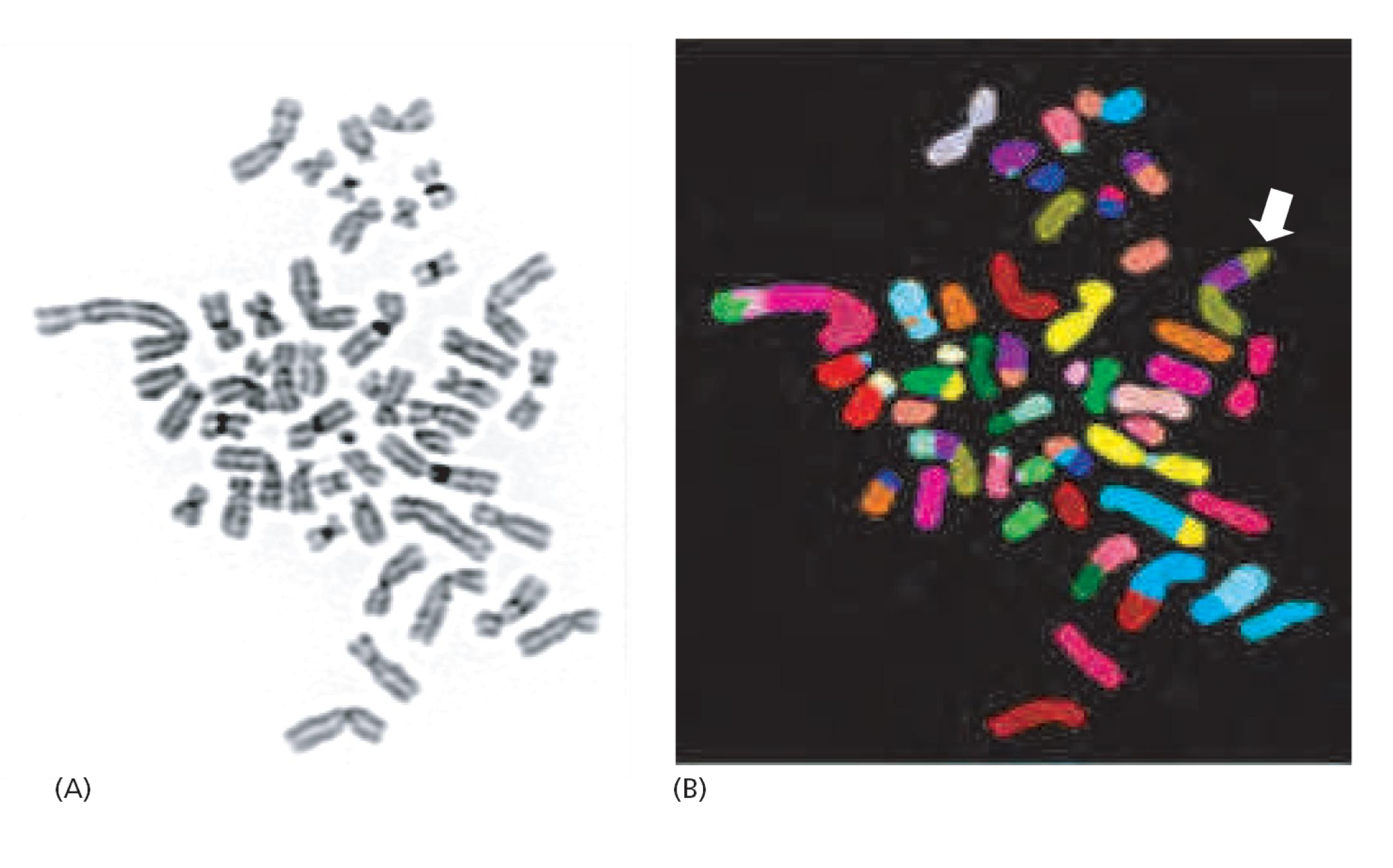
- Chromosomes from a tumor displaying abnormalities in structure & number: polyploidy(多倍性), aneuploidy(非整倍性), translocations(易位), etc.
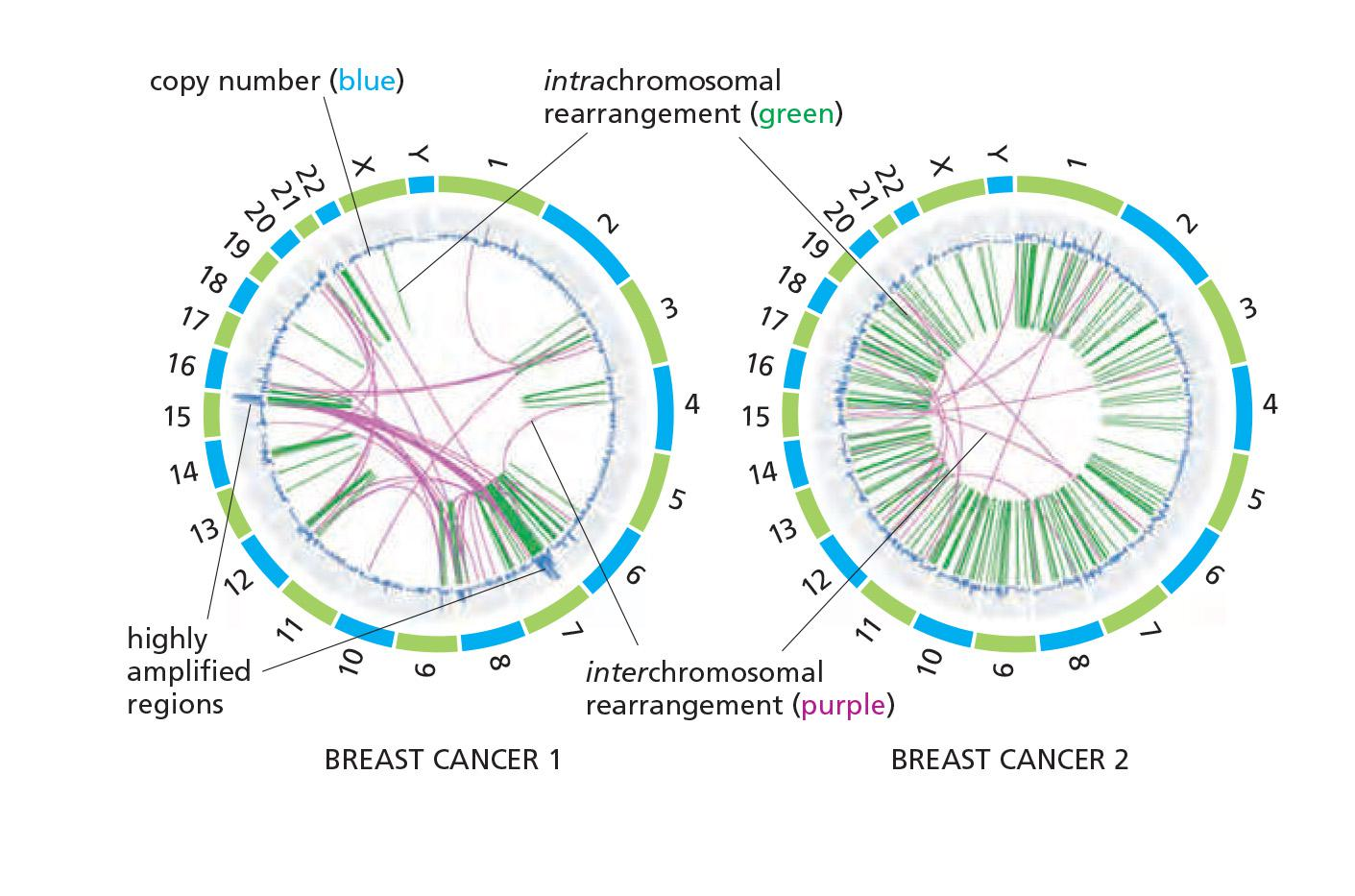
Extraordinarily disrupted genome of cancer cells
The karyotype—the set of chromosomes as they appear at mitosis
- Often, however, the karyotype is severely disordered, with many chromosome breaks and rearrangements.
- In some breast cancers, for example, genome sequencing reveals an astonishing scene of genetic chaos
The normal machinery for avoidance or repair of DNA double-strand breaks is evidently somehow defective
The cancer cells themselves were distinguished by their severely disrupted genomes.
Many Mutations in Tumor Cells are Merely Passengers
- Cancer cells generally contain many mutations in addition to gross chromosome abnormalities
Clearly, cancer cells are constantly mutating, multiplying, competing, evolving, and diversifying as they exploit new ecological niches and react to the treatments that are used against them
Cancer cells escape normal restrictions on proliferation potential
Cancer Cells Display an Altered Control of Growth
- they can evolve an alternate mechanism based on homologous recombination (called ALT,同源重组) for elongating their chromosome ends.
Cancer cells that can be grown in culture, or cultured cells artificially engineered to contain the types of mutations encountered in cancers, typically show a transformed phenotype
- They are abnormal in their shape, their motility, their responses to growth factors in the culture medium, and, most characteristically, in the way they react to contact with the substratum and with one another.
Human Cancer Cells Escape a Built-in Limit to Cell Proliferation
Many normal human cells have a built-in limit to the number of times they can divide when stimulated to proliferate in culture: they permanently stop dividing after a certain number of population doublings (25–50 for human fibroblasts, for example).
- This cell-division-counting mechanism is termed replicative cell senescence, and it generally depends on the progressive shortening of the telomeres at the ends of chromosomes, a process that eventually changes their structure
- the replication of telomere DNA during S phase depends on the enzyme telomerase, which maintains a special telomeric DNA sequence that promotes the formation of protein cap structures to protect chromosome ends.
- Because many proliferating human cells (stem cells being an exception) are deficient in telomerase, their telomeres shorten with every division, and their protective caps deteriorate(恶化, 变坏), creating a DNA damage signal
Human cancer cells avoid replicative cell senescence in one of two ways.
- They can maintain the activity of telomerase as they proliferate, so that their telomeres do not shorten or become uncapped, or they can evolve an alternate mechanism based on homologous recombination (called ALT) for elongating their chromosome ends.
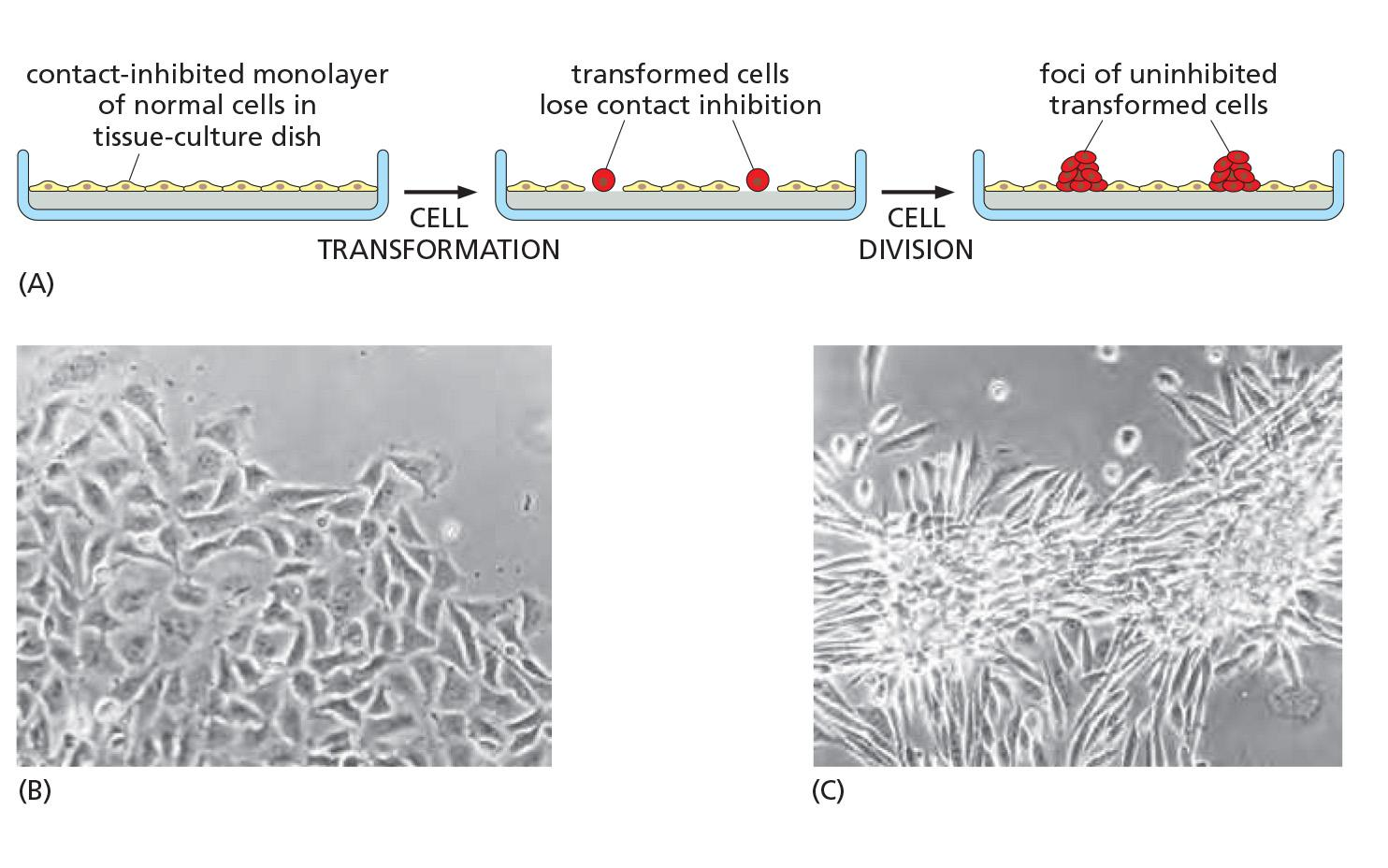
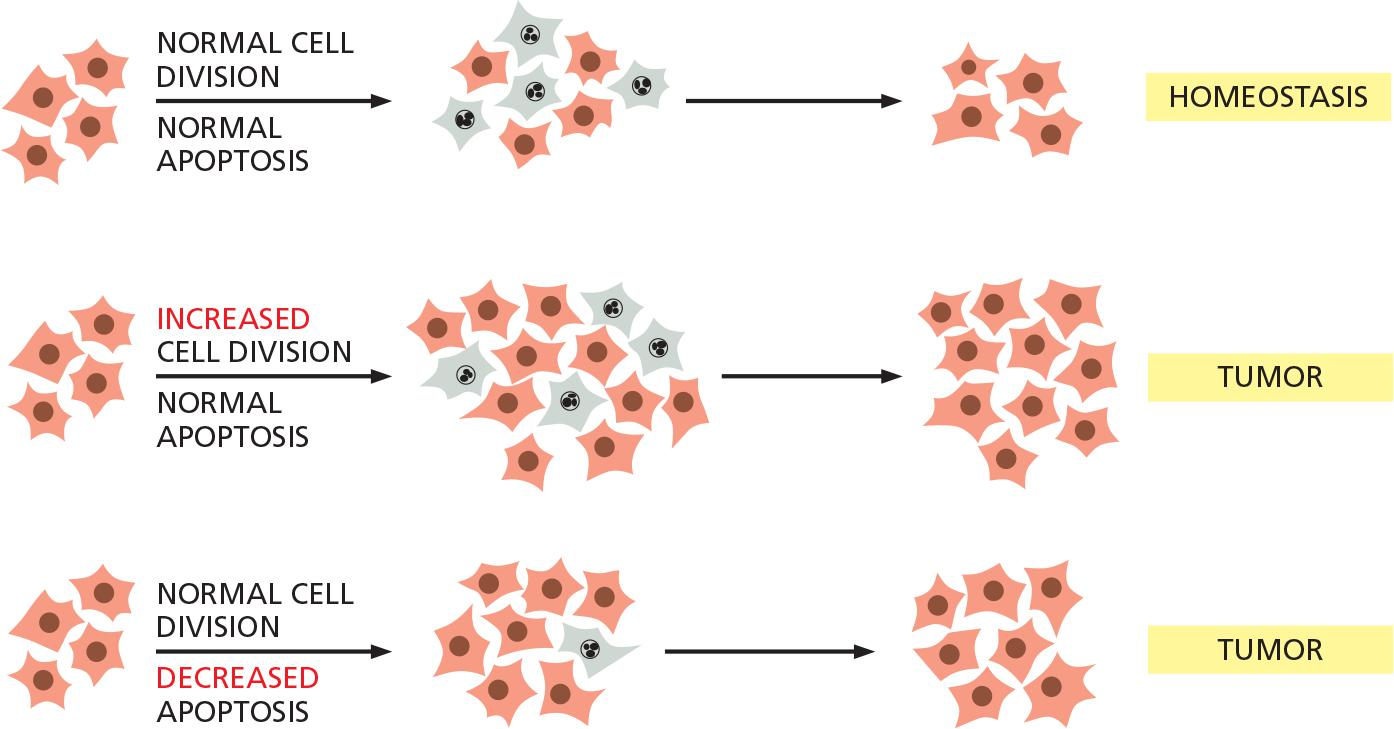
- Loss of contact-inhibition
- Increased cell divisions
- Decreased apoptosis
- Both together
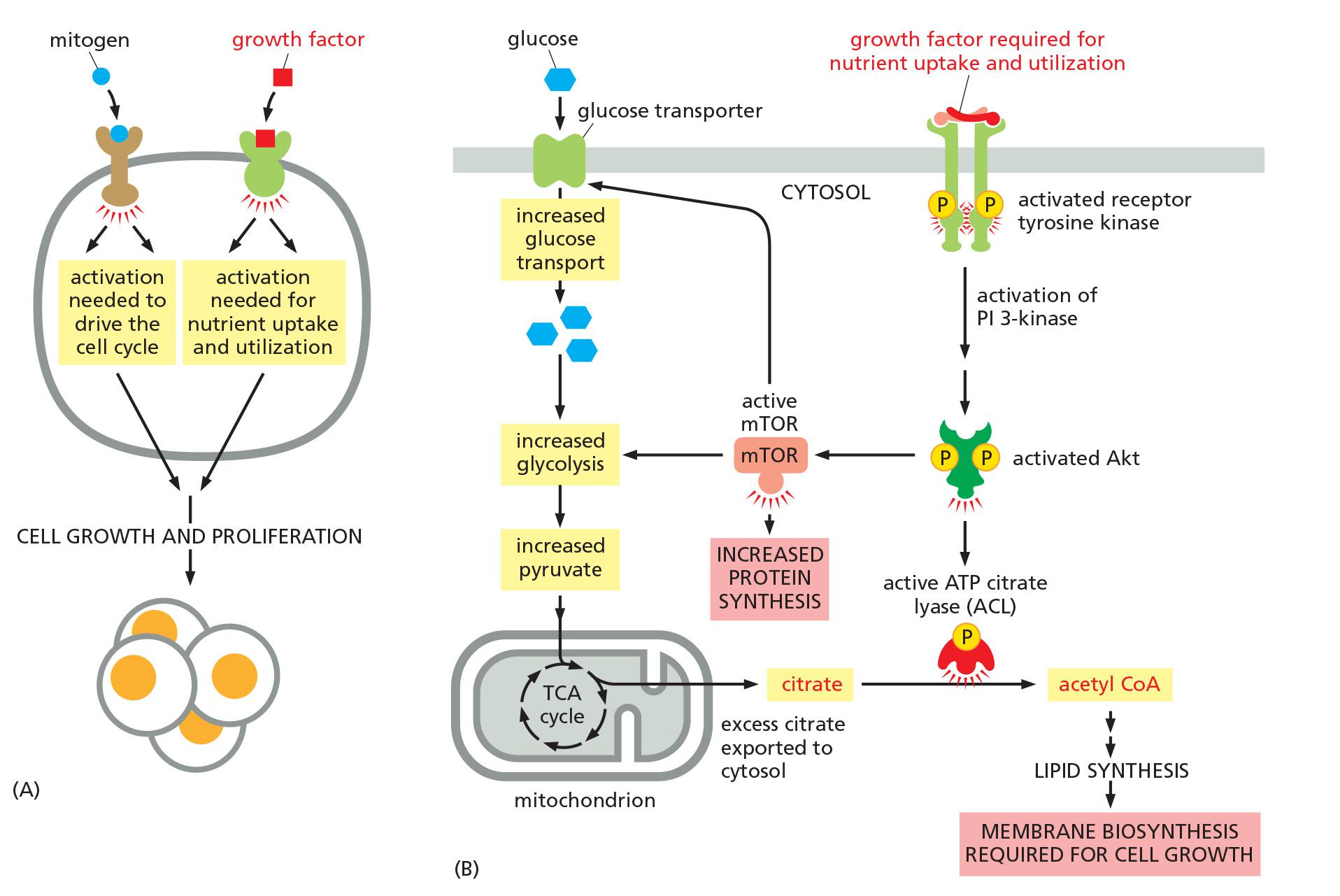
Cancer cells have an altered sugar metabolism
Cancer Cells Have an Altered Sugar Metabolism
most tumors have a metabolism more similar to that of a growing embryo than to that of normal adult tissue.
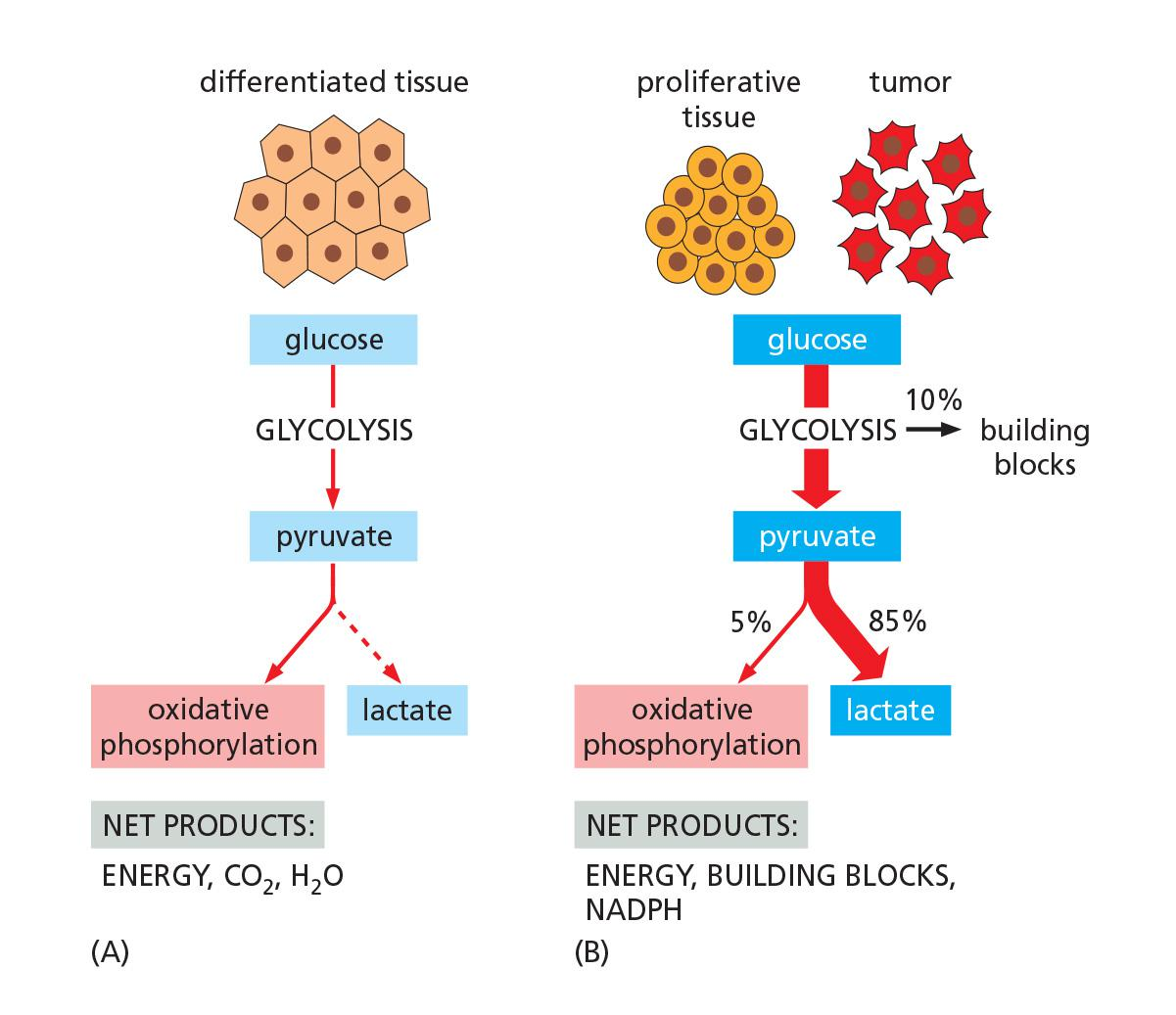
- Warburg effects
- increase glycolysis versus oxidative phosphorylation → tumor tends to ferment(发酵)
Cancer cells have abnormal responses to DNA damage and other stresses
Cancer Cells Have an Abnormal Ability to Survive Stress and DNA Damage
In fact, one of the most important properties of many types of cancer cells is that they fail to undergo apoptosis when a normal cell would do so
- DNA damage:
- p53 mutations, ATM mutations
- failure to arrest cell cycle or/and failure to cause apoptosis
- each resulting in producing more genetic mutations in each cell cycle
The tumor microenvironment plays a role in tumorigenesis
The Tumor Microenvironment Influences Cancer Development
The development of a tumor relies on a two-way communication between the tumor cells and the tumor stroma, just as the normal development of epithelial organs relies on communication between epithelial cells and mesenchymal cells (间充质细胞)
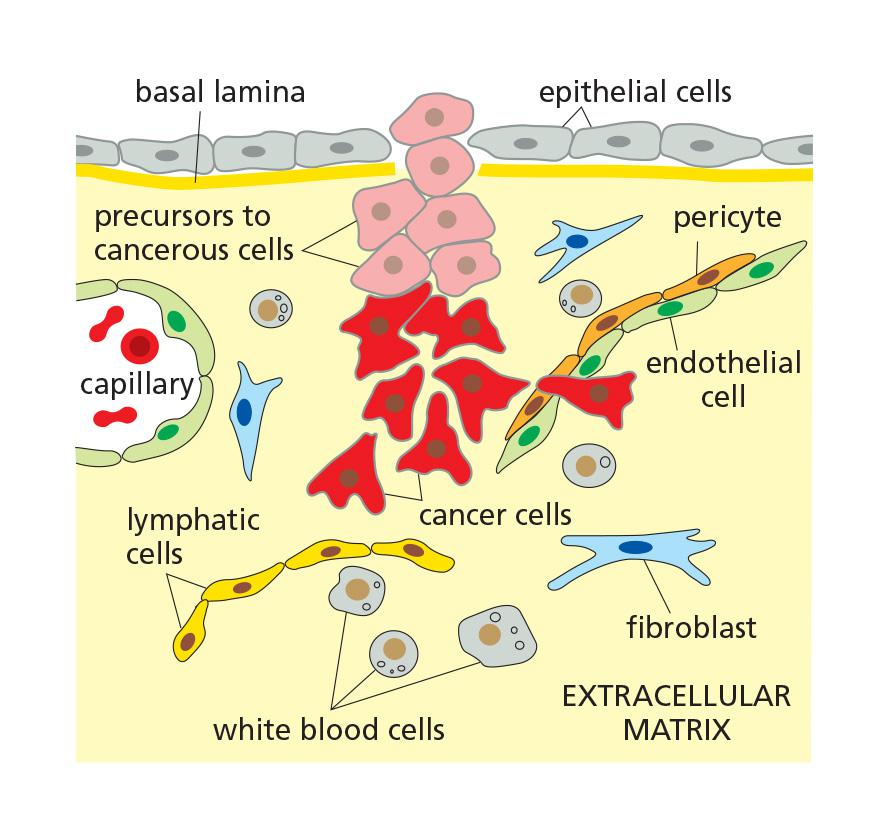
Cell microenvironment includes neighboring cells and ECM.
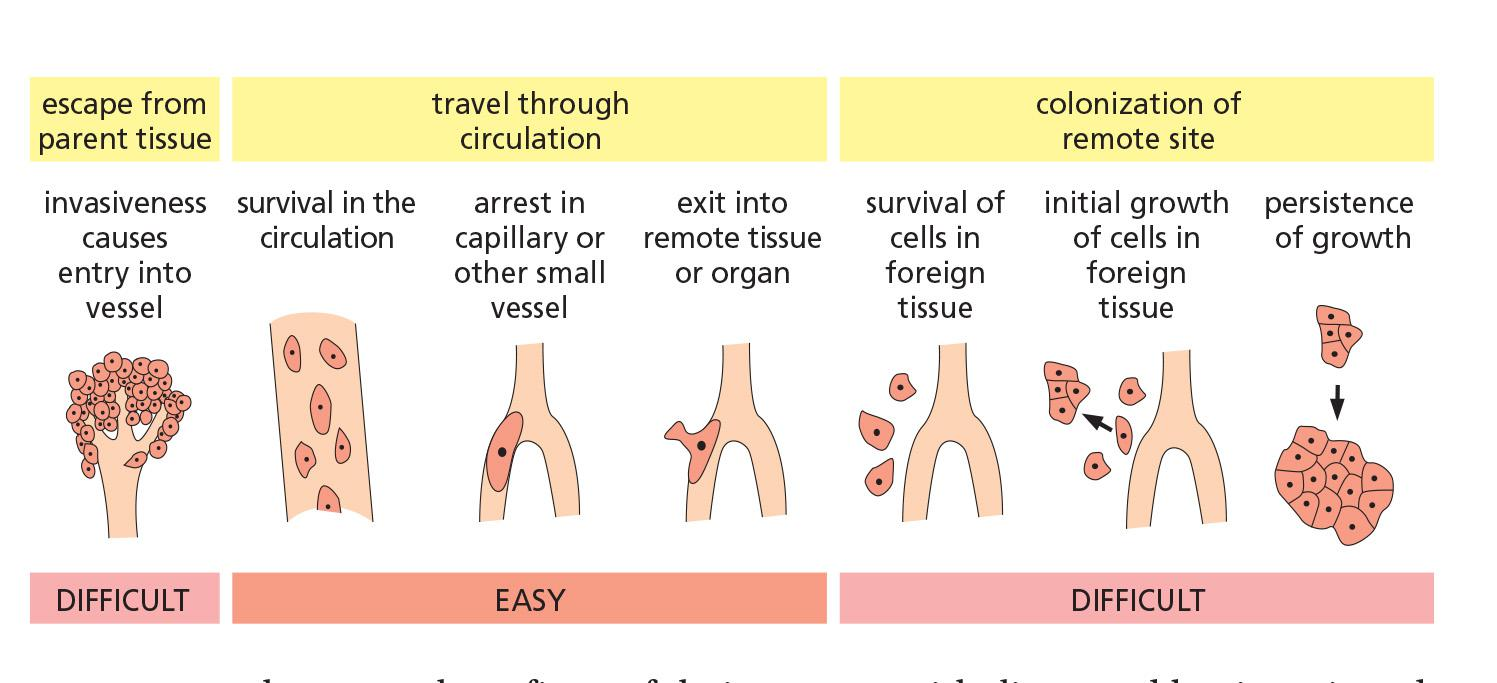
Metastasis
Cancer Cells Must Survive and Proliferate in a Foreign Environment
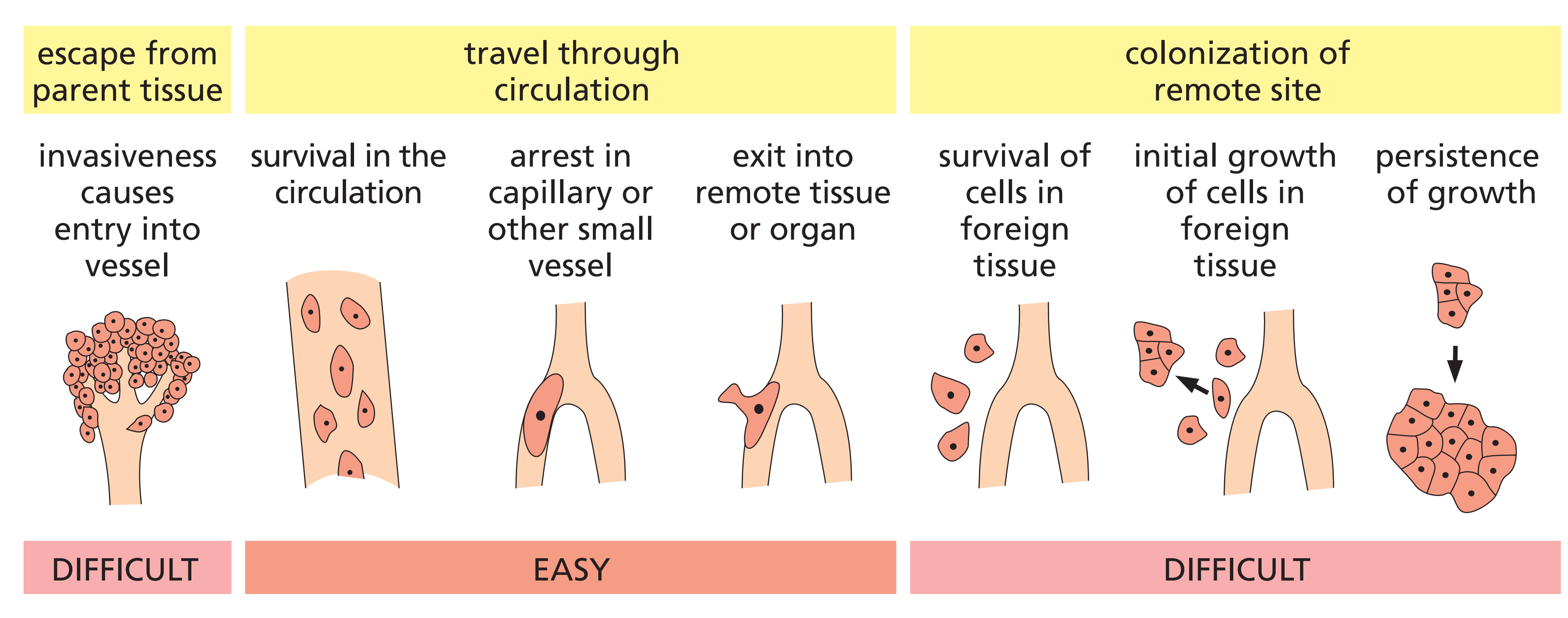
- First, the cells must escape the normal confines of their parent epithelium and begin to invade the tissue immediately beneath.
- Second, they must travel via the blood or lymph to lodge in distant sites.
- Third, they must survive there and multiply.
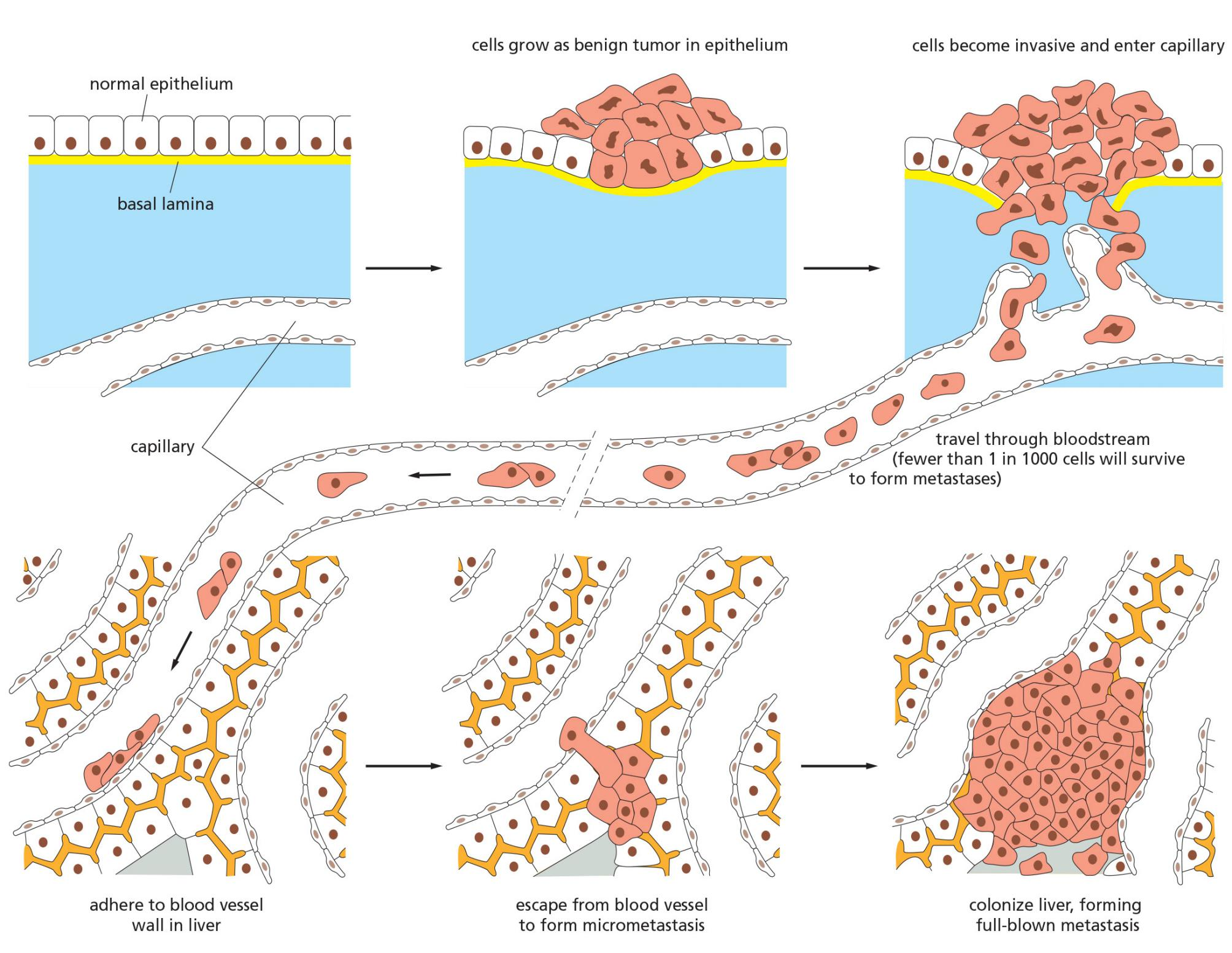
The first step, local invasiveness(局部侵袭性), requires a relaxation of the mechanisms that normally hold epithelial cells together.
- As mentioned earlier, this step resembles the normal developmental process known as the epithelial–mesenchymal transition (EMT,上皮-间质转化), in which epithelial cells undergo a shift in character, becoming less adhesive and more migratory(迁移的;有迁居习惯(或特色)的)
- A key part of the EMT process involves switching off expression of the E-cadherin genes
- The primary function of the transmembrane E-cadherin protein is in cell–cell adhesion, binding epithelial cells together through adherens junctions
- In some carcinomas of the stomach and of the breast, E-cadherin has been identified as a tumor suppressor gene, and a loss of E-cadherin may promote cancer development by facilitating local invasiveness.
The initial entry of tumor cells into the circulation is helped by the presence of a dense supply of blood vessels and sometimes lymphatic vessels, which tumors attract to themselves as they grow larger and become hypoxic(低氧) in their interior
- This process, called angiogenesis(血管再生术), is caused by the secretion of angiogenic factors that promote the growth of blood vessels, such as vascular endothelial growth factor (VEGF)
The remaining steps in metastasis, involving exit from a blood or lymphatic vessel and the effective colonization of remote sites
- To discover which of the later steps in metastasis present cancer cells with the greatest difficulties, one can label the cells with a fluorescent dye or green fluorescent protein (GFP), inject them into the bloodstream of a mouse, and then monitor their fate
Cancer cells must survive proliferate in a foreign environment
Metastasis is itself a multi-step process: the cancer cells first have to invade local tissues and vessels, move through the circulation, leave the vessels, and then establish new cellular colonies at distant sites
Invasiveness is thus one of the defining properties of malignant tumors
For carcinomas, this change resembles the epithelial–mesenchymal transition (EMT) that occurs in some epithelial tissues during normal development
1. High activity of angiogenesis (formation of blood vessels)
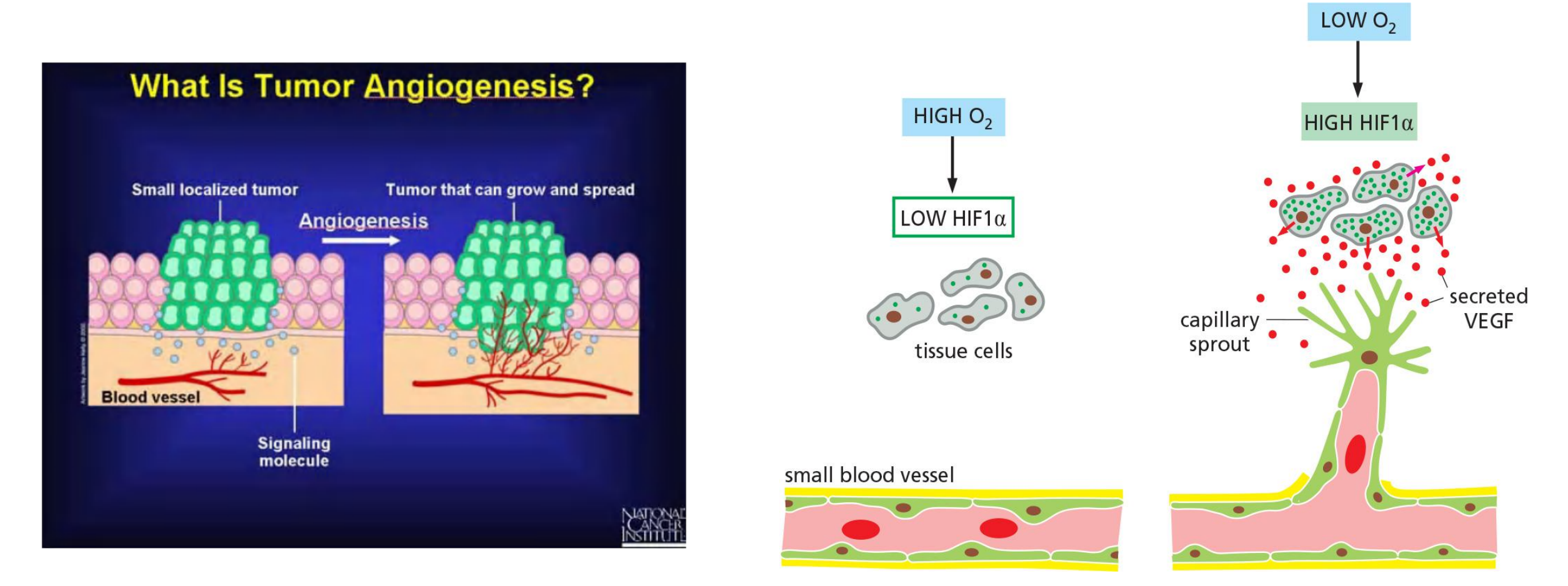
- Tumors induce the formation of new blood vessels to secure their own supply with oxygen and nutrients
- VEGF (vascular endothelial growth factor) protein
- HIF1 (hypoxia-inducible factor 1a) transcription factor for VEGF
二、Critical genes in cancer
a given cancer cell will also contain a large number of somatic mutations that are accidental by-products
cancer-critical genes, meaning all genes whose alteration contributes to the causation or evolution of cancer by driving tumorigenesis.
a gain-of-function mutation can drive a cell toward cancer, are called proto-oncogenes(原癌基因); their mutant, overactive or overexpressed forms are called oncogenes(致癌基因).
- Most cells expressing the oncogene, however, do not give rise to cancers
- multiple mutations are required for tumorigenesis
Genes of the second class, in which a loss-of-function mutation can contribute to cancer, are called tumor suppressor genes
- Those genes whose alteration results in genomic instability represent a subclass of cancer-critical genes that are sometimes called genome maintenance genes.
- The mutation of a single copy of a proto-oncogene that converts it to an oncogene has a dominant, growth-promoting effect on a cell
Some tumors contain distinct sectors, all clearly cancerous, but differing in appearance because they differ genetically
Genes Mutated in Cancer Can Be Made Overactive in Many Ways
- A small change in DNA sequence such as a point mutation or deletion(点突变或缺失) may produce a hyperactive protein when it occurs within a protein-coding sequence, or lead to protein overproduction when it occurs within a regulatory region for that gene.
- Gene amplification(基因扩增) events, such as those that can be caused by errors in DNA replication, may produce extra gene copies; this can lead to overproduction of the protein.
- A chromosomal rearrangement(染色体重排)— involving the breakage and rejoining of the DNA helix—may either change the protein-coding region, resulting in a hyperactive fusion protein, or alter the control regions for a gene so that a normal protein is overproduced.
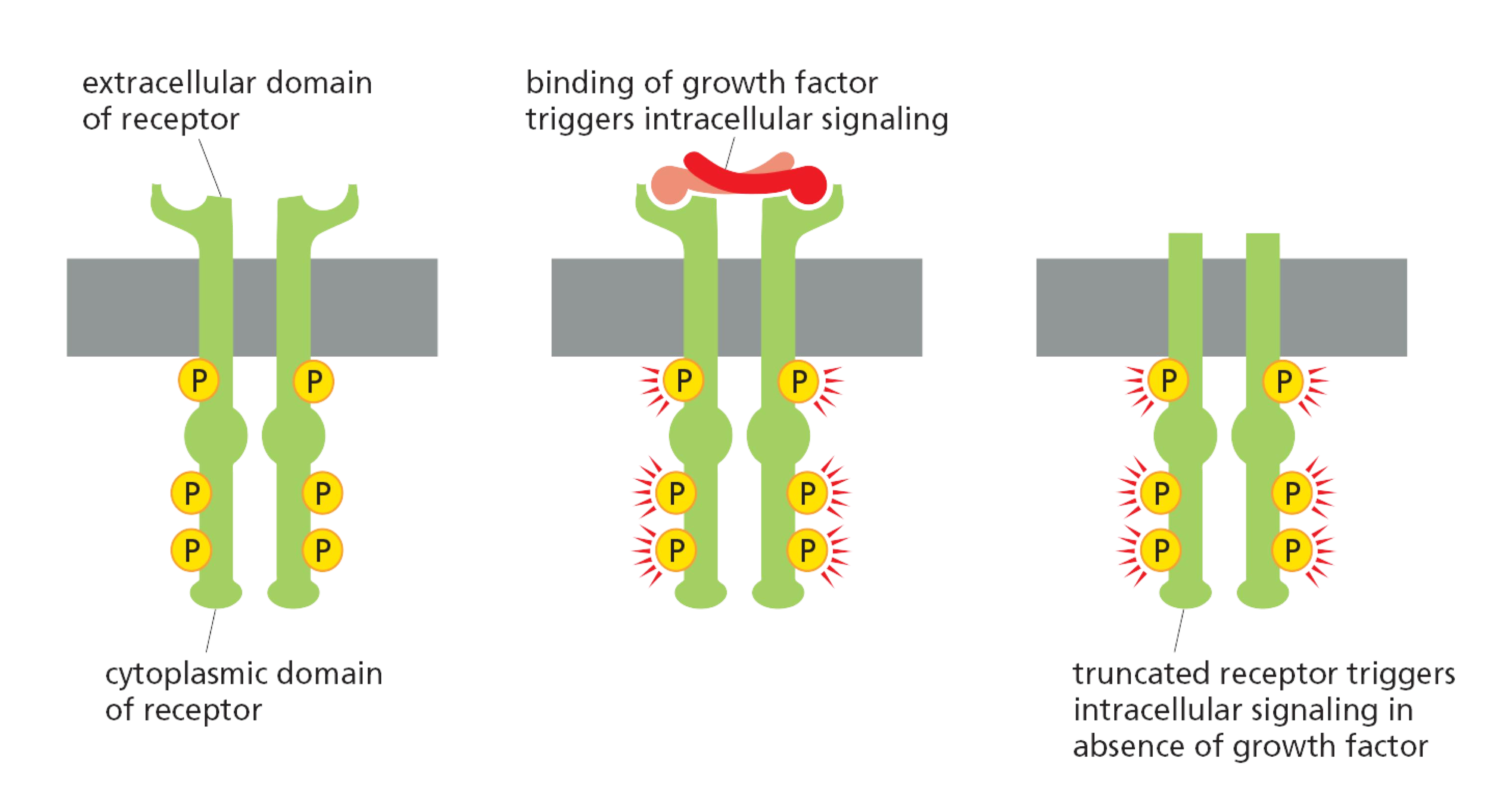
As one example, the receptor for the extracellular signal protein epidermal growth factor (EGF) can be activated by a deletion that removes part of its extracellular domain, causing it to be active even in the absence of EGFs
- It thus produces an inappropriate stimulatory signal, like a faulty doorbell that rings even when nobody is pressing the button. Mutations of this type are frequently found in the most common type of human brain tumor, called glioblastoma(成胶质细胞瘤;恶性胶质瘤;胶质母细胞瘤)
Discovery of genes which are critical to cancer formation
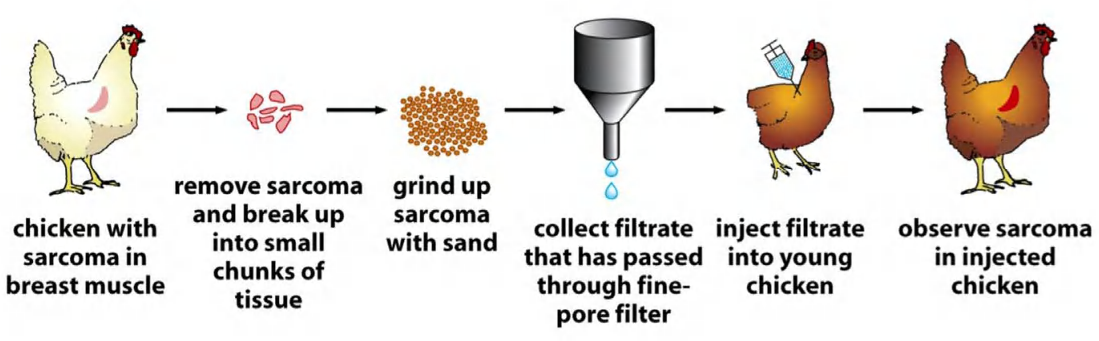
- Discovery of sarcoma (Src) genes
- The egg or the chicken? This time, it started with the chicken
- Dr. Peyton Rous: Sarcoma induction in chicken by a cell-free tumor filtrate (→ discovery of the Rous sarcoma virus, RSV)
- Later, Rous discovered that sarcoma virus DNA can induce sarcoma formation
Cellular origin of retroviral oncogenes
- Proto-oncogenes
Retroviruses Can Act as Vectors for Oncogenes That Alter Cell Behavior
an infectious agent that causes connective-tissue tumors, or sarcomas, was characterized as a virus—the Rous sarcoma virus.
- Like all the other RNA tumor viruses discovered since, it is a retrovirus. When it infects a cell, its RNA genome is copied into DNA by reverse transcription, and the DNA is inserted into the host genome, where it can persist and be inherited by subsequent generations of cells.
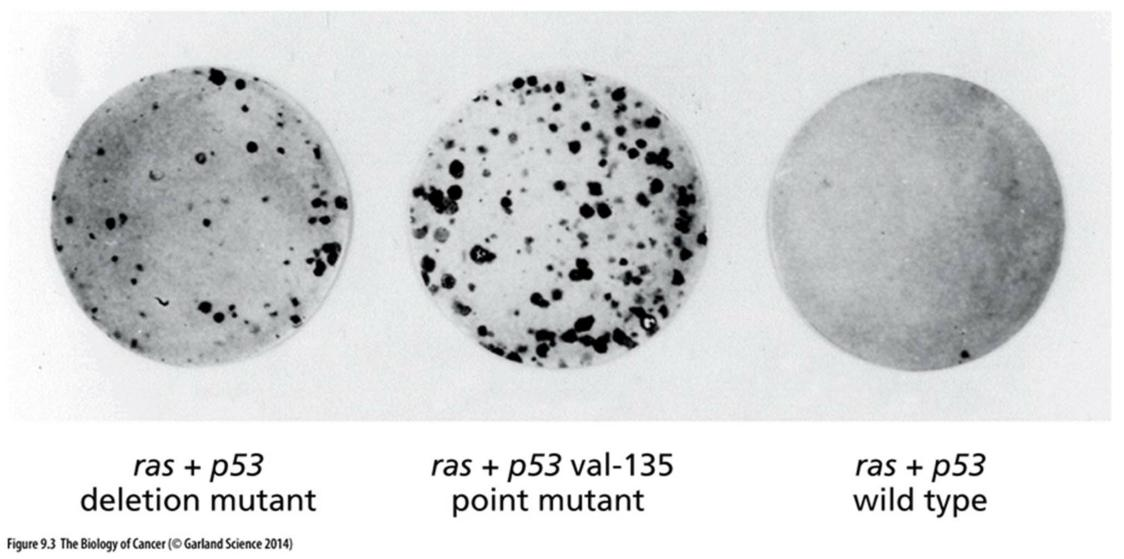
1. Discovery of tumor suppressor
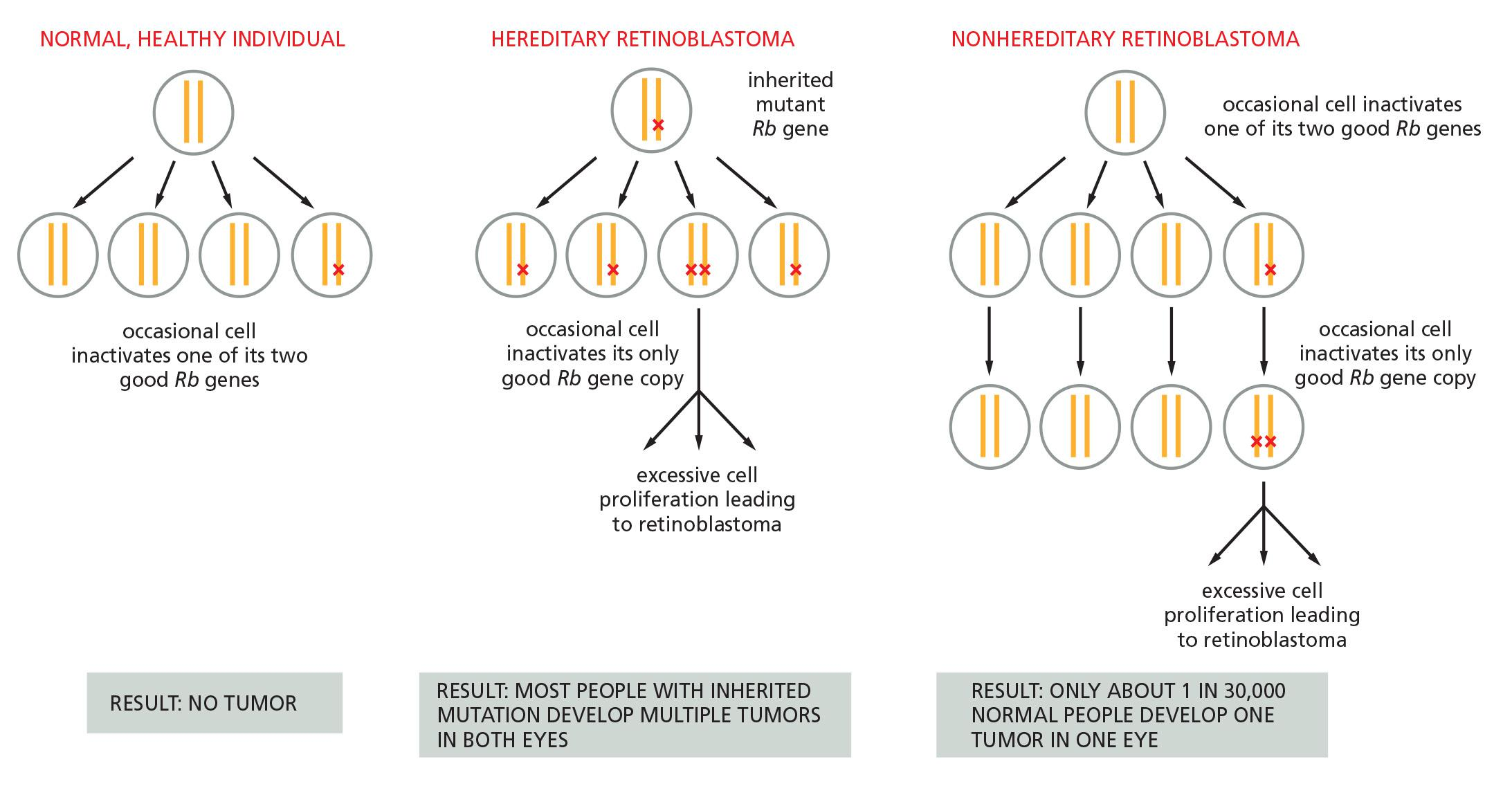
- Studies of rare hereditary cancer syndromes first identified tumor suppressor genes
- Rb (retinoblastoma) gene identification: infected individual has a deletion of a certain band in his chromosome 13.
- Both copies of the Rb gene need to be defective to confer cancer phenotype.
2. Alteration of “cancer-critical genes” influence cancer development
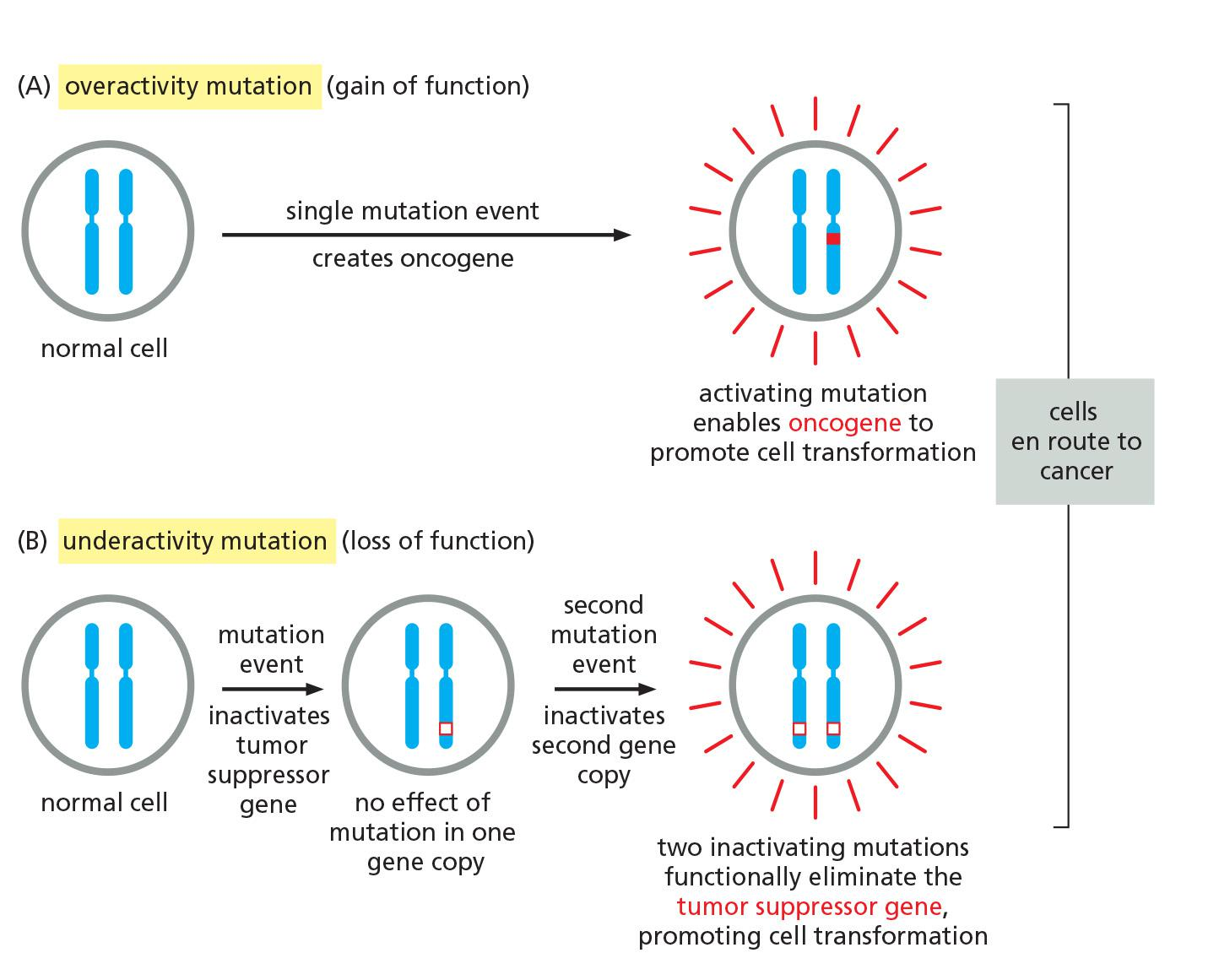
Two broad categories
- Proto-oncogenes vs. tumor suppressors
- Oncogene: Genes which mutational activation of proteins that normally Promote cell proliferation
- Tumor suppressor: Genes which Mutational inactivation of proteins that normally inhibit cell proliferation
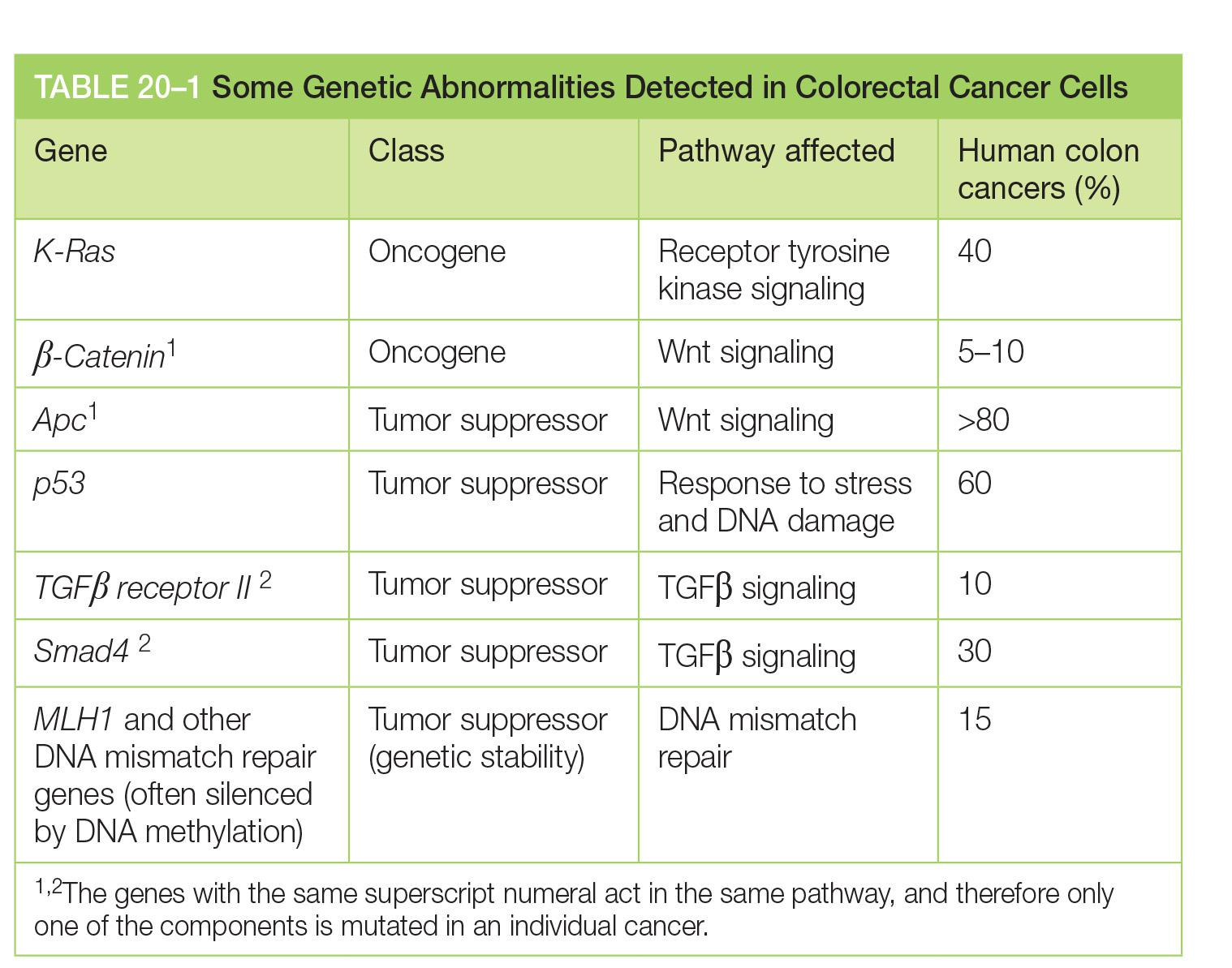
Cancer-critical genes in human genome
- 1 % of the genes in the human genome are cancer-critical genes
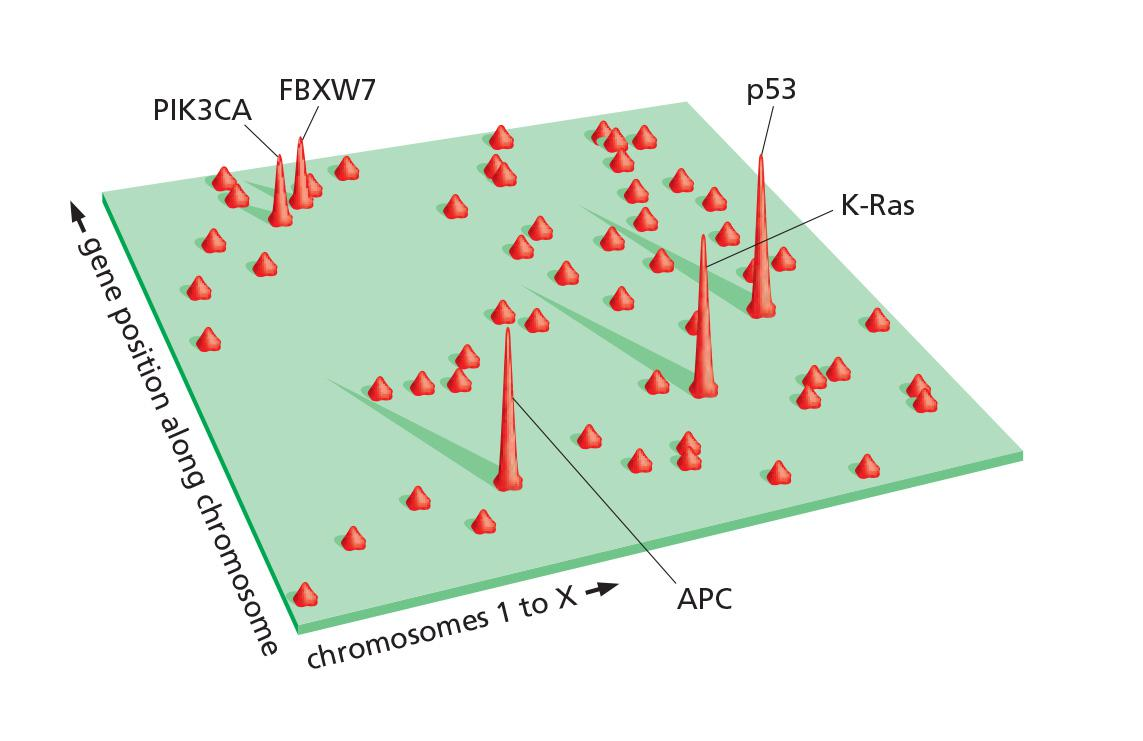
- The mutation landscape in colorectal cancer
- These cancer-critical genes are amazingly diverse
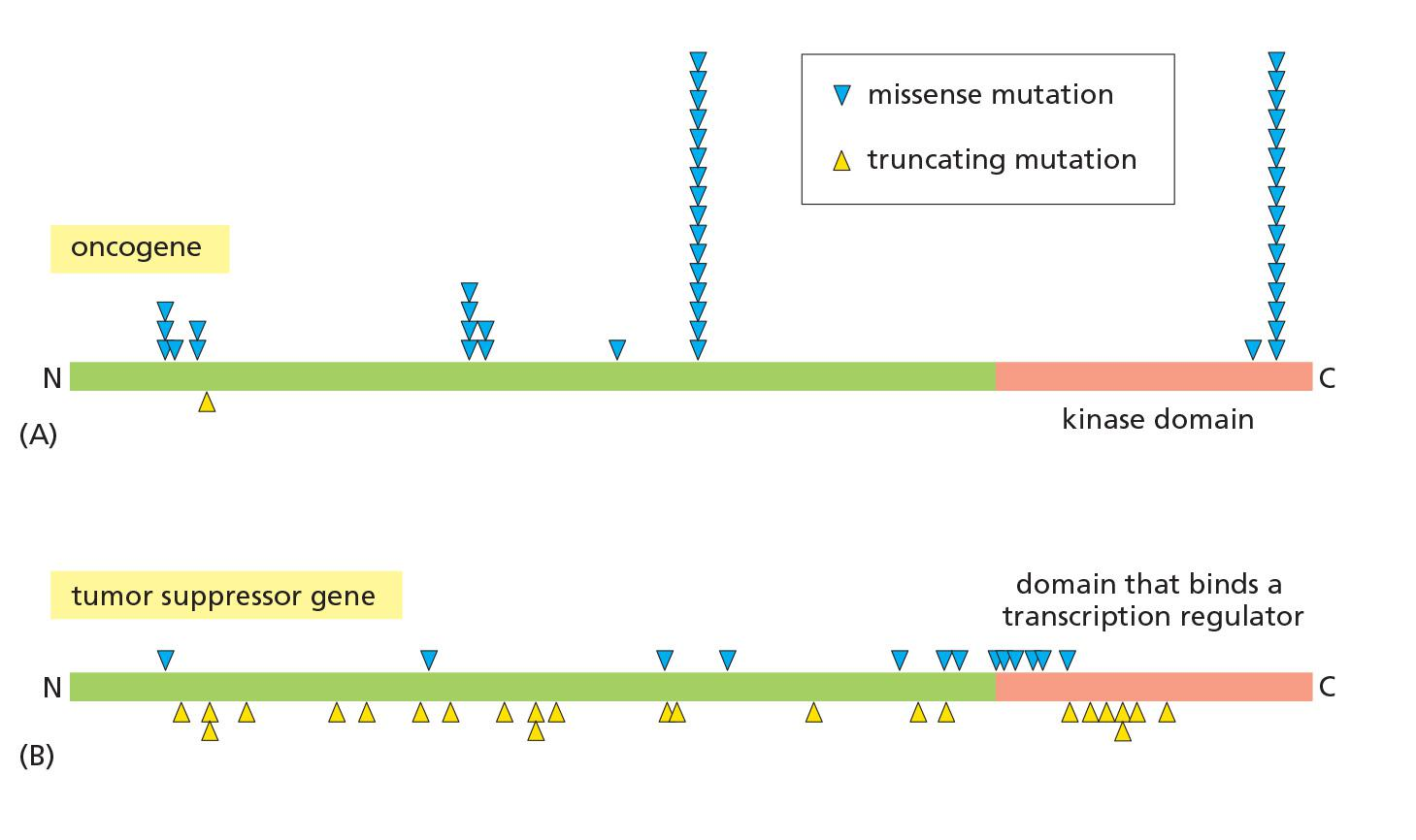
Molecular mechanisms for cancer critical genes: activation of proto-oncogenes
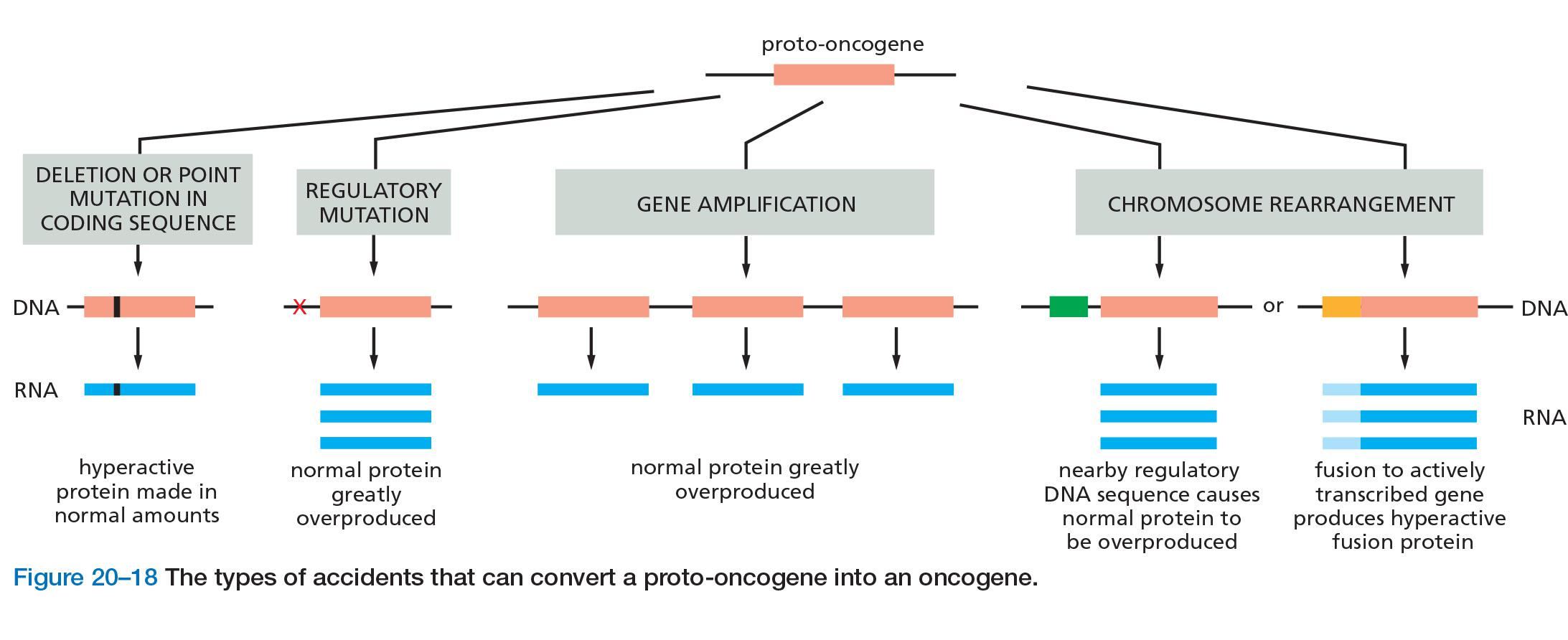
- Genes mutated in cancer can be made overactive in many ways
(1) Example: EGFR mutation can make it active even in the absence of EGF
Molecular mechanisms for cancer critical genes: inactivation of tumor suppressor
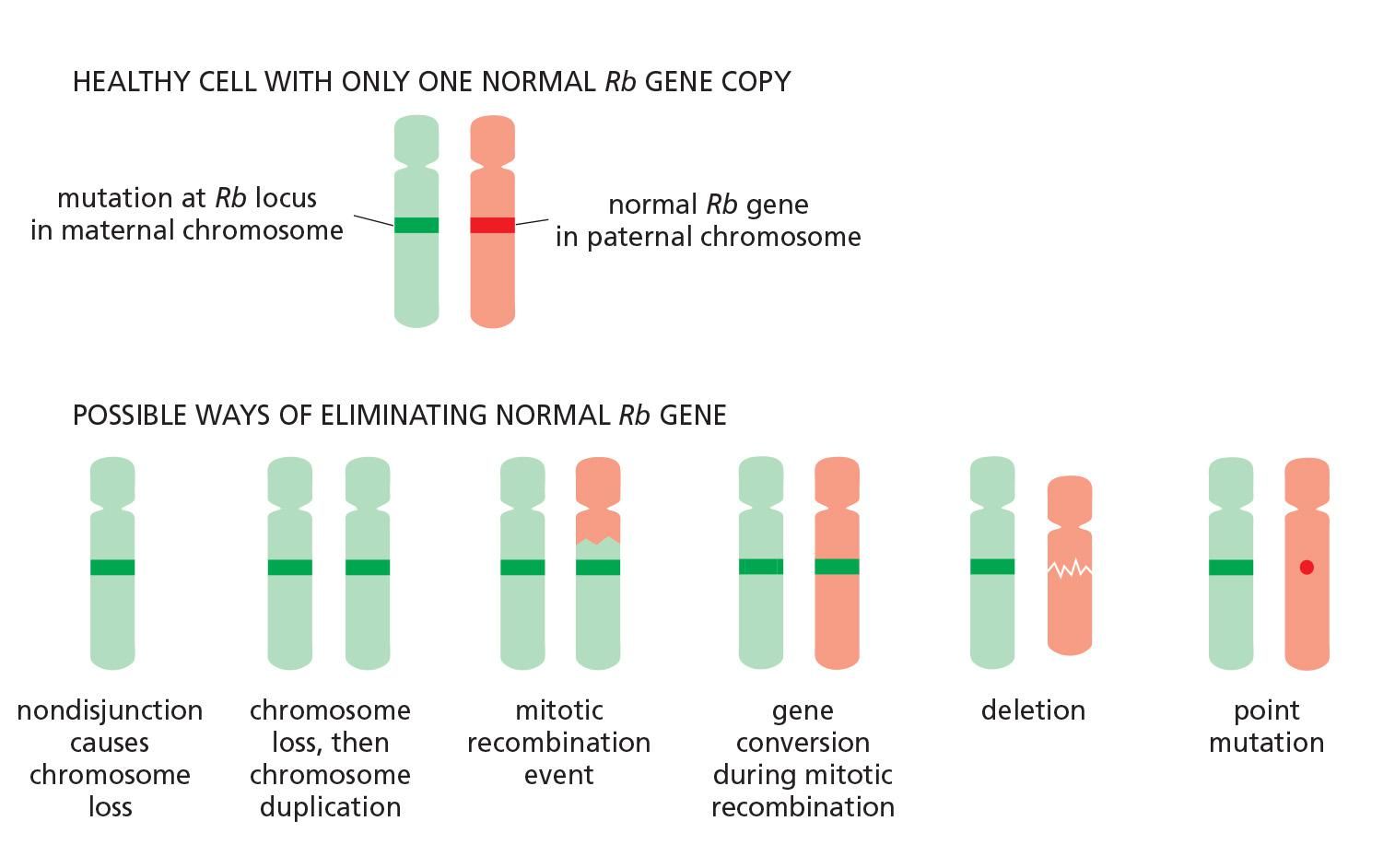
- Six ways of losing the remaining good copy of a tumor suppressor gene through a change in DNA sequences.
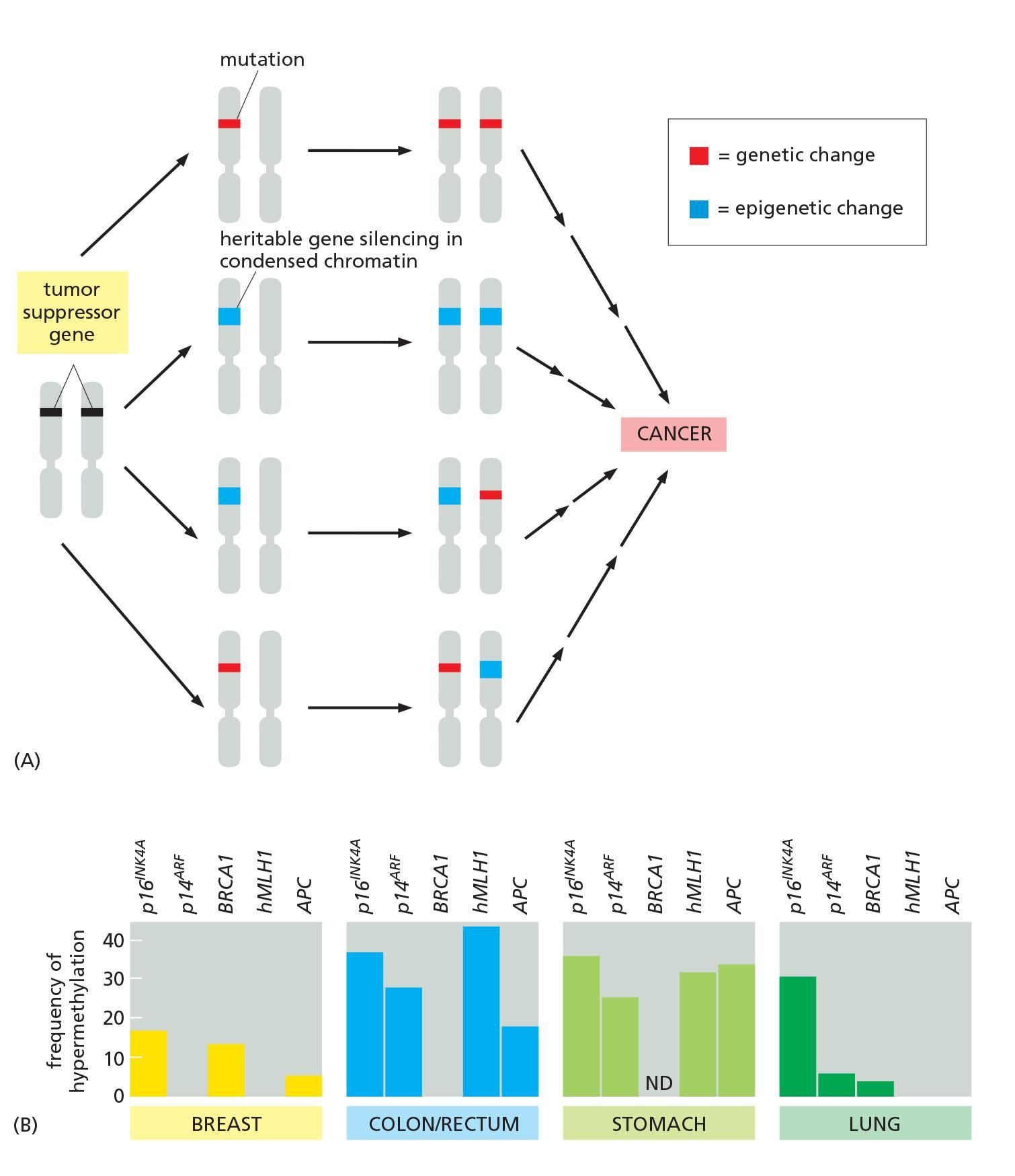
- The pathways leading to loss of tumor suppressor gene function in cancer involve both genetic and epigenetic changes
Cancer cell genomes can be scanned systematically in several different ways.
3. Molecular mechanisms for cancer critical genes with examples
Some genes, like Rb and Ras, are mutated in many cases of cancer and in cancers of many different types.
Disruptions in a handful of key pathways are common to many cancers
- Ras mutation in human cancers
- Rb loss of heterozygosity
- p53 mutation or loss
- APC mutation in colon cancers
- Myc Mutations
Myc
the Myc protein, which acts in the nucleus to stimulate cell growth and division (see Chapter 17), generally contributes to cancer by being overproduced in its normal form.
In some cases, the gene is amplified— that is, errors of DNA replication lead to the creation of large numbers of gene copies in a singlecell. Or a point mutation can stabilize the protein, which normally turns over very rapidly. More commonly, the overproduction appears to be due to a change in a regulatory element that acts on the gene
- For example, a chromosomal translocation can inappropriately bring powerful gene regulatory sequences next to the Myc protein-coding sequence, so as to produce unusually large amounts of Myc mRNA.
- Thus, in Burkitt’s lymphoma(伯基特淋巴瘤), a translocation brings the Myc gene under the control of sequences that normally drive the expression of antibody genes in B lymphocytes.
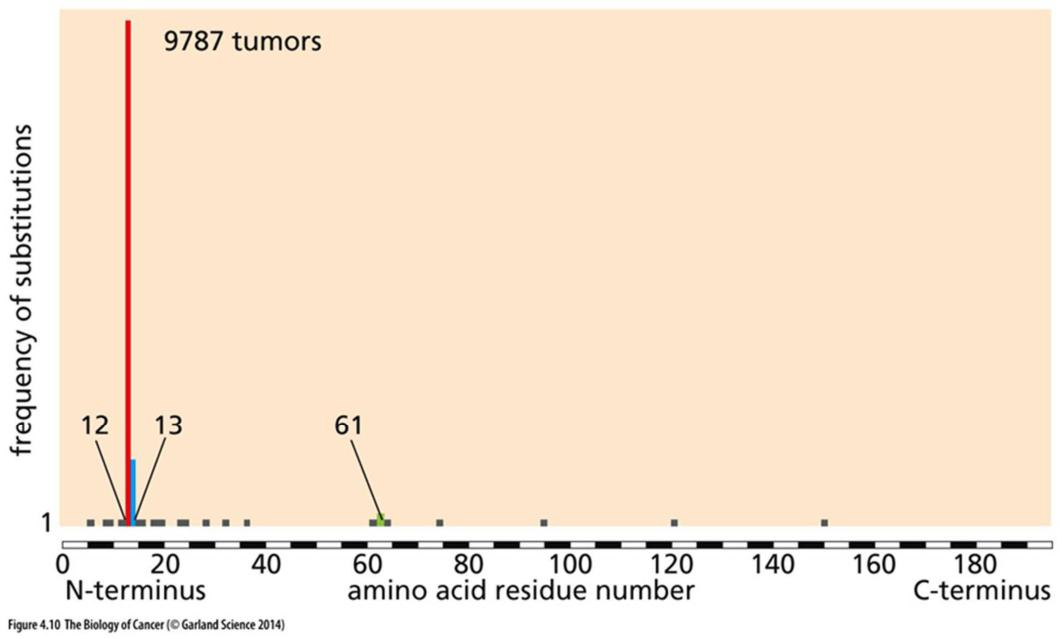
Ras mutation
normal Ras proteins are monomeric GTPases that help transmit signals from cell-surface receptors to the cell interior
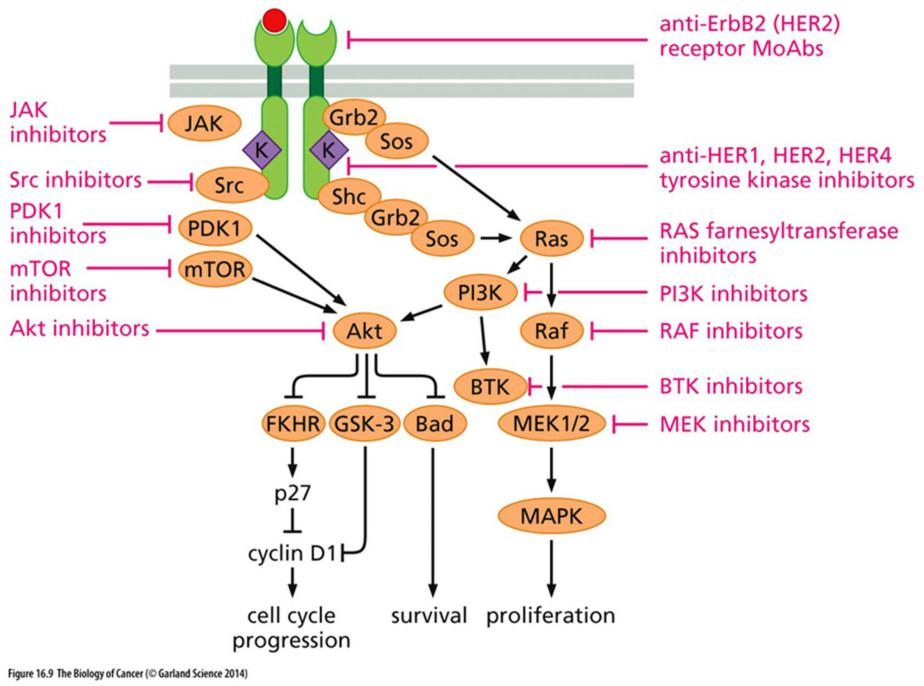
Another consisted of genes in the same regulatory subnetwork as Ras—a more loosely defined system of genes referred to as the RTK/Ras/PI3K pathway, after three of its core components; this pathway serves to transmit signals for cell growth and cell division from the cell exterior into the heart of the cell.
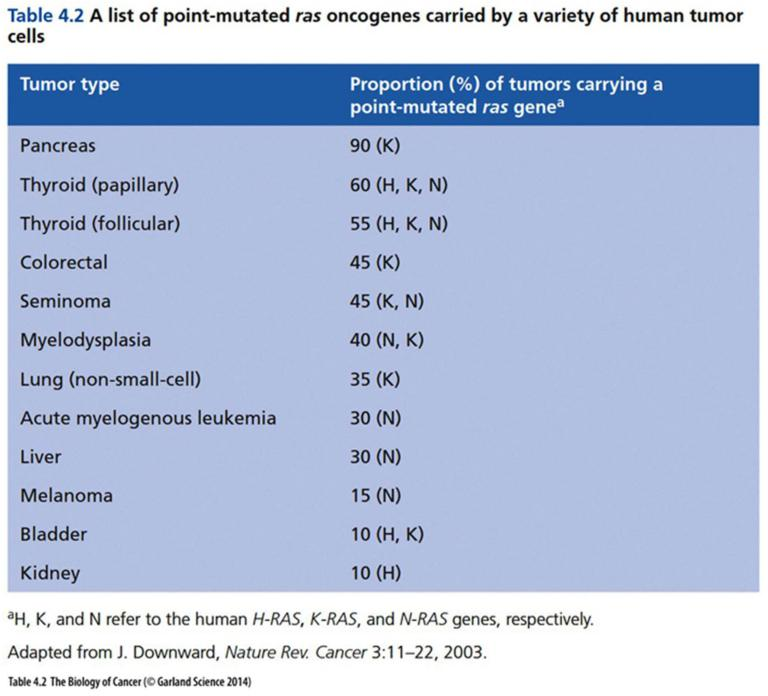
(1) Most oncogenic mutations on Ras occur on amino acid 12
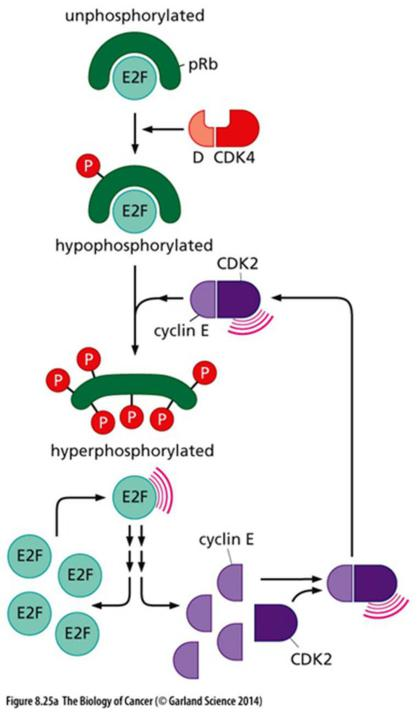
Rb and cell cycle control
Rb protein, which is a universal regulator of the cell cycle present in almost all cells of the body
- One of these groupings consisted of genes in the Rb pathway (that is, Rb itself, along with genes that directly regulate Rb); this pathway governs initiation of the cell-division cycle
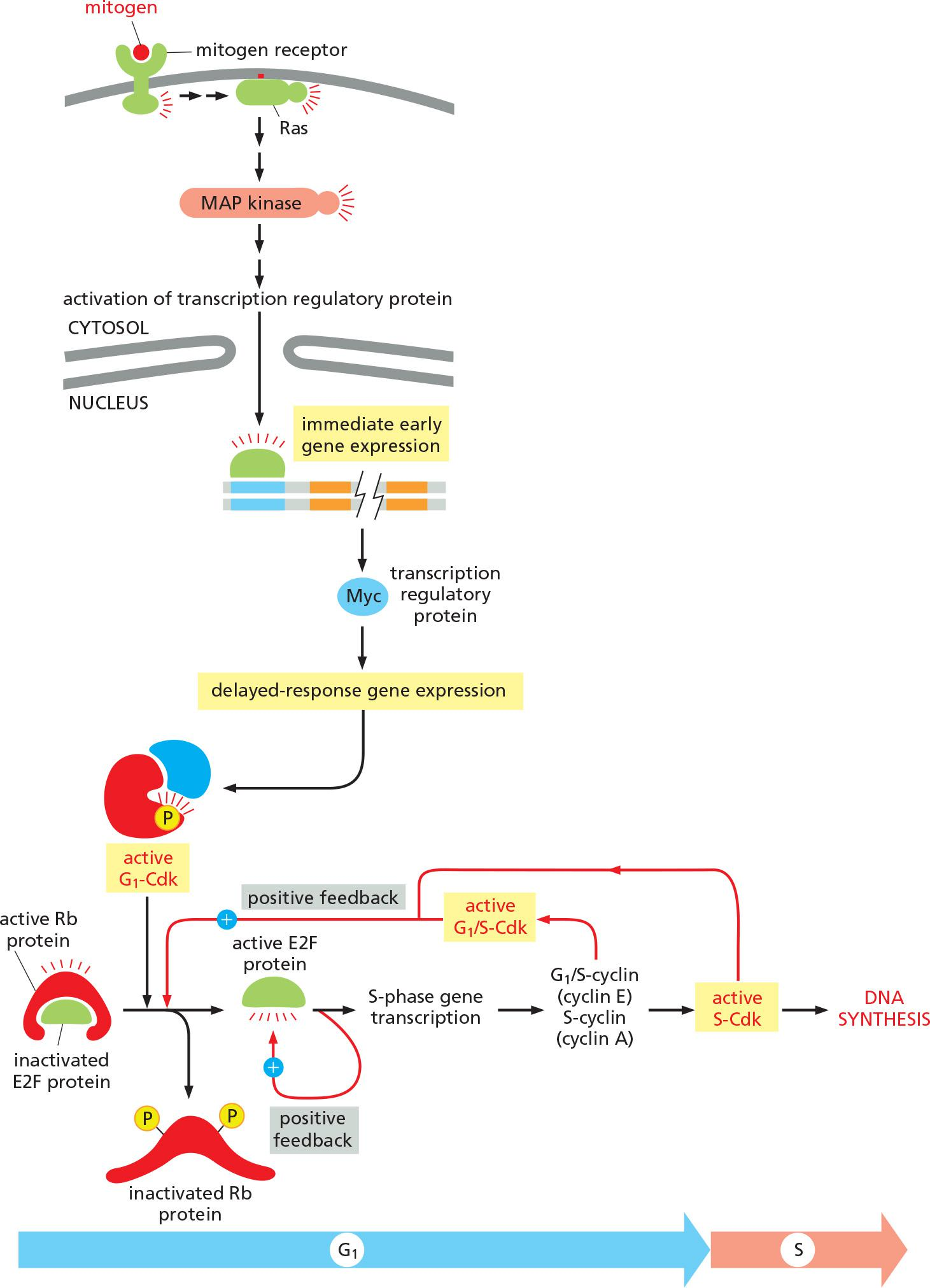
Phosphorylation of Rb promotes cyclin E/cdk activity
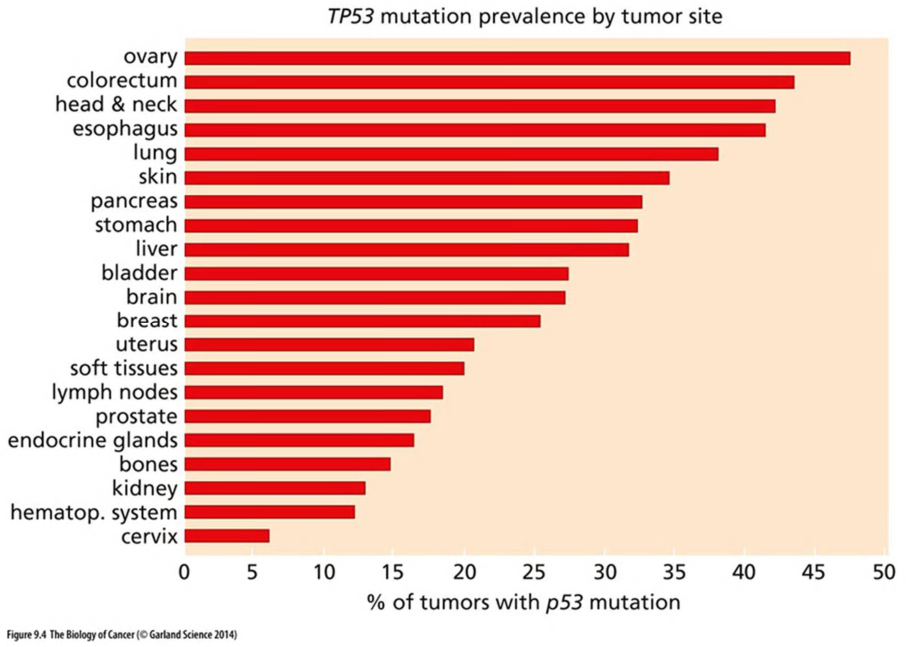
Mutation of p53 in human cancers
The third grouping consisted of genes in a pathway regulating responses to stress and DNA damage—the p53 pathway.
the p53 gene, is mutated in about 50% of all cases of cancer
The p53 pathway, therefore, behaves as a sort of antenna, sensing the presence of a wide range of dangerous conditions, and when any are detected, triggering appropriate action—either a temporary or permanent arrest of cell cycling (senescence), or suicide by apoptosis
Only by losing p53 function can the cancer cells with hyperactive oncogenes survive and progress.
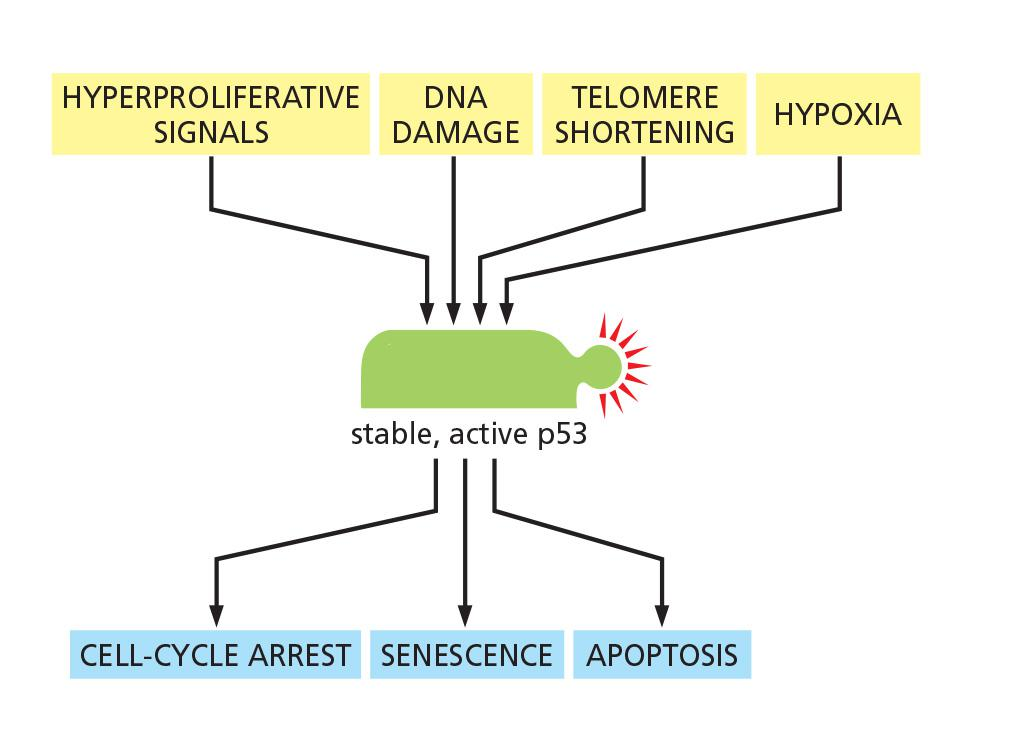
(1) p53 prevent cells from proliferation upon DNA damage
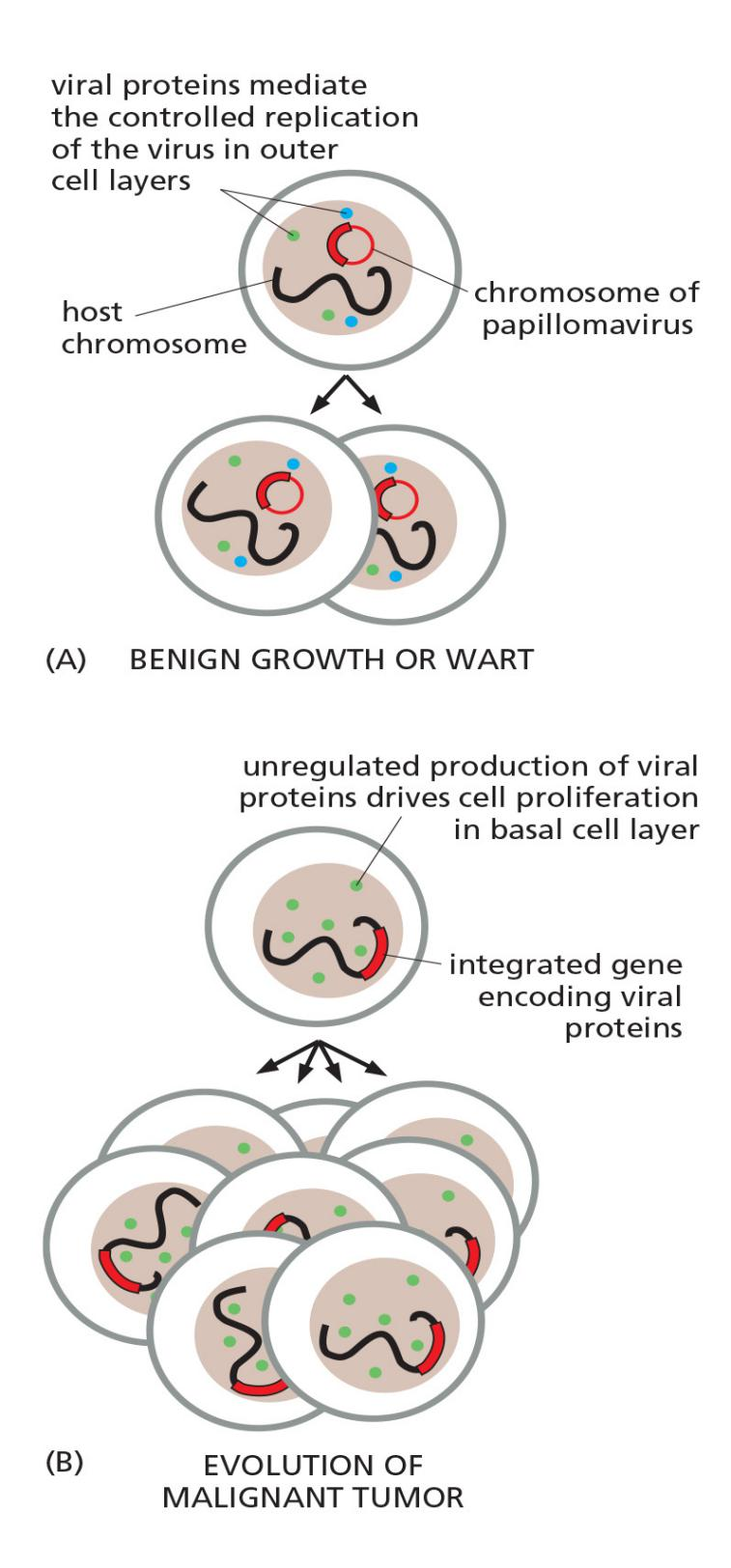
(2) Mode of action for HPV: p53 inactivation
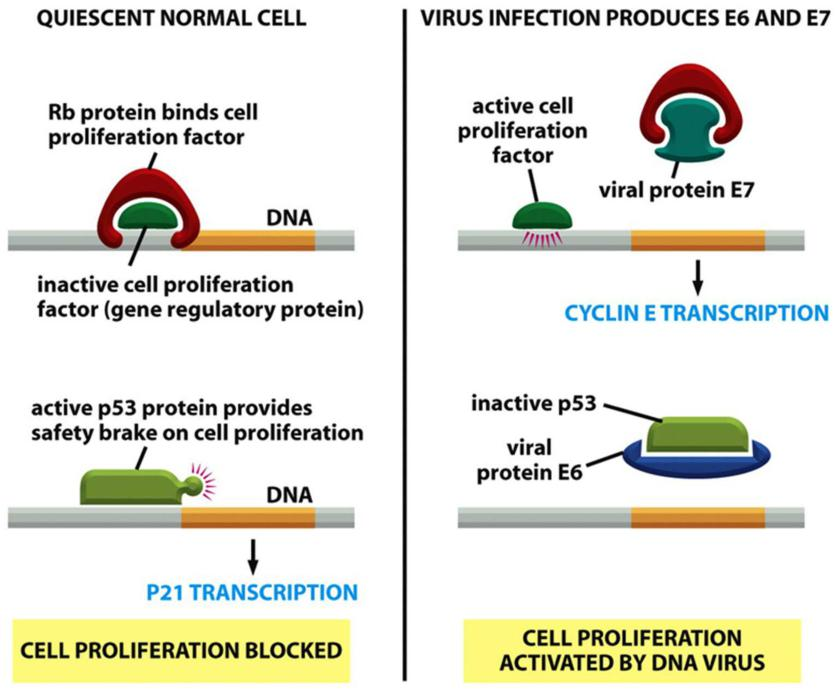
- Cancers of the uterine cervix(子宫颈) can be prevented by vaccination against human papillomavirus(人乳头状瘤病毒)
Mutations in the PI3K/Akt/mTOR pathway
The phosphoinositide 3-kinase (PI 3-kinase)/Akt/mTOR intracellular signaling pathway is critical for cell growth control
The abnormal activation of the PI 3-kinase/Akt/mTOR pathway, which normally occurs early in the process of tumor progression, helps to explain the excessive rate of glycolysis that is observed in tumor cells, known as the Warburg effect
Also very common in cancers is the loss of the PTEN phosphatase, an enzyme that normally suppresses the PI 3-kinase/Akt/mTOR pathway by dephosphorylating the PI (3,4,5) P3 molecules that the PI 3-kinase forms
- PTEN is thus a common tumor-suppressor gene.
A few key lesions in a large fraction of human colorectal cancers
Wnt pathway
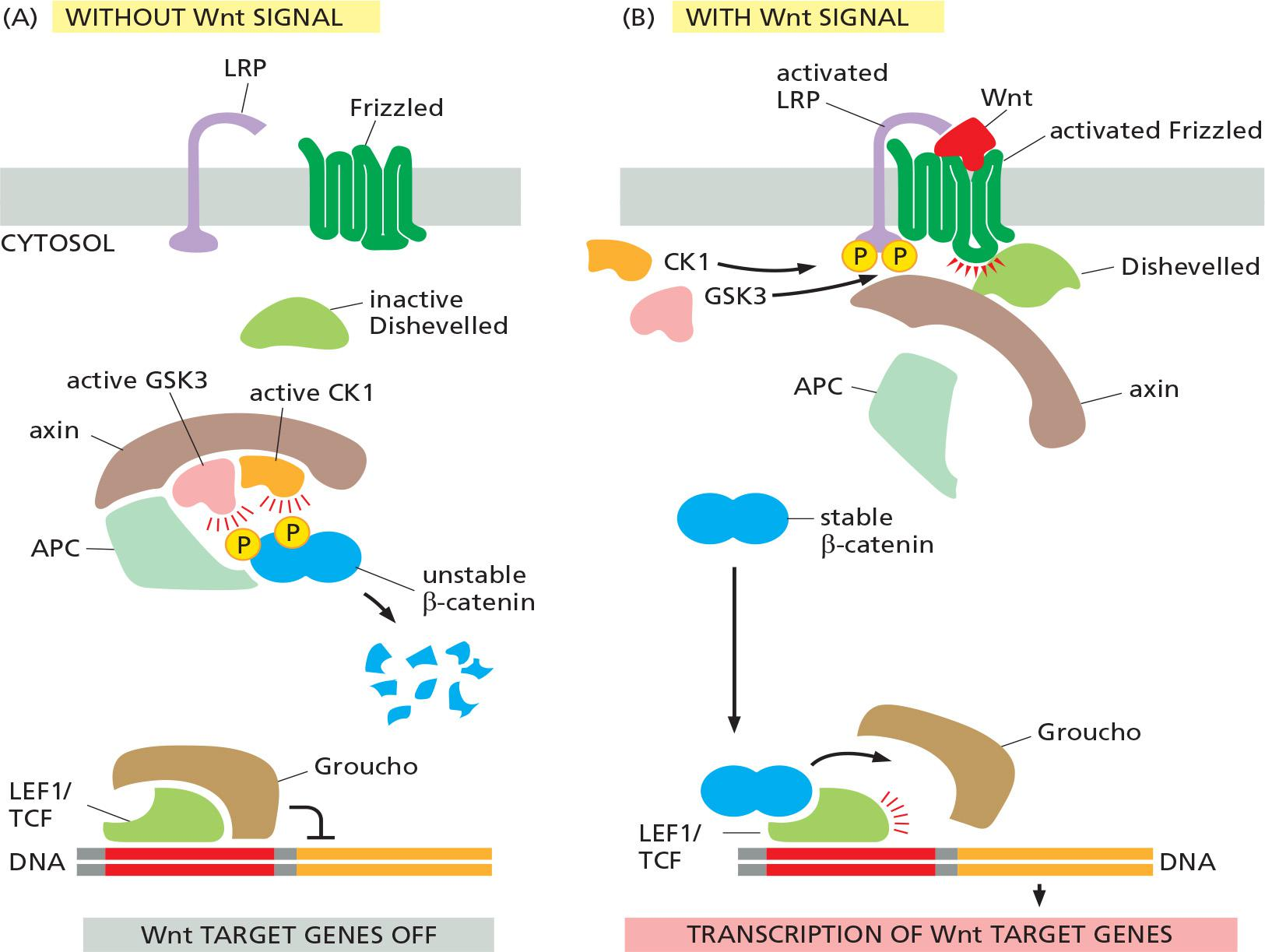
- Co-receptor: LRP ( LDL-receptor-related protein) and Frizzled
- Latent transcription regulators: β-catenin
- Scaffold protein:
- Adenomatous polyposis coli (APC)
- axin
APC loss-of-function mutations induce polyposis, which usually happens before colon cancer
The Apc protein, as we now know, is an inhibitory component of the Wnt signaling pathway
- It binds to the β-catenin protein, another component of the Wnt pathway, and helps to induce the protein’s degradation
- Apc prevents the β-catenin from migrating to the nucleus, where it would act as a transcriptional regulator to drive cell proliferation and maintain the stem-cell state
Changes underlying the development of colorectal carcinoma
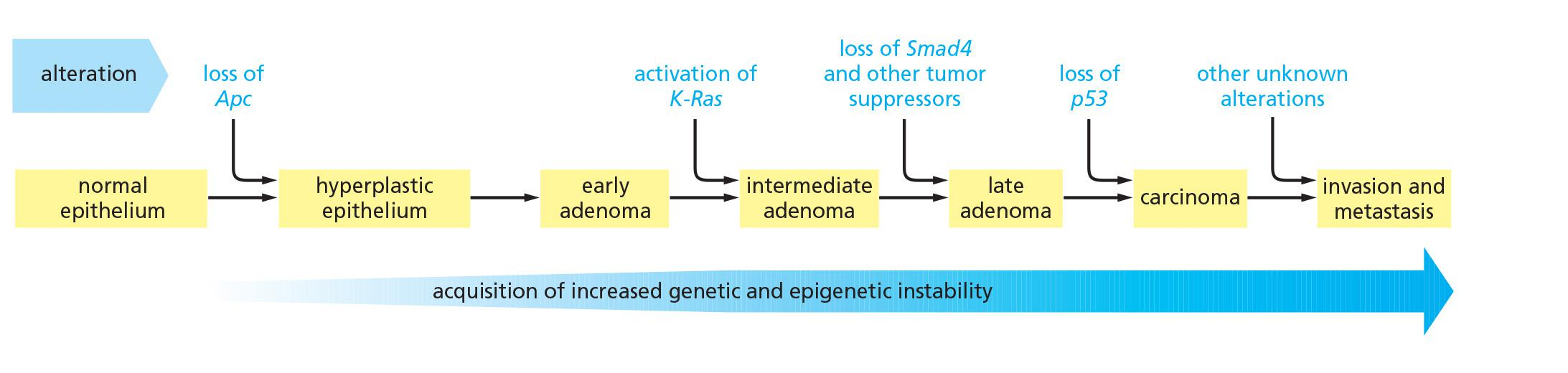
Colorectal cancers evolve slowly via a succession of visible changes
Suggested typical sequence of genetic changes underlying the development of a colorectal carcinoma.
Metastasis remains largely unknown
1. Epithelial-mesenchymal transition is important in metastasis
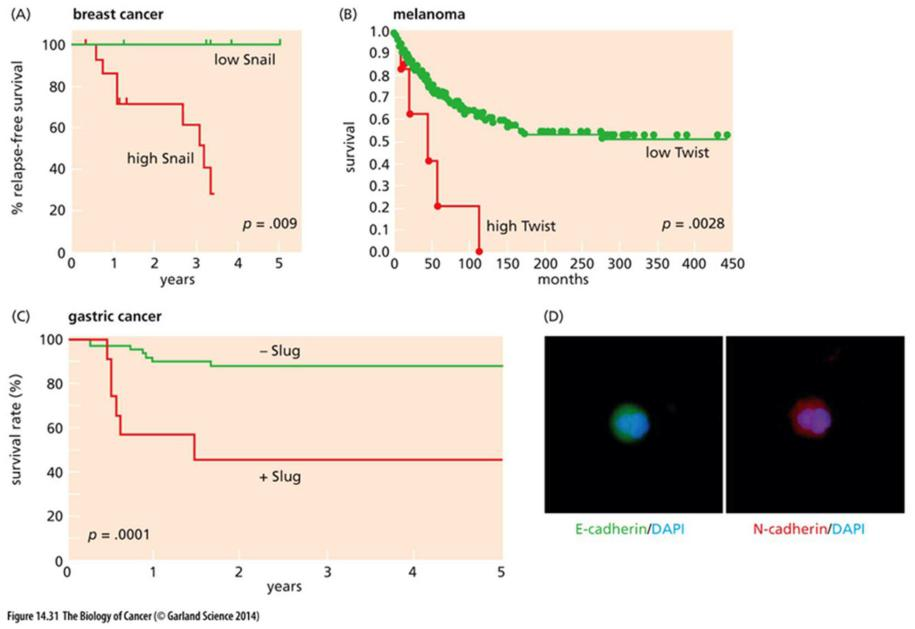
- EMT(epithelial–mesenchymal transition) promoting transcription factors promotes metastasis
- EMT is associating to increased migration of epithelial cells
Increased activity of MT-MMP promotes cancer invasion
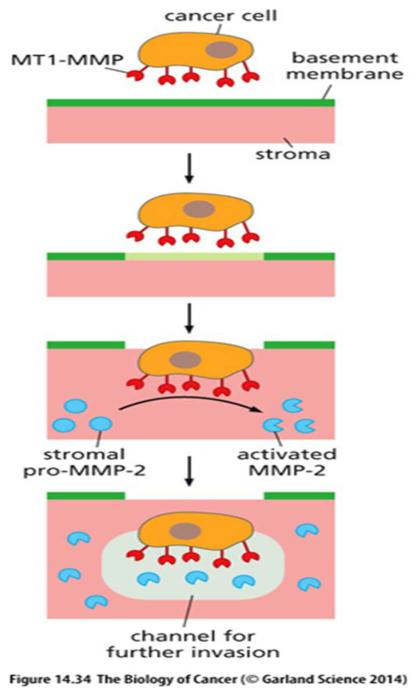
- MT-MMP: membrane type MMP
三、Cancer stem cells
Stem cell–like cancer cells
- Take a tumor mass, make single cell suspension
- Inject single cell into immunodeficiency mice to induce tumor formation
- <<1% of the isolated cancer cells can induce a new tumor formation
- Those that can induce tumor formation has the characteristics of cancer stem cells: They are capable of indefinite self-renewal, but they also give rise to rapidly cells that have limited capacity to self-renewal. They are responsible for maintaining the Population of cells in a tumor.
Cancers may arise from cancer stem cells
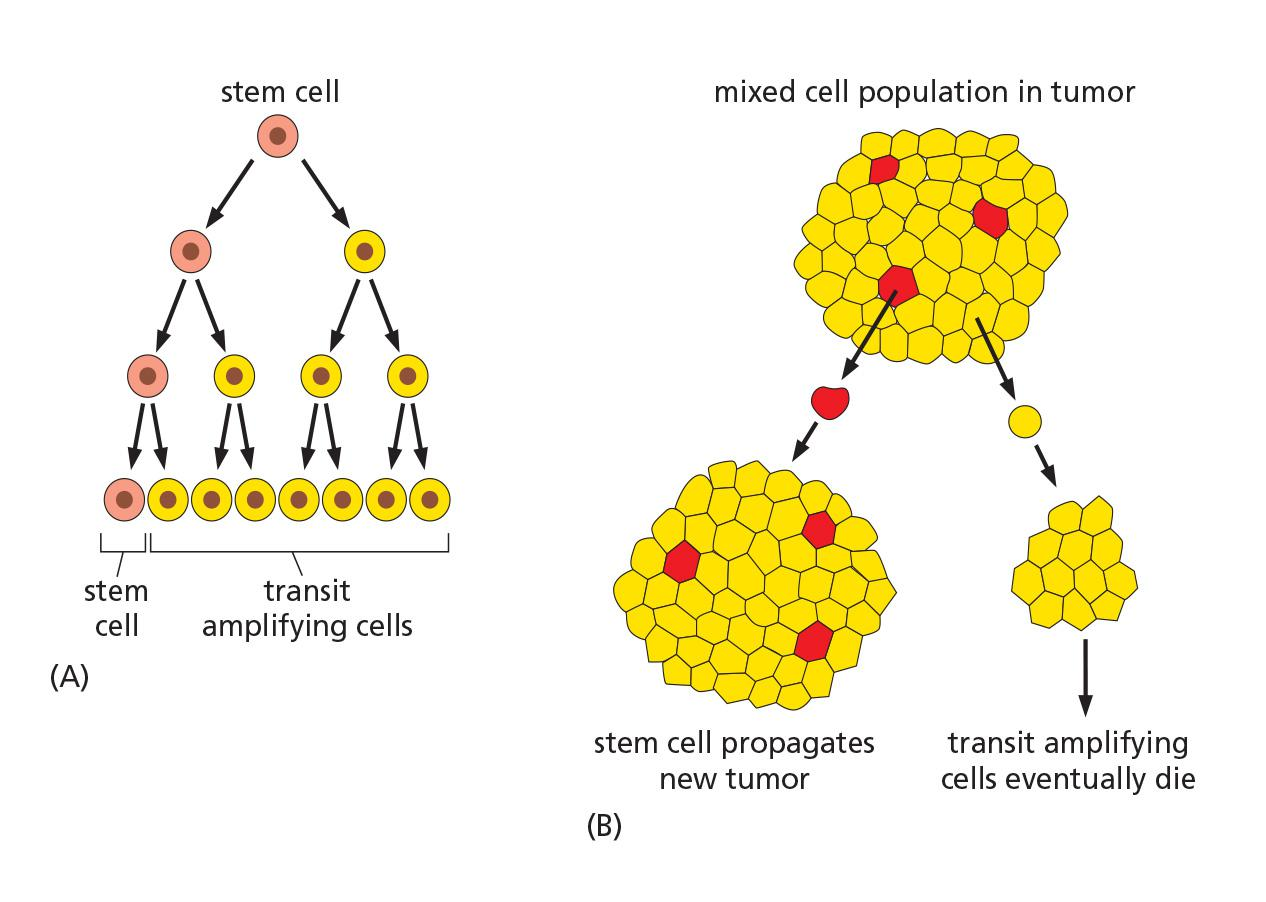
On average, the two fates—stem cell or differentiating cell—normally occur with equal probability, so that half the daughters of stem-cell divisions take the one path and half take the other.
- Experiments with breast cancer cells have revealed that, instead of following a rigid program from stem cell to transit amplifying cell to terminally differentiated cell, these cancer cells can randomly switch to and fro(来回切换)—with a certain low transition probability—between different states of differentiation that express different molecular markers
feedback controls regulate the process, adjusting this balance of cell-fate choices to correct for any departure(离开、离去) from the proper cell population numbers.
The cancer stem-cell phenomenon, whatever its basis, implies that even when the tumor cells are genetically similar, they are phenotypically diverse
- Some cancers seem to be organized in a similar way: they consist of rare cancer stem cells capable of dividing indefinitely, together with much larger numbers of dividing transit amplifying cells that are derived from the cancer stem cells but have a limited capacity for self-renewal
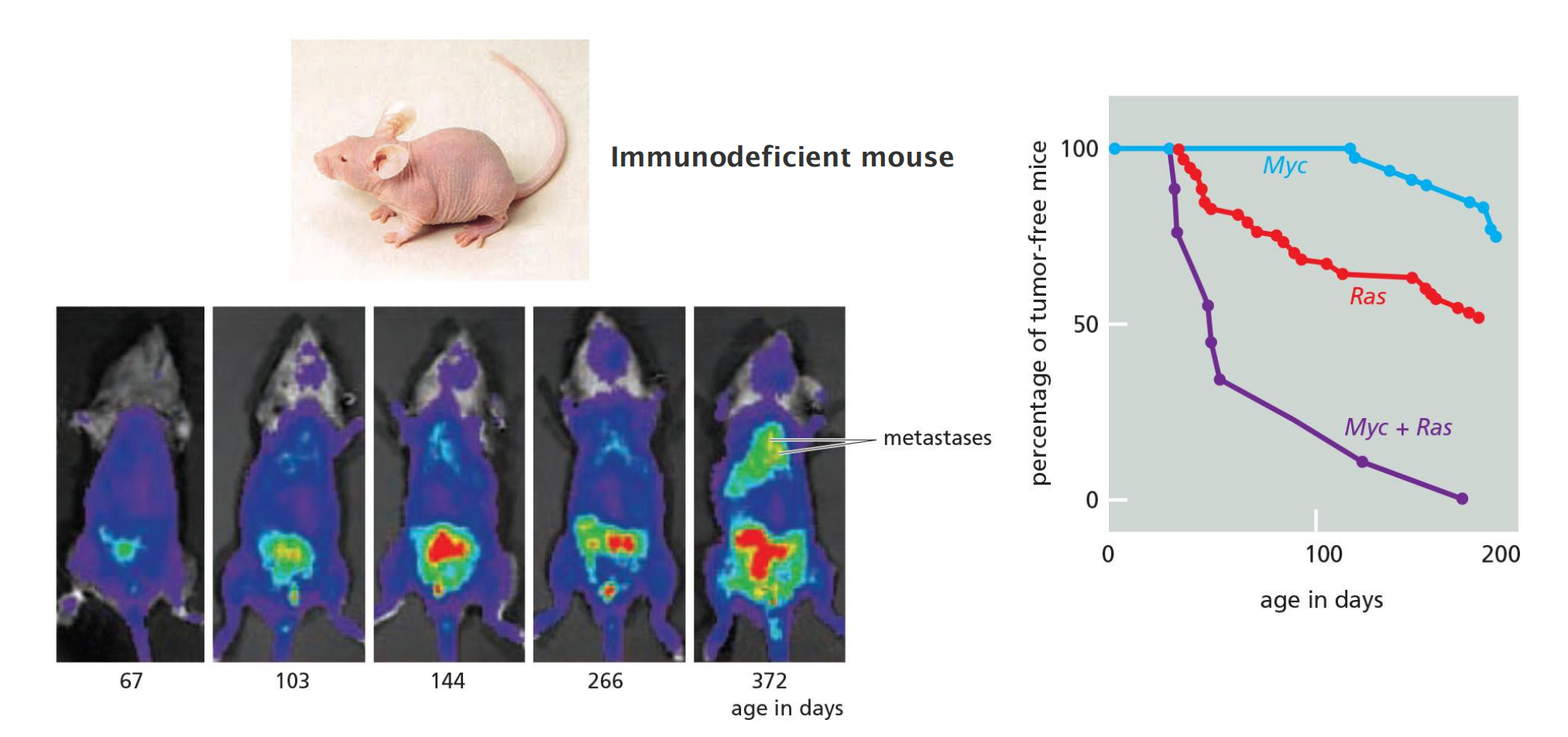
四、Study cancer using mice
五、Cancer prevention and treatment
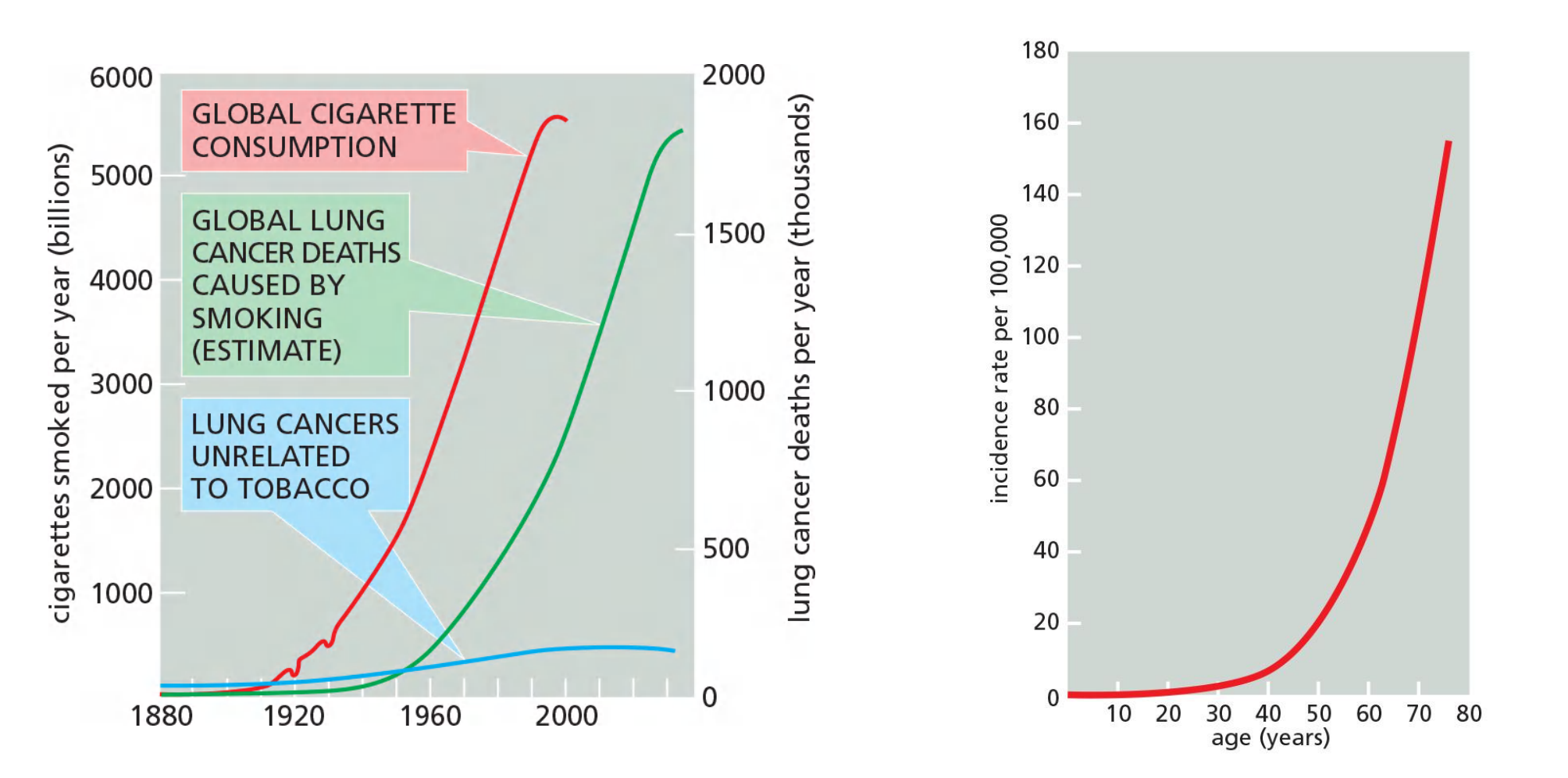
Epidemiology Reveals That Many Cases of Cancer Are Preventable
the differences are thought to be due mostly to environmental, not genetic, factors. From such findings, it has been suggested that 80–90% of cancers should be avoidable, or at least postponable
Cancer incidence related to environmental influences
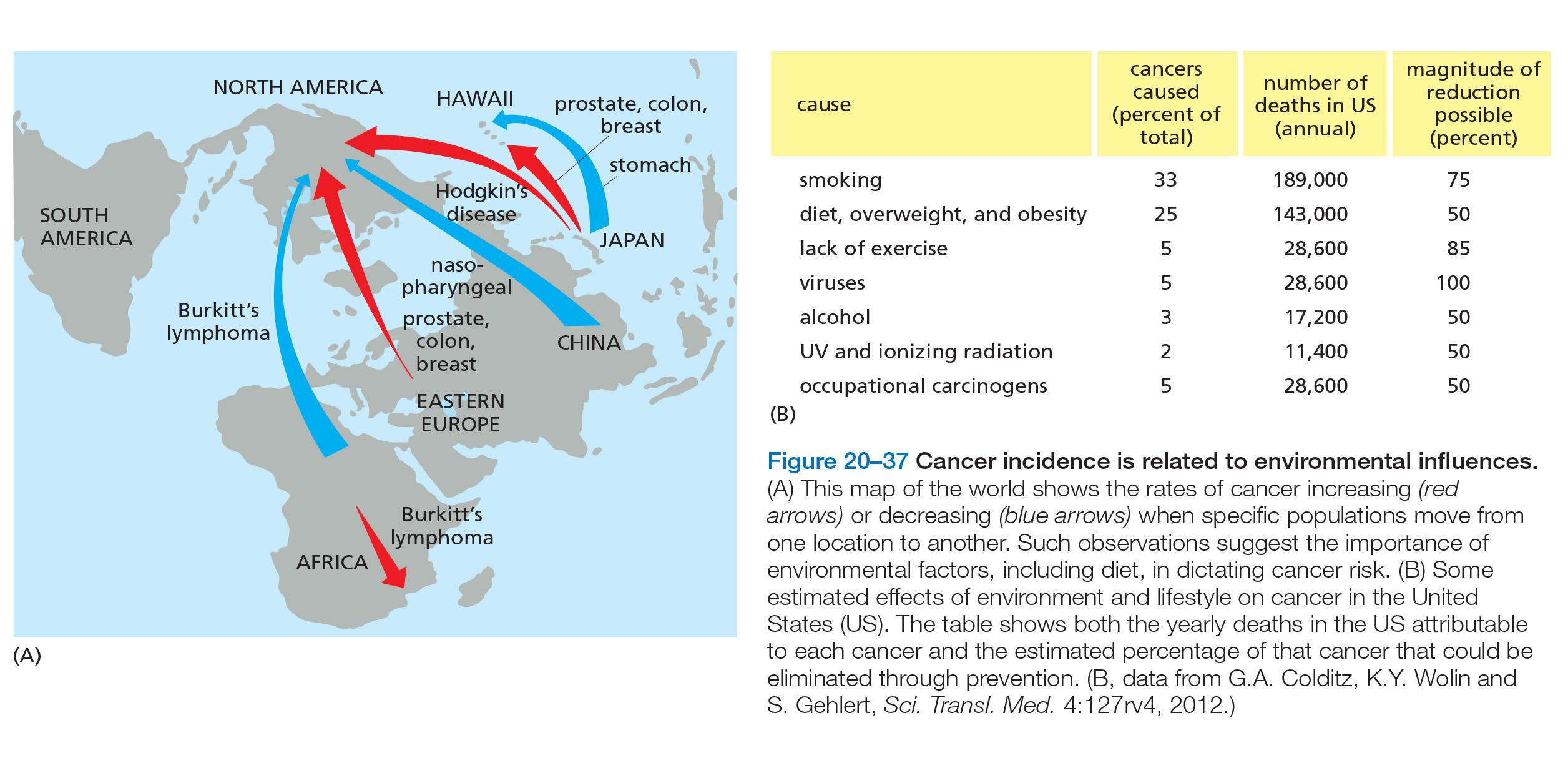
- Fifty percent of cancers could be prevented by changes in lifestyle
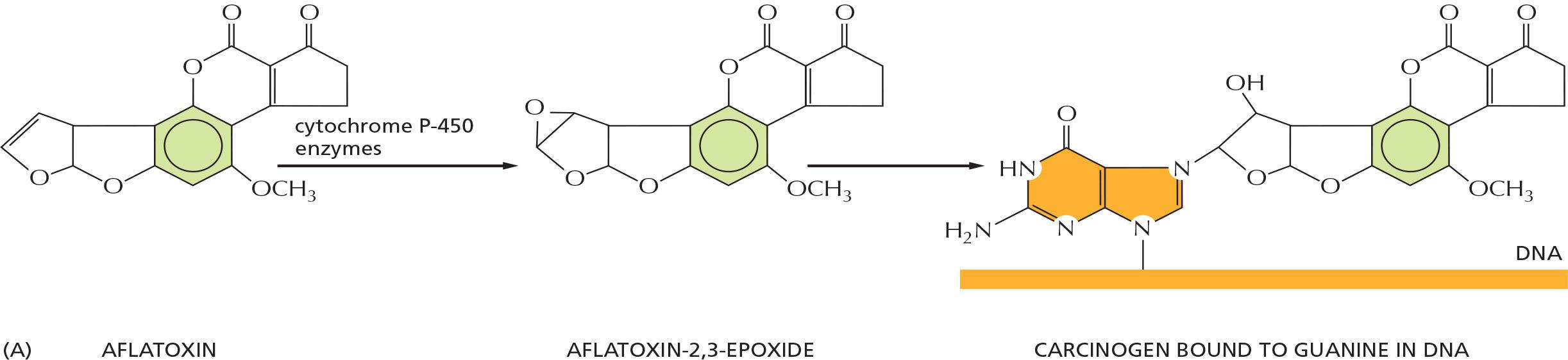
Some known carcinogens
Although these chemical carcinogens are diverse in structure, a large proportion of them have at least one shared property—they cause mutations, mutations can be tested by Ames Test
- benzo[a]pyrene
- aflatoxin B1
- 2-naphthylamine
- asbestos
Viruses associated with human cancers
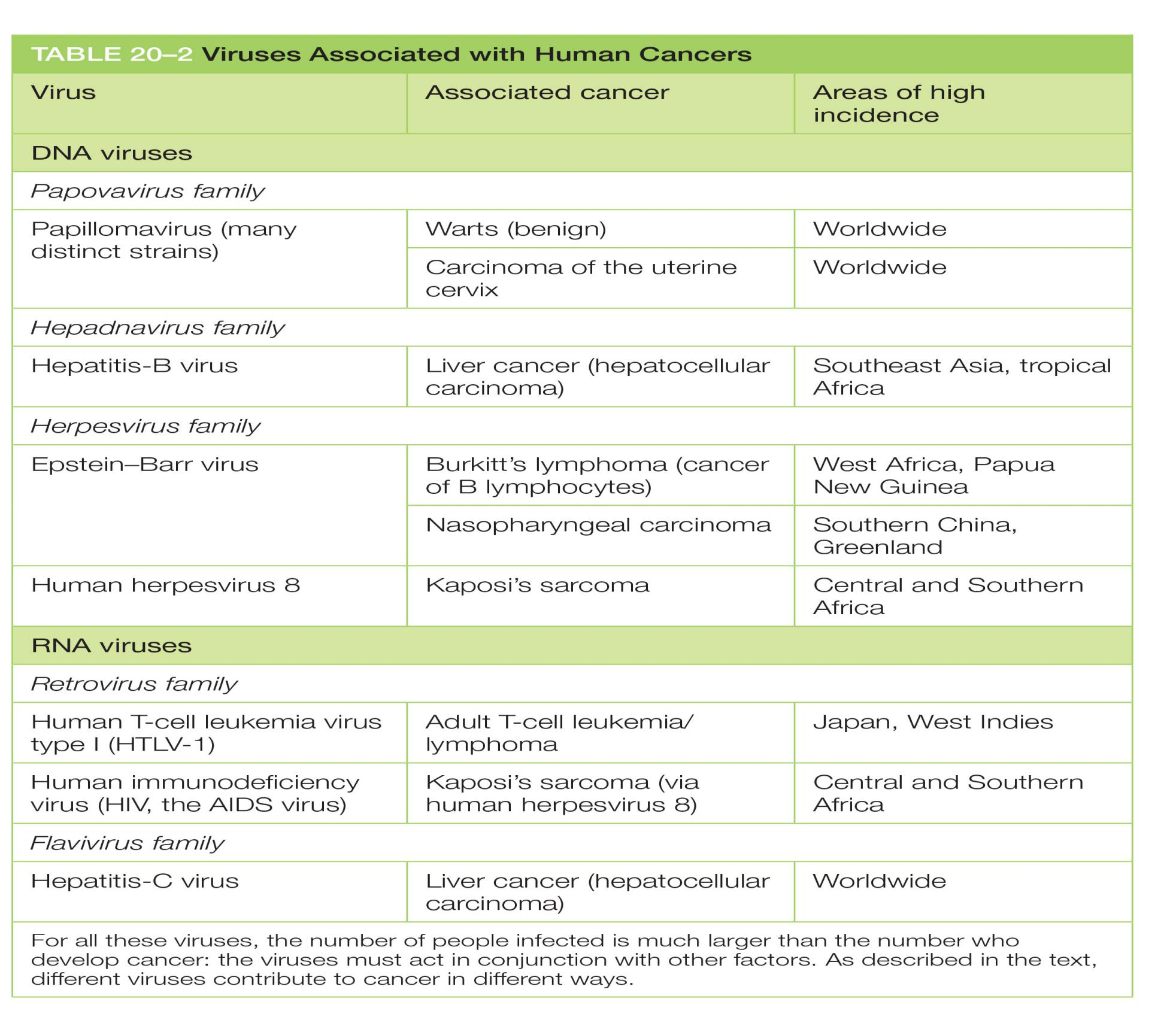
- Viruses and other infections contribute to a significant proportion of human cancers
cancer treatment
1. Traditional cancer treatment ( before 1975)
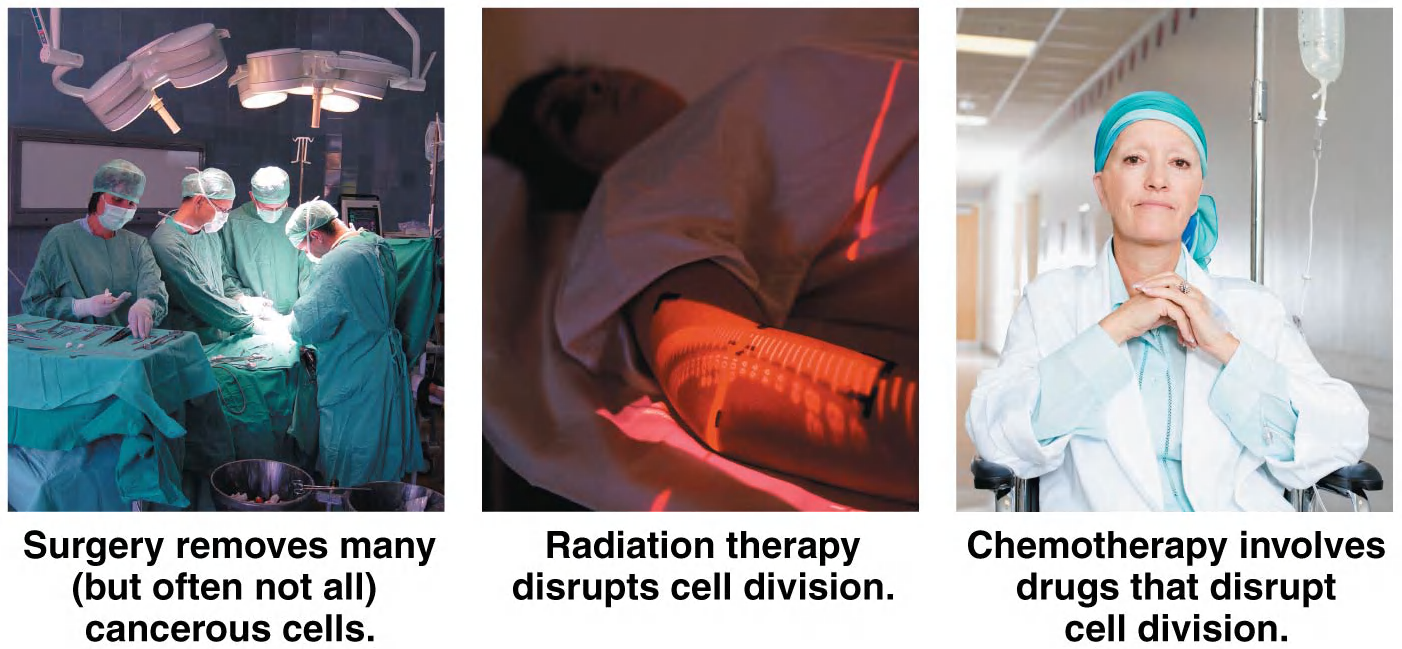
- Three cancer treatments: “Slash, burn, and poison”
2. drugs
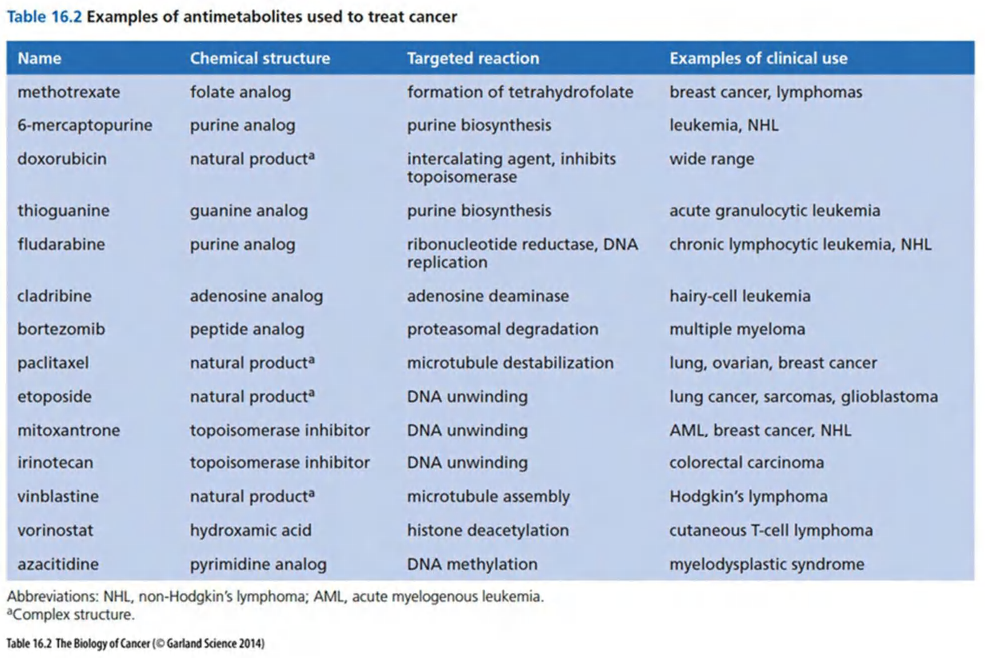
- Examples for some of them, all are generally cytotoxic
More specific cancer drug development
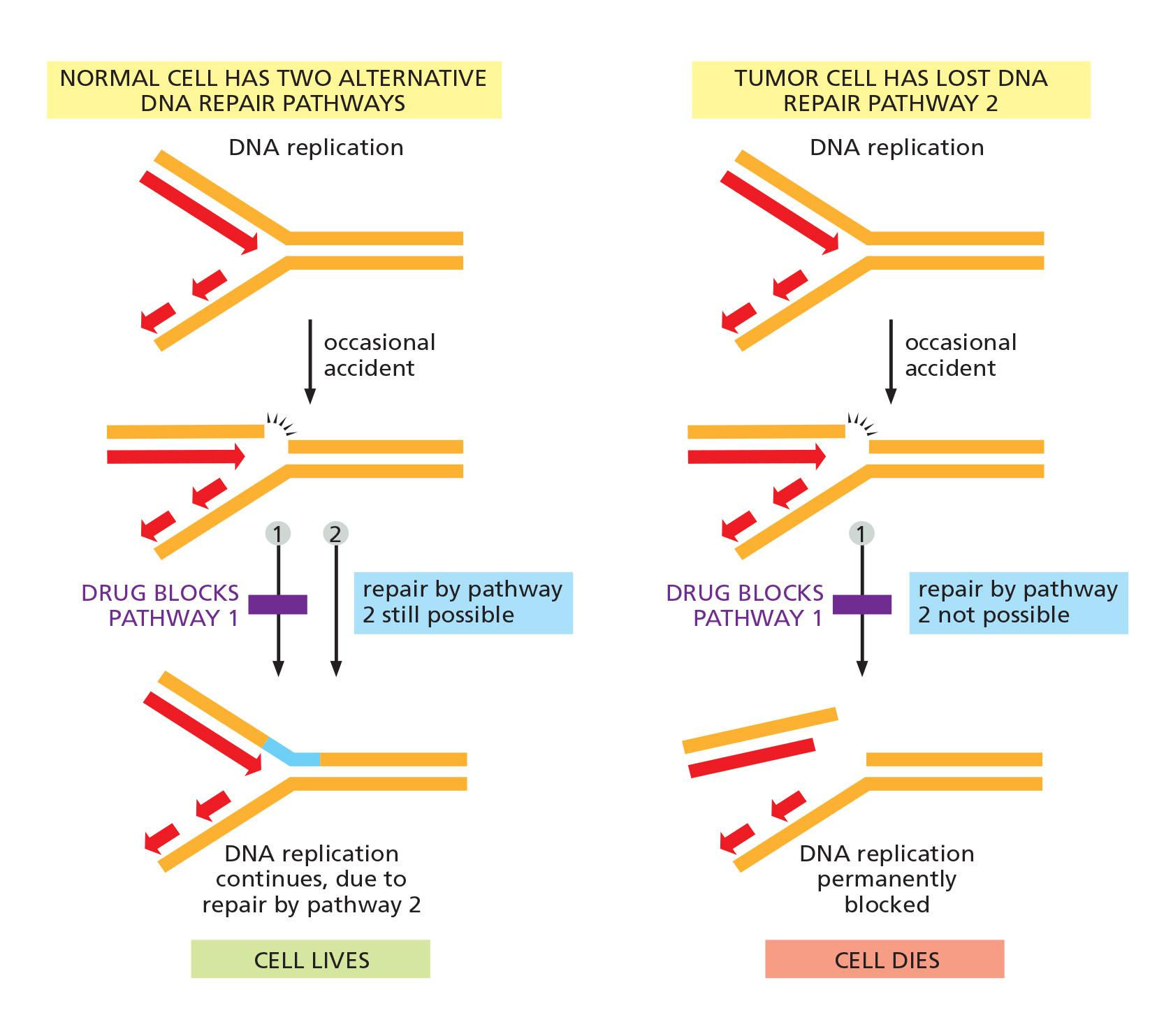
Tumor’s genetic instability can be exploited for cancer therapy
genetic instability is not an accidental by-product of malignant behavior but a contributory cause—and that cancer cells can acquire this instability in multiple ways. is not an accidental by-product of malignant behavior but a contributory cause—and that cancer cells can acquire this instability in multiple ways.
The conversion of the Abl proto-oncogene into an oncogene in patients with CLL
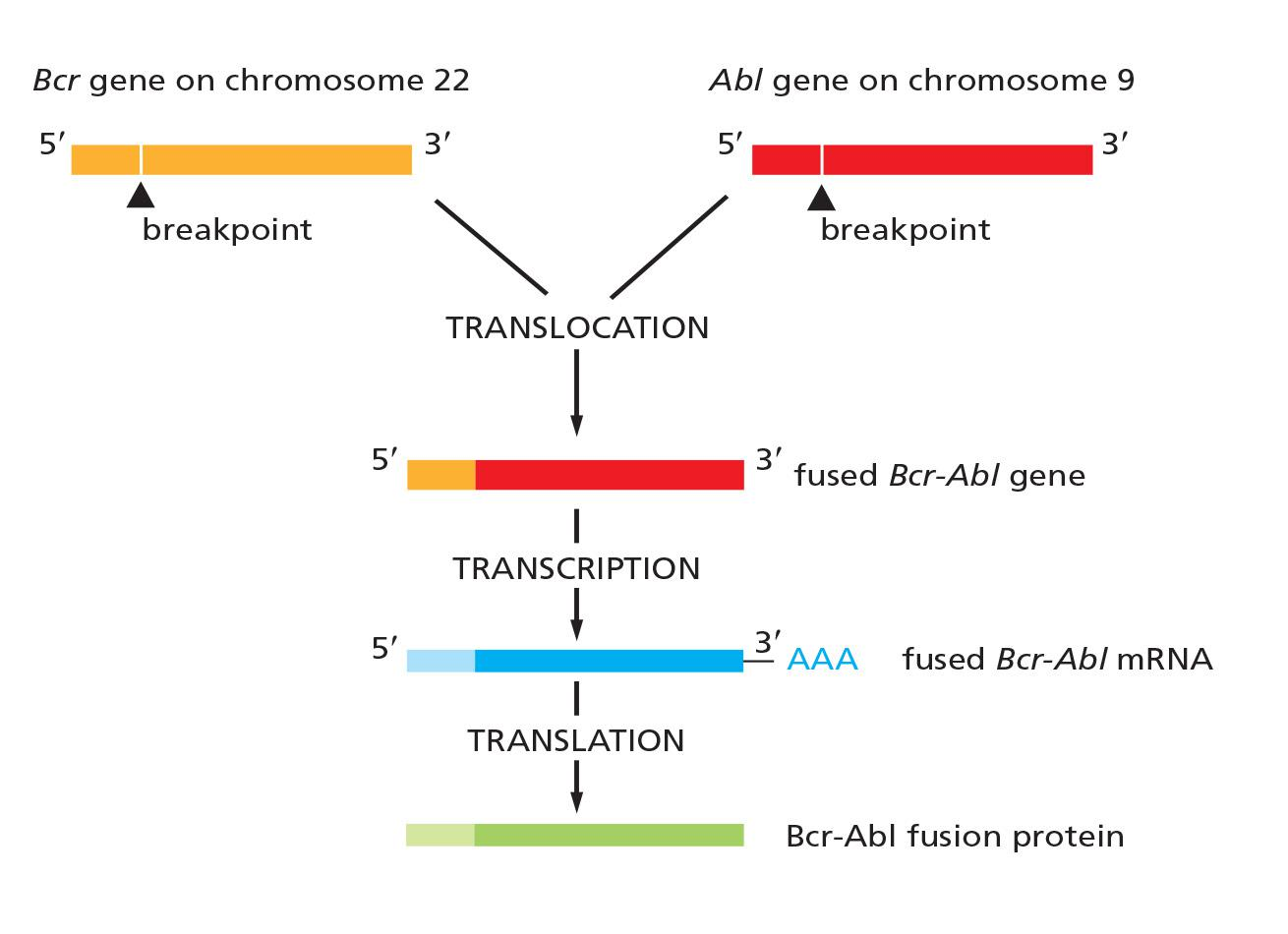
- CLL: chronic myelogenous Leukemia
The successful case of Imatinib (Gleevec)
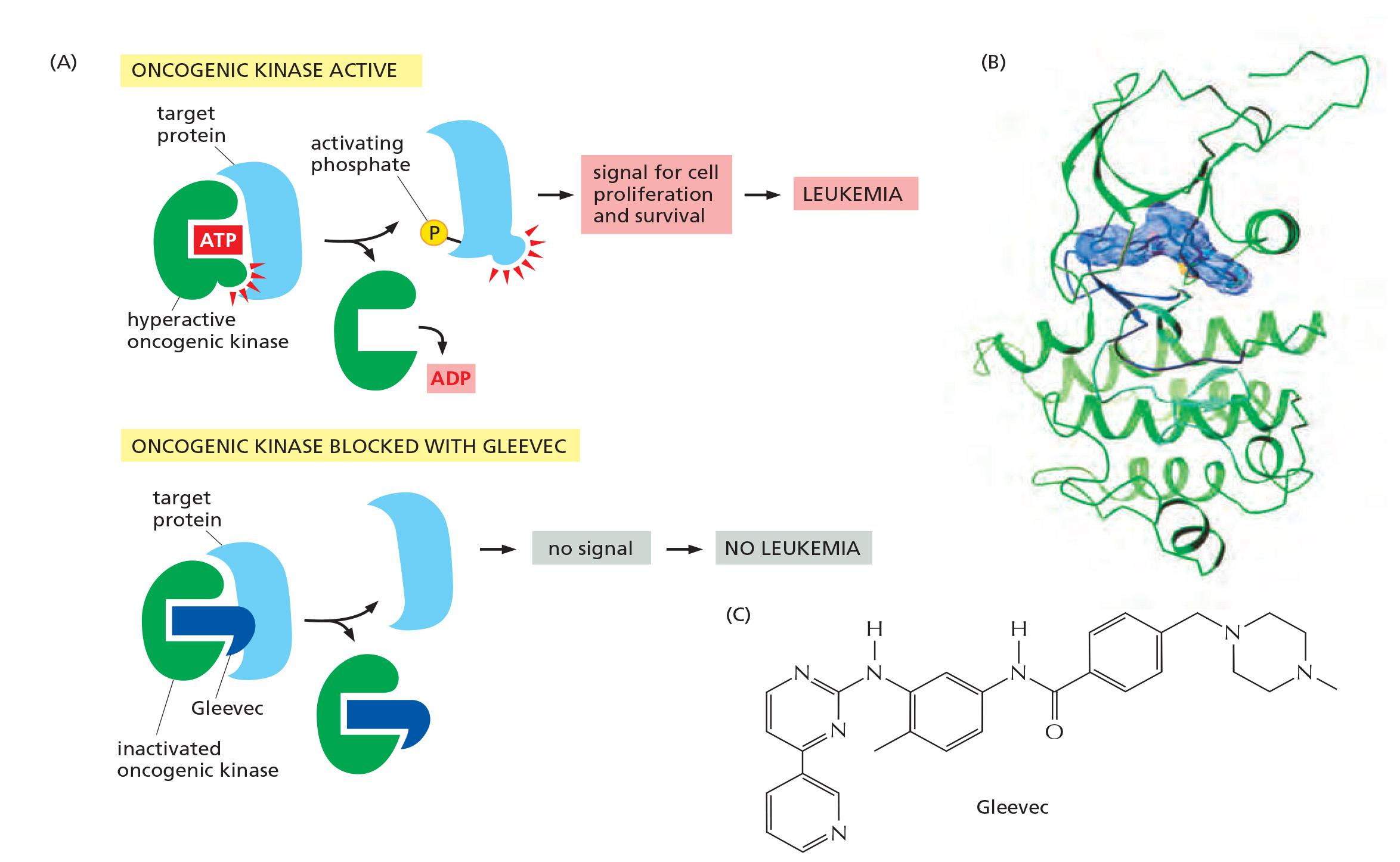
- Target BCR-Abl, which is the initiating oncogene to induce chronic myelogenous leukemia (CML), greatly increase the lifespan of this type of leukemia patients.
- The inhibition of Gleevec to BCR-Abl is specific
Targeting Ras–MAP-kinase signaling pathway
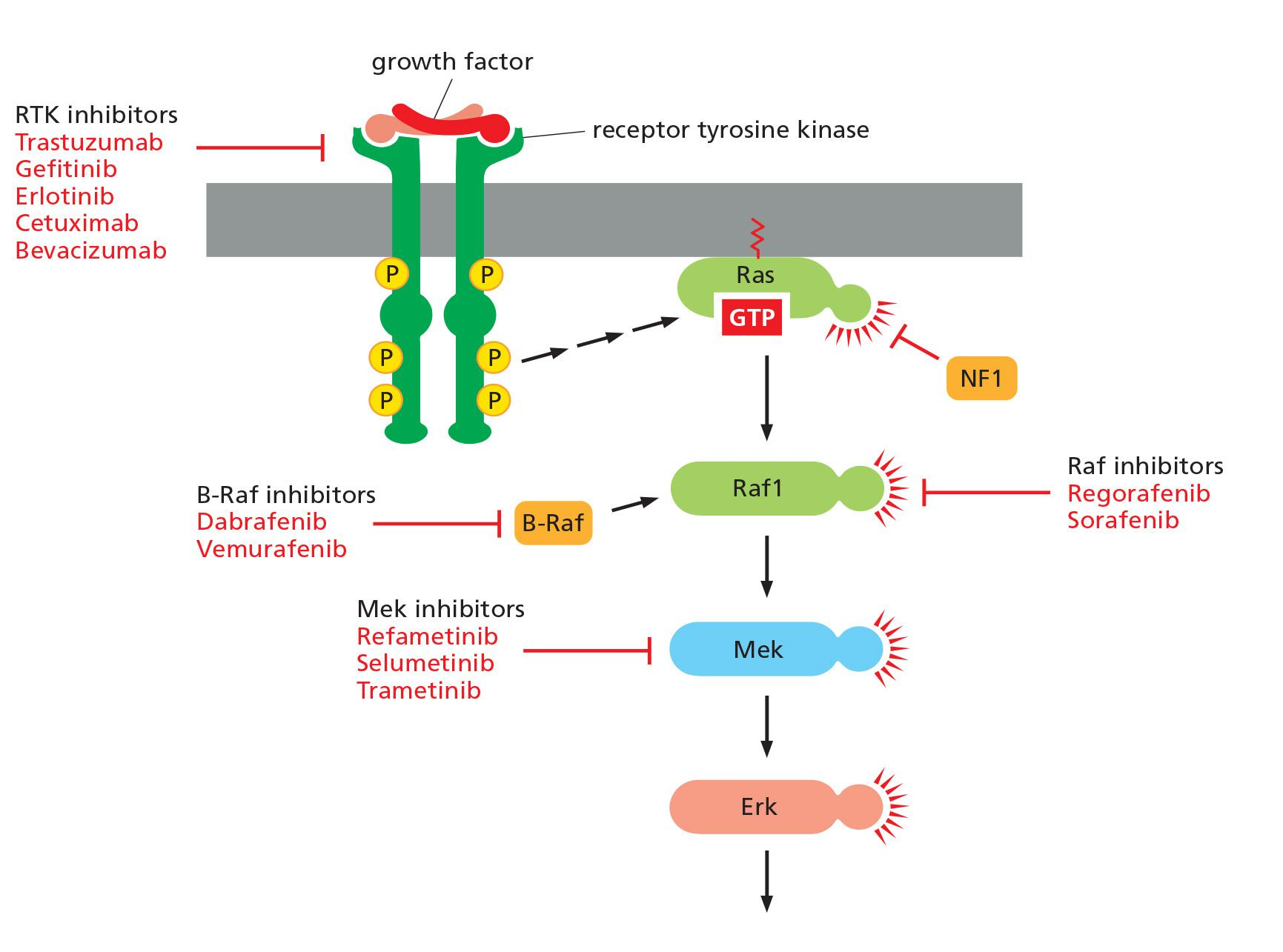
- Some anticancer drugs and drug targets in the Ras–MAP-kinase signaling pathway
Drug resistance and combinational treatment
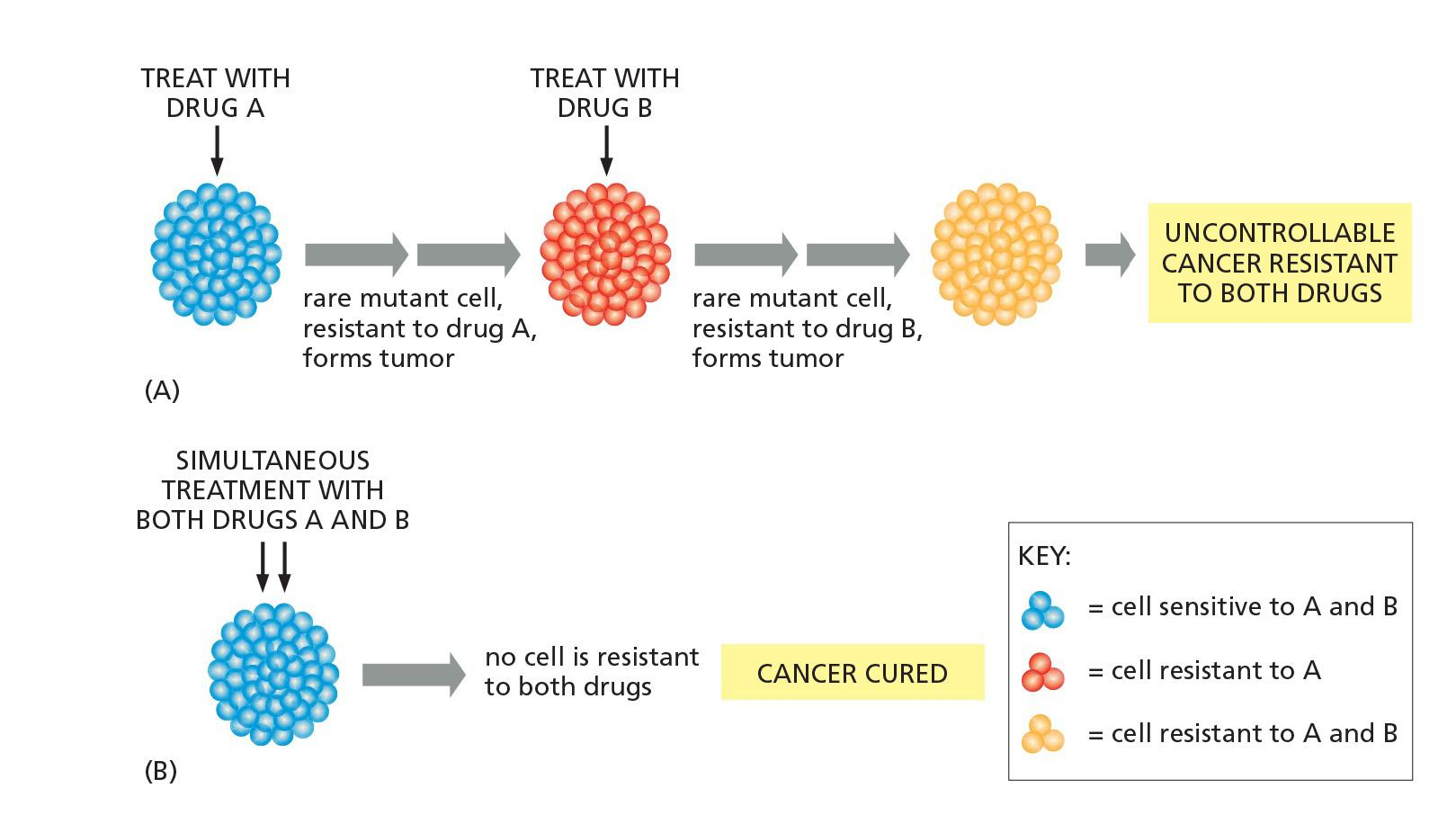
- Multidrug treatments can be more effective than sequential treatments for cancer therapy
1. Combination therapies tailored to the individual patient (personalized medicine)
- Better understanding which genes are altered in the cells of any given tumor can help to tailor treatments more accurately to each individual patient.
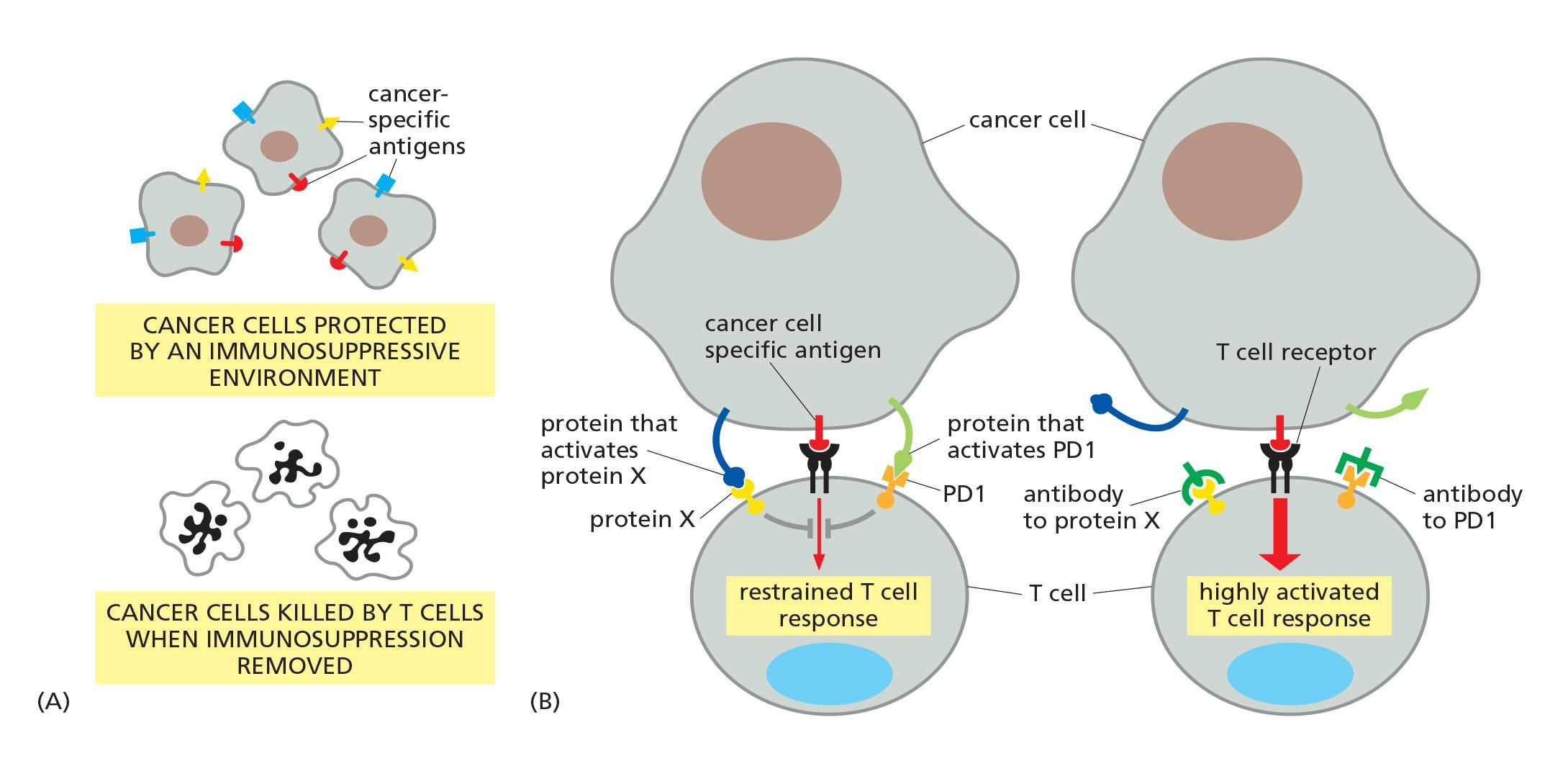
Cancer immunotherapy
Reactivation of immune system in cancer patients to inhibit cancer development
Two examples:
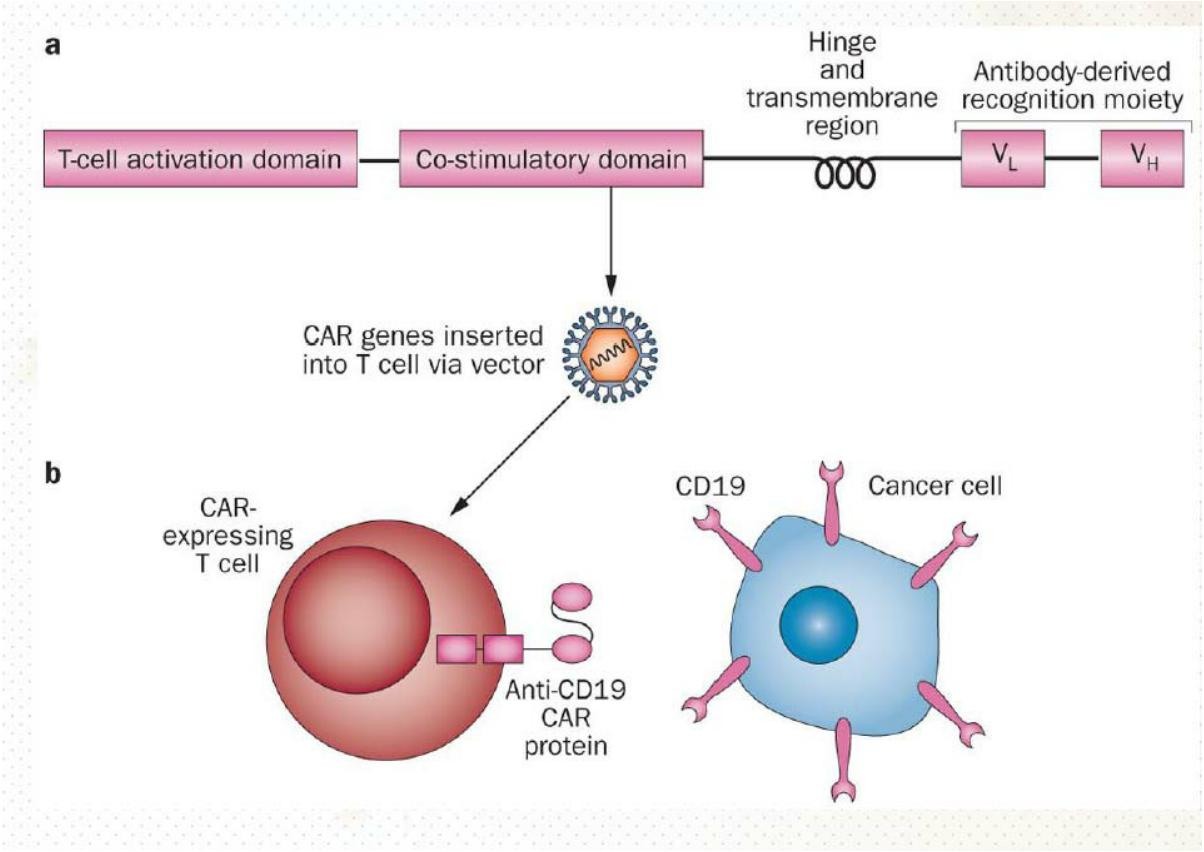
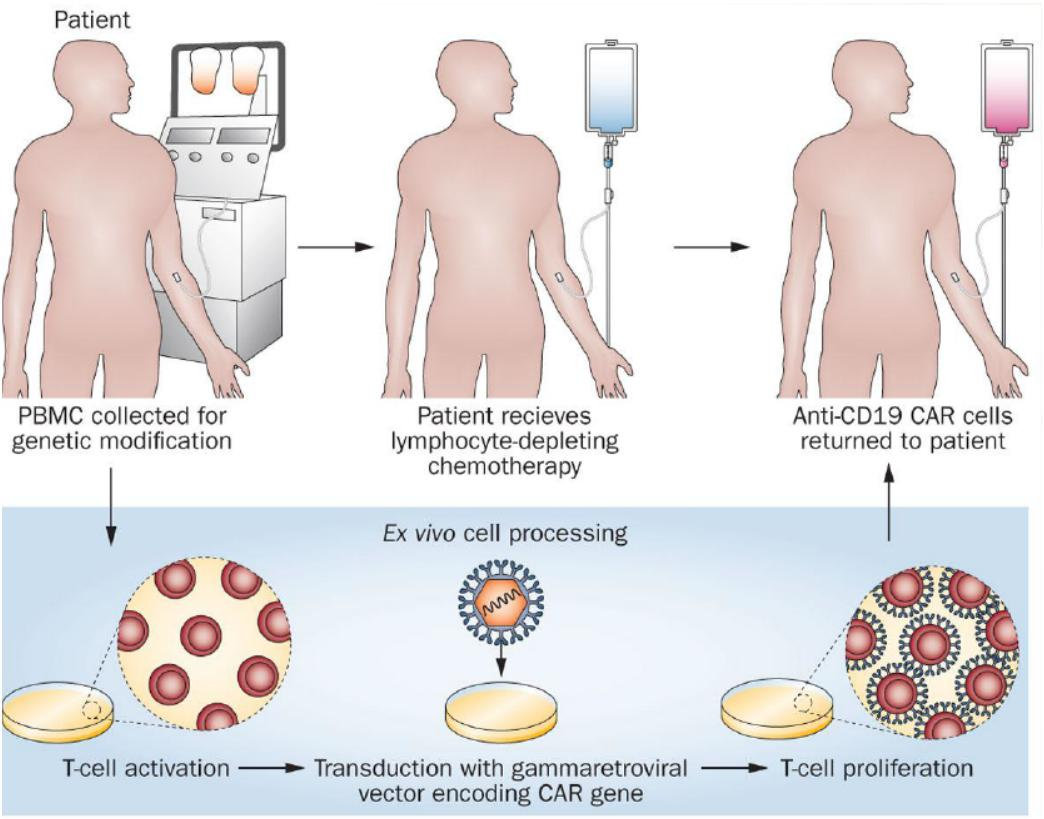
- CAR-T ( chimeric antigen receptor- T cell )
- Anti-PD1 antibody
Emily Whitehead: A young girl beats cancer with immunotherapy
- CD19-specific CAR-T cell therapy
- A case of how these cells cure acute lymphocytic leukemia (ALL)
- 03/2013, New England Journal of Medicine
- It was approved by FDA in August 2017.